Tension pneumothorax resident survival guide: Difference between revisions
| Line 76: | Line 76: | ||
{{familytree | | | | |!| | | | | }} | {{familytree | | | | |!| | | | | }} | ||
{{familytree | | | | B01 | | | | |B01= <div style="float: Left; text-align: left; width: 40em; padding:1em;">'''Examine the patient:'''<BR> | {{familytree | | | | B01 | | | | |B01= <div style="float: Left; text-align: left; width: 40em; padding:1em;">'''Examine the patient:'''<BR> | ||
'''Appearance of the patient'''<br> | |||
❑ Patient with [[tension pneumothorax]] is severely distressed with [[labored respirations]]. | |||
'''Vital signs'''<BR> | '''Vital signs'''<BR> | ||
❑ [[Pulse]]:<BR> | ❑ [[Pulse]]:<BR> | ||
:❑ [[Tachycardia]]<BR> | :❑ Rate | ||
:❑ | ::❑ [[Tachycardia]]<BR> | ||
❑ | :❑ Rhythm<br> | ||
:❑ | ::❑ Regular | ||
:❑ Strength | |||
::❑ Weak | |||
❑ [[Blood pressure]]<BR> | ❑ [[Blood pressure]]<BR> | ||
:❑ [[Hypotension]] <BR> | :❑ [[Hypotension]] <BR> | ||
❑ [[Respiratory rate]]<BR> | |||
:❑ [[Tachypnea]]<BR> | |||
'''Focused chest examination:'''<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref><BR> | '''Focused chest examination:'''<ref name="pmid20696690">{{cite journal| author=MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group| title=Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. | journal=Thorax | year= 2010 | volume= 65 Suppl 2 | issue= | pages= ii18-31 | pmid=20696690 | doi=10.1136/thx.2010.136986 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20696690 }} </ref><BR> | ||
| Line 91: | Line 97: | ||
❑ Enlarged involved [[Thorax|hemithorax]]<BR> | ❑ Enlarged involved [[Thorax|hemithorax]]<BR> | ||
❑ [[Jugular venous distension]] (absent in severe [[hypotension]])<BR> | ❑ [[Jugular venous distension]] (absent in severe [[hypotension]])<BR> | ||
❑ [[Intercostal space]] widening on the affected hemithorax<br> | |||
'''Palpation'''<BR> | '''Palpation'''<BR> | ||
❑ Reduced [[lung expansion]] on the affected side <BR> | ❑ Reduced [[lung expansion]] on the affected side <BR> | ||
Revision as of 19:59, 24 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohamed Moubarak, M.D. [2]
Synonyms and keywords: Collapsed lung; air around the lung; air outside the lung
| Tension Pneumothorax Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Tension pneumothorax is a medical emergency resulting from accumulation of air in the pleural cavity. Air enters the intrapleural space as a result of disruption in the parietal pleura, visceral pleura or tracheobronchial tree, this disruption results in the formation of a one way valve which allows the air to enter in the pleural cavity (during inspiration) but prevents its escape (during expiration). Subsequently, pressure inside the pleural cavity rises high enough to cause respiratory and cardiovascular failure. Tension pneumothorax can occur as a result of trauma, ventilation, resuscitation and preexisting lung disease.[1] It should be managed immediately with emergency needle decompression.
Causes
Life Threatening Causes
Tension pneumothorax is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
Tension pneumothorax can be a complication of primary, or secondary pneumothorax. The most common causes of tension pneumothorax are:
- Mechanical ventilation
- Trauma
- Central venous catheter
- Cardiopulmonary resuscitation
- Emphysema
- Chronic obstructive pulmonary disease
- Asthma
Diagnosis
Shown below is an algorithm depicting the diagnostic approach of tension pneumothorax based on the British Thoracic Society Pleural Disease Guideline 2010.[1]
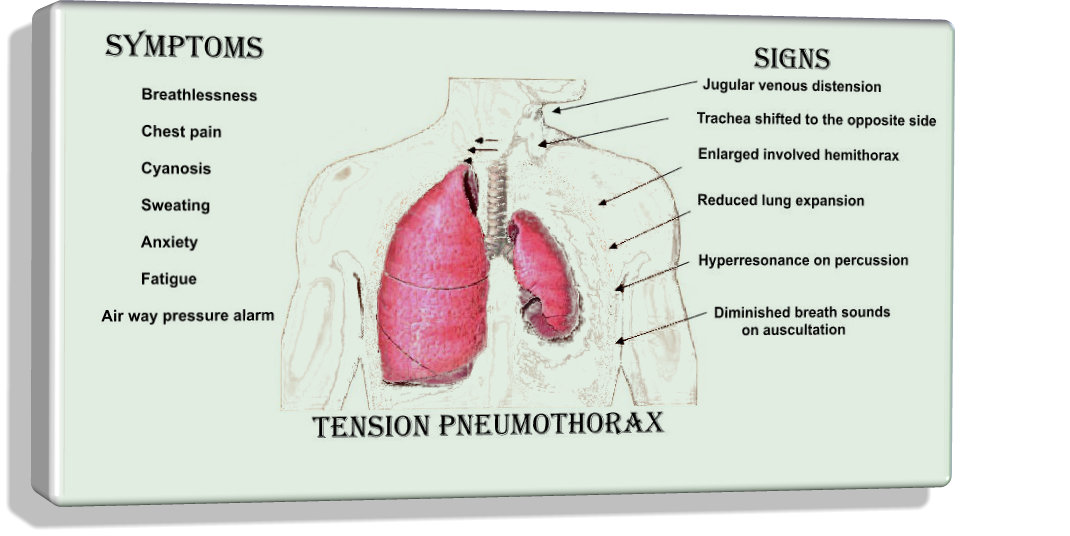
Characterize the symptoms:[1] Tension pneumothorax requires immediate intervention. It should be diagnosed based on the history and physical examination findings. ❑ Dyspnoea | |||||||||||||||||||||||||||
Identify the precipitating factors: (Diagnosis of pneumothorax is more likely if any of the following is present) ❑ Mechanical ventilation | |||||||||||||||||||||||||||
Examine the patient: Appearance of the patient
Inspection Percussion Auscultation Additional findings in ventilated patients: | |||||||||||||||||||||||||||
Rule out the following alternative diagnosis clinically: | |||||||||||||||||||||||||||
| Stable patient | Unstable patient | ||||||||||||||||||||||||||
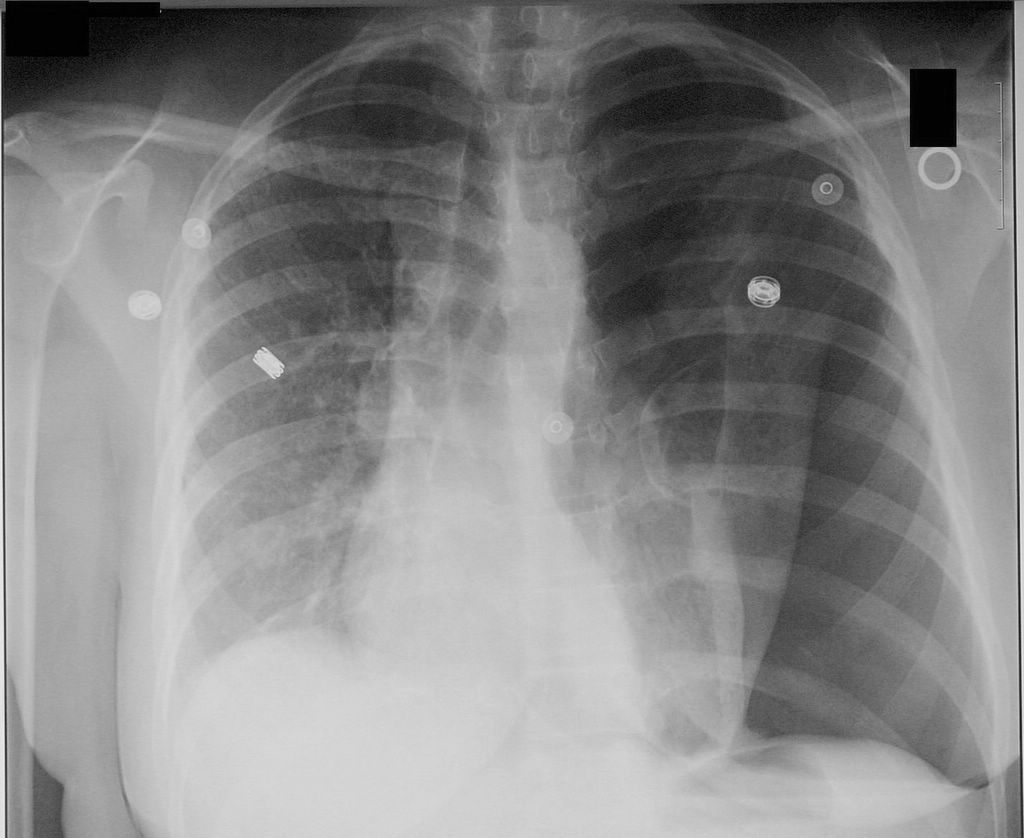
❑ Proceed with imaging studies to confirm the diagnosis Imaging studies:
❑ Chest CT scanning
| ❑ Administer high concentration oxygen ❑ Perform emergent needle decompression (14-16 G) | ||||||||||||||||||||||||||
Treatment
Shown below is an algorithm depicting the treatment approach to tension pneumothorax based on the British Thoracic Society Pleural Disease Guideline 2010.[1]
Initial supportive measures: (In cases of chest wall trauma) | |||||||||||||||||||||||||||||||||||||
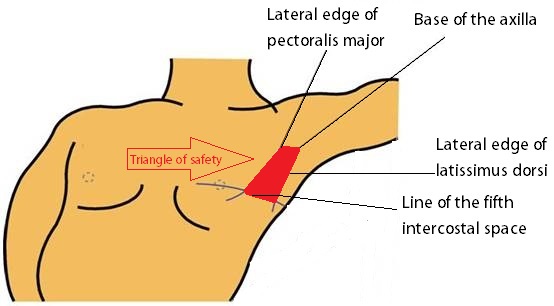
Emergency needle decompression:
❑ Aseptic preparation
❑ Use 14-16 G intravenous cannula
❑ Listen for gush of air | |||||||||||||||||||||||||||||||||||||
| Admit the patient | |||||||||||||||||||||||||||||||||||||
Insert chest drain ❑ Obtain the informed consent
❑ Ensure asepsis
❑ Site
❑ Insert the chest tube
❑ Intrapleural infection
| |||||||||||||||||||||||||||||||||||||
Discharge and follow up ❑ All patients should be followed up by respiratory physicians | |||||||||||||||||||||||||||||||||||||
Do`s
- Tension pneumothorax diagnosis should be made based on the history and physical examination findings.
- Serial chest radiographs every 6 hrs on the first day after injury to rule out pneumothorax is ideal.[2]
- Leave the cannula in place until bubbling is confirmed in the chest drain underwater seal system
- Suspect tension pneumothorax with blunt and penetrating trauma to the chest
- Differentiate tension pneumothorax from pericardial tamponade, and myocardial infarction.
- Suspect tension pneumothorax in patients on mechanical ventilations, who have a rapid onset of hemodynamic instability or cardiac arrest, and require increasing peak inspiratory pressures.
- Check chest tubes, as they can become plugged or malpositioned and stop functioning.
- Give adequate analgesia to patients before chest tube insertion, as the procedure is extremely painful.
- Refer the patient to respiratory specialist within 24h of admission.
Dont`s
- Don`t start using chest radiograph or CT scan unless in doubt regarding the diagnosis and when the patient's clinical condition is sufficiently stable.
- Don`t use large bore chest drains.[1]
- Don`t repeat needle aspiration unless there were technical difficulties.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 MacDuff A, Arnold A, Harvey J, BTS Pleural Disease Guideline Group (2010). "Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010". Thorax. 65 Suppl 2: ii18–31. doi:10.1136/thx.2010.136986. PMID 20696690.
- ↑ 2.0 2.1 2.2 Sharma A, Jindal P (2008). "Principles of diagnosis and management of traumatic pneumothorax". J Emerg Trauma Shock. 1 (1): 34–41. doi:10.4103/0974-2700.41789. PMC 2700561. PMID 19561940.