Telithromycin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ammu Susheela, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Boxed Warning
See full prescribing information for complete Boxed Warning.
* Ketek is contraindicated in patients with myasthenia gravis. There have been reports of fatal and life-threatening respiratory failure in patients with myasthenia gravis associated with the use of Ketek.
|
Overview
Telithromycin is a antibiotic that is FDA approved for the treatment of community-acquired pneumonia (of mild to moderate severity) due to Streptococcus pneumoniae, (including multi-drug resistant isolates [MDRSP3]), Haemophilus influenzae, Moraxella catarrhalis, Chlamydophila pneumoniae, or Mycoplasma pneumoniae, for patients 18 years old and above. There is a Black Box Warning for this drug as shown here. Common adverse reactions include diarrhea, nausea, vomiting, dizziness, headache, abnormal vision , blurred vision, diplopia, problem of visual accommodation.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- KETEK tablets are indicated for the treatment of community-acquired pneumonia (of mild to moderate severity) due to Streptococcus pneumoniae, (including multi-drug resistant isolates [MDRSP3]), Haemophilus influenzae, Moraxella catarrhalis, Chlamydophila pneumoniae, or Mycoplasma pneumoniae, for patients 18 years old and above.
- To reduce the development of drug-resistant bacteria and maintain the effectiveness of KETEK and other antibacterial drugs, KETEK should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
- 3 MDRSP, Multi-drug resistant Streptococcus pneumoniae includes isolates known as PRSP (penicillin-resistant Streptococcus pneumoniae), and are isolates resistant to two or more of the following antibiotics: penicillin, 2 nd generation cephalosporins, e.g., cefuroxime, macrolides, tetracyclines and trimethoprim/sulfamethoxazole.
- The dose of KETEK tablets is 800 mg (2 tablets of 400 mg) taken orally once every 24 hours, for 7–10 days. KETEK tablets can be administered with or without food.
- KETEK may be administered without dosage adjustment in the presence of hepatic impairment.
- In the presence of severe renal impairment (CLCR < 30 mL/min), including patients who need dialysis, the dose should be reduced to KETEK 600 mg once daily. In patients undergoing hemodialysis, KETEK should be given after the dialysis session on dialysis days.
- In the presence of severe renal impairment (CLCR < 30 mL/min), with coexisting hepatic impairment, the dose should be reduced to KETEK 400 mg once daily.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Telithromycin in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Telithromycin in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Telithromycin in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Telithromycin in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Telithromycin in pediatric patients.
Contraindications
- KETEK is contraindicated in patients with myasthenia gravis. Exacerbations of myasthenia gravis have been reported in patients and sometimes occurred within a few hours of the first dose of telithromycin. Reports have included fatal and life-threatening acute respiratory failure with a rapid onset and progression.
- KETEK is contraindicated in patients with previous history of hepatitis and/or jaundice associated with the use of KETEK tablets, or any macrolide antibiotic.
- KETEK is contraindicated in patients with a history of hypersensitivity to telithromycin and/or any components of KETEK tablets, or any macrolide antibiotic.
- Concomitant administration of KETEK with cisapride or pimozide is contraindicated.
- Concomitant administration of KETEK and colchicine is contraindicated in patients with renal or hepatic impairment.
Warnings
|
Boxed Warning
See full prescribing information for complete Boxed Warning.
* Ketek is contraindicated in patients with myasthenia gravis. There have been reports of fatal and life-threatening respiratory failure in patients with myasthenia gravis associated with the use of Ketek.
|
Hepatotoxicity
- Acute hepatic failure and severe liver injury, in some cases fatal, have been reported in patients treated with KETEK. These hepatic reactions included fulminant hepatitis and hepatic necrosis leading to liver transplant, and were observed during or immediately after treatment. In some of these cases, liver injury progressed rapidly and occurred after administration of a few doses of KETEK.
- Physicians and patients should monitor for the appearance of signs or symptoms of hepatitis, such as fatigue, malaise, anorexia, nausea, jaundice, bilirubinuria, acholic stools, liver tenderness or hepatomegaly. Patients with signs or symptoms of hepatitis must be advised to discontinue KETEK and immediately seek medical evaluation, which should include liver function tests. If clinical hepatitis or transaminase elevations combined with other systemic symptoms occur, KETEK should be permanently discontinued.
- Ketek must not be re-administered to patients with a previous history of hepatitis and/or jaundice associated with the use of KETEK tablets, or any macrolide antibiotic.
- In addition, less severe hepatic dysfunction associated with increased liver enzymes, hepatitis and in some cases jaundice was reported with the use of KETEK. These events associated with less severe forms of liver toxicity were reversible.
QTc prolongation
- Telithromycin has the potential to prolong the QTc interval of the electrocardiogram in some patients. QTc prolongation may lead to an increased risk for ventricular arrhythmias, including torsades de pointes. Thus, telithromycin should be avoided in patients with congenital prolongation of the QTc interval, and in patients with ongoing proarrhythmic conditions such as uncorrected hypokalemia or hypomagnesemia, clinically significant bradycardia, and in patients receiving Class IA (e.g., quinidine and procainamide) or Class III (e.g., dofetilide) antiarrhythmic agents.
- Cases of torsades de pointes have been reported post-marketing with KETEK. In clinical trials, no cardiovascular morbidity or mortality attributable to QTc prolongation occurred with telithromycin treatment in 4780 patients in clinical trials, including 204 patients having a prolonged QTc at baseline.
Visual disturbances
- KETEK may cause visual disturbances particularly in slowing the ability to accommodate and the ability to release accommodation. Visual disturbances included blurred vision, difficulty focusing, and diplopia. Most events were mild to moderate; however, severe cases have been reported.
Loss of Consciousness
- There have been post-marketing adverse event reports of transient loss of consciousness including some cases associated with vagal syndrome.
- Because of potential visual difficulties or loss of consciousness, patients should attempt to minimize activities such as driving a motor vehicle, operating heavy machinery or engaging in other hazardous activities during treatment with KETEK. If patients experience visual disorders or loss of consciousness while taking KETEK, patients should not drive a motor vehicle, operate heavy machinery or engage in other hazardous activities.
Drug Interactions
- Serious adverse reactions have been reported in patients taking KETEK concomitantly with CYP 3A4 substrates. These include colchicine toxicity with colchicine; rhabdomyolysis with simvastatin, lovastatin, and atorvastatin; and hypotension with calcium channel blockers metabolized by CYP 3A4 (e.g., verapamil, amlodipine, diltiazem). (See PRECAUTIONS, DRUG INTERACTIONS.)
- Life-threatening and fatal drug interactions have been reported in patients treated with colchicine and strong CYP 3A4 inhibitors. Telithromycin is a strong CYP 3A4 inhibitor and this interaction may occur while using both drugs at their recommended doses. If co-administration of telithromycin and colchicine is necessary in patients with normal renal and hepatic function, the dose of colchicine should be reduced. Patients should be monitored for clinical symptoms of colchicine toxicity. Concomitant administration of KETEK and colchicine is contraindicated in patients with renal or hepatic impairment.
Pseudomembranous Colitis
- Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including KETEK, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
- C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
- If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C difficile, and surgical evaluation should be instituted as clinically indicated.
Adverse Reactions
Clinical Trials Experience
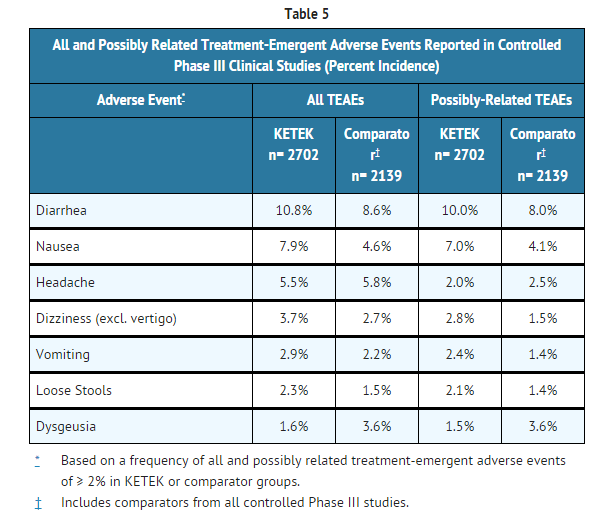
- In Phase III clinical trials, 4,780 patients (n=2702 in controlled trials) received daily oral doses of KETEK 800 mg once daily for 5 days or 7 to 10 days. Most adverse events were mild to moderate in severity. In the combined Phase III studies, discontinuation due to treatment-emergent adverse events occurred in 4.4% of KETEK-treated patients and 4.3% of combined comparator-treated patients. Most discontinuations in the KETEK group were due to treatment-emergent adverse events in the gastrointestinal body system, primarily diarrhea (0.9% for KETEK vs. 0.7% for comparators), nausea (0.7% for KETEK vs. 0.5% for comparators).
- All and possibly related treatment-emergent adverse events (TEAEs) occurring in controlled clinical studies in ≥ 2.0% of all patients are included below:
- The following events judged by investigators to be at least possibly drug related were observed infrequently (≥ 0.2% and < 2%), in KETEK-treated patients in the controlled Phase III studies.
- Gastrointestinal system
- Abdominal distension, dyspepsia, gastrointestinal upset, flatulence, constipation, gastroenteritis, gastritis, anorexia, oral candidiasis, glossitis, stomatitis, watery stools.
- Liver and biliary system
- Abnormal liver function tests: increased transaminases, increased liver enzymes (e.g., ALT, AST) were usually asymptomatic and reversible. ALT elevations above 3 times the upper limit of normal were observed in 1.6%, and 1.7% of patients treated with KETEK and comparators, respectively. Hepatitis, with or without jaundice, occurred in 0.07% of patients treated with KETEK, and was reversible.
- Nervous system
- Dry mouth, somnolence, insomnia, vertigo, increased sweating
- Body as a whole
- Abdominal pain, upper abdominal pain, fatigue
- Special senses
- Visual adverse events most often included blurred vision, diplopia, or difficulty focusing. Most events were mild to moderate; however, severe cases have been reported. Some patients discontinued therapy due to these adverse events. Visual adverse events were reported as having occurred after any dose during treatment, but most visual adverse events (65%) occurred following the first or second dose. Visual events lasted several hours and recurred upon subsequent dosing in some patients. For patients who continued treatment, some resolved on therapy while others continued to have symptoms until they completed the full course of treatment.
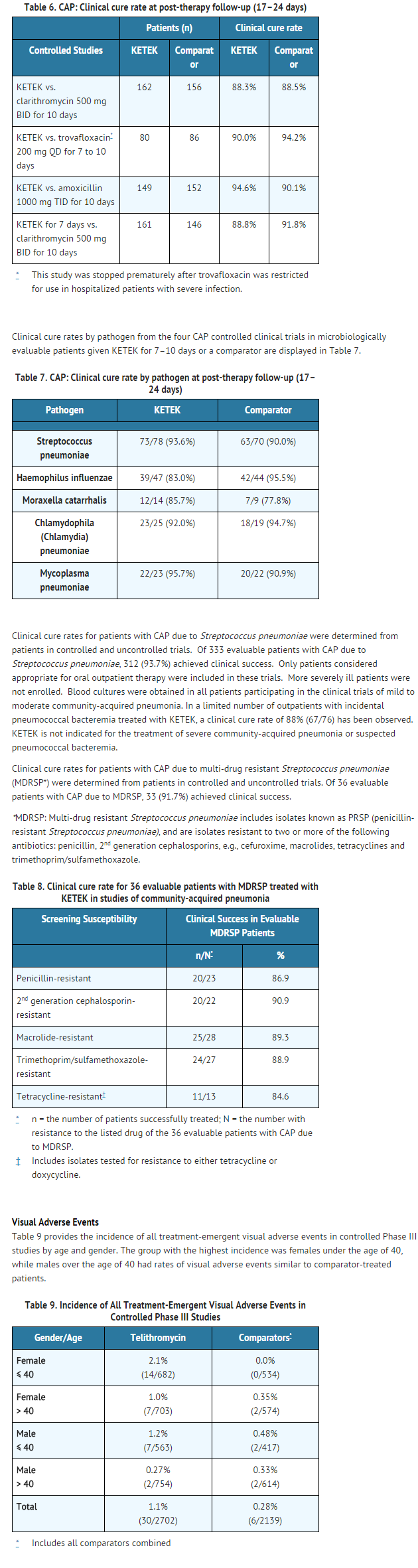
- Females and patients under 40 years old experienced a higher incidence of telithromycin-associated visual adverse events. (See CLINICAL STUDIES.)
- Urogenital system
- Vaginal candidiasis, vaginitis, vaginosis fungal
- Skin
- Hematologic
- Increased platelet count
- Other possibly related clinically-relevant events occurring in <0.2% of patients treated with KETEK from the controlled Phase III studies included: anxiety, bradycardia, eczema, elevated blood bilirubin, erythema multiforme, flushing, hypotension, increased blood alkaline phosphatase, increased eosinophil count, paresthesia, pruritus, urticaria.
Postmarketing Experience
- In addition to adverse events reported from clinical trials, the following events have been reported from worldwide post-marketing experience with KETEK.
- Allergic
- Face edema, rare reports of severe allergic (hypersensitivity) reactions, including angioedema and anaphylaxis
- Cardiovascular
- Atrial arrhythmias, palpitations
- Gastrointestinal system
- Pancreatitis
- Liver and biliary system
- Hepatic dysfunction has been reported.
- Severe and in some cases fatal hepatotoxicity, including fulminant hepatitis, hepatic necrosis and hepatic failure have been reported in patients treated with KETEK. These hepatic reactions were observed during or immediately after treatment. In some of these cases, liver injury progressed rapidly and occurred after administration of only a few doses of KETEK. (See CONTRAINDICATIONS and WARNINGS.) Severe reactions, in some but not all cases, have been associated with serious underlying diseases or concomitant medications.
- Data from post-marketing reports and clinical trials show that most cases of hepatic dysfunction were mild to moderate. (See PRECAUTIONS, GENERAL.)
- Musculoskeletal
- Muscle cramps, rare reports of exacerbation of myasthenia gravis. Arthralgia, myalgia
- Nervous system
- Loss of consciousness, in some cases associated with vagal syndrome.
- Psychiatric disorders
- Confusion, hallucinations (mostly visual)
- Special senses
- Taste/smell perversion and/or loss
Drug Interactions
In vitro interactions
- In vitro studies using a model compound have shown that telithromycin may act as an inhibitor for the hepatic uptake transporters OATP1B1 and OATP1B3. Although the clinical relevance of this finding is unknown, it is possible that concomitant administration of telithromycin with drugs that are substrates of OATP family members could result in increased plasma concentrations of the co-administered drug.
In vivo interactions
- Studies were performed to evaluate the effect of CYP 3A4 inhibitors on telithromycin and the effect of telithromycin on drugs that are substrates of CYP 3A4 and CYP 2D6. In addition, drug interaction studies were conducted with several other concomitantly prescribed drugs.
CYP 3A4 inhibitors
Itraconazole
- A multiple-dose interaction study with itraconazole showed that Cmax of telithromycin was increased by 22% and AUC by 54%.
Ketoconazole
- A multiple-dose interaction study with ketoconazole showed that Cmax of telithromycin was increased by 51% and AUC by 95%.
Grapefruit juice
- When telithromycin was given with 240 mL of grapefruit juice after an overnight fast to healthy subjects, the pharmacokinetics of telithromycin were not affected.
CYP 3A4 substrates
Cisapride
- Steady-state peak plasma concentrations of cisapride (an agent with the potential to increase QT interval) were increased by 95% when co-administered with repeated doses of telithromycin, resulting in significant increases in QTc.
Simvastatin
- When simvastatin was co-administered with telithromycin, there was a 5.3-fold increase in simvastatin Cmax, an 8.9-fold increase in simvastatin AUC, a 15-fold increase in the simvastatin active metabolite Cmax, and a 12-fold increase in the simvastatin active metabolite AUC. (See PRECAUTIONS)
- In another study, when simvastatin and telithromycin were administered 12 hours apart, there was a 3.4-fold increase in simvastatin Cmax, a 4.0-fold increase in simvastatin AUC, a 3.2-fold increase in the active metabolite Cmax, and a 4.3-fold increase in the active metabolite AUC. (See PRECAUTIONS)
Midazolam
- Concomitant administration of telithromycin with intravenous or oral midazolam resulted in 2- and 6-fold increases, respectively, in the AUC of midazolam due to inhibition of CYP 3A4-dependent metabolism of midazolam.
CYP 2D6 substrates
Paroxetine
- There was no pharmacokinetic effect on paroxetine when telithromycin was co-administered.
Metoprolol
- When metoprolol was co-administered with telithromycin, there was an increase of approximately 38% on the Cmax and AUC of metoprolol, however, there was no effect on the elimination half-life of metoprolol. Telithromycin exposure is not modified with concomitant single-dose administration of metoprolol.
Other drug interactions
Digoxin
- The plasma peak and trough levels of digoxin were increased by 73% and 21%, respectively, in healthy volunteers when co-administered with telithromycin. However, trough plasma concentrations of digoxin (when equilibrium between plasma and tissue concentrations has been achieved) ranged from 0.74 to 2.17 ng/mL. There were no significant changes in ECG parameters and no signs of digoxin toxicity.
Theophylline
- When theophylline was co-administered with repeated doses of telithromycin, there was an increase of approximately 16% and 17% on the steady-state Cmax and AUC of theophylline. Co-administration of theophylline may worsen gastrointestinal side effects such as nausea and vomiting, especially in female patients. It is recommended that telithromycin should be taken with theophylline 1 hour apart to decrease the likelihood of gastrointestinal side effects.
Sotalol
- Telithromycin has been shown to decrease the Cmax and AUC of sotalol by 34% and 20%, respectively, due to decreased absorption.
Warfarin
- When co-administered with telithromycin in healthy subjects, there were no pharmacodynamic or pharmacokinetic effects on racemic warfarin.
Oral contraceptives
- When oral contraceptives containing ethinyl estradiol and levonorgestrel were co-administered with telithromycin, the steady-state AUC of ethinyl estradiol did not change and the steady-state AUC of levonorgestrel was increased by 50%. The pharmacokinetic/pharmacodynamic study showed that telithromycin did not interfere with the antiovulatory effect of oral contraceptives containing ethinyl estradiol and levonorgestrel.
Ranitidine
- There was no clinically relevant pharmacokinetic interaction of ranitidine or antacids containing aluminum and magnesium hydroxide on telithromycin.
Rifampin
- During concomitant administration of rifampin and KETEK in repeated doses, Cmax and AUC of telithromycin were decreased by 79%, and 86%, respectively.
Use in Specific Populations
Pregnancy
- Telithromycin was not teratogenic in the rat or rabbit. Reproduction studies have been performed in rats and rabbits, with effect on pre-post natal development studied in the rat. At doses estimated to be 1.8 times (900 mg/m2) and 0.49 times (240 mg/m2) the daily human dose of 800 mg (492 mg/m2) in the rat and rabbit, respectively, no evidence of fetal terata was found. At doses higher than the 900 mg/m2 and 240 mg/m2 in rats and rabbits, respectively, maternal toxicity may have resulted in delayed fetal maturation. No adverse effects on prenatal and postnatal development of rat pups were observed at 1.5 times (750 mg/m2/d) the daily human dose.
- There are no adequate and well-controlled studies in pregnant women. Telithromycin should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Telithromycin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Telithromycin during labor and delivery.
Nursing Mothers
- Telithromycin is excreted in breast milk of rats. Telithromycin may also be excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when KETEK is administered to a nursing mother.
Pediatric Use
There is no FDA guidance on the use of Telithromycin with respect to pediatric patients.
Geriatic Use
- In all Phase III clinical trials (n=4,780), KETEK was administered to 694 patients who were 65 years and older, including 231 patients who were 75 years and older. Efficacy and safety in elderly patients ≥ 65 years were generally similar to that observed in younger patients; however, greater sensitivity of some older individuals cannot be ruled out. No dosage adjustment is required based on age alone.
Gender
- There was no significant difference between males and females in mean AUC, Cmax, and elimination half-life in two studies; one in 18 healthy young volunteers (18 to 40 years of age) and the other in 14 healthy elderly volunteers (65 to 92 years of age), given single and multiple once daily doses of 800 mg of KETEK.
Race
There is no FDA guidance on the use of Telithromycin with respect to specific racial populations.
Renal Impairment
- In a multiple-dose study, 36 subjects with varying degrees of renal impairment received 400 mg, 600 mg, or 800 mg KETEK once daily for 5 days. There was a 1.4-fold increase in Cmax,ss, and a 1.9-fold increase in AUC (0–24)ss at 800 mg multiple doses in the severely renally impaired group (CLCR < 30 mL/min) compared to healthy volunteers. Renal excretion may serve as a compensatory elimination pathway for telithromycin in situations where metabolic clearance is impaired. Patients with severe renal impairment are prone to conditions that may impair their metabolic clearance. Therefore, in the presence of severe renal impairment (CLCR < 30 mL/min), a reduced dosage of KETEK is recommended.
Hepatic Impairment
- In a single-dose study (800 mg) in 12 patients and a multiple-dose study (800 mg) in 13 patients with mild to severe hepatic insufficiency (Child Pugh Class A, B and C), the Cmax, AUC and t1/2 of telithromycin were similar to those obtained in age- and sex-matched healthy subjects. In both studies, an increase in renal elimination was observed in hepatically impaired patients indicating that this pathway may compensate for some of the decrease in metabolic clearance. No dosage adjustment is recommended due to hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Telithromycin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Telithromycin in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral.
Monitoring
- Physicians and patients should monitor for the appearance of signs or symptoms of hepatitis, such as fatigue, malaise, anorexia, nausea, jaundice, bilirubinuria, acholic stools, liver tenderness or hepatomegaly
- Patients concomitantly treated with statins should be carefully monitored for signs and symptoms of myopathy and rhabdomyolysis.
- Monitoring of digoxin side effects or serum levels should be considered during concomitant administration of digoxin and KETEK.
- Monitoring of digoxin side effects or serum levels should be considered during concomitant administration of digoxin and KETEK.
IV Compatibility
There is limited information regarding IV Compatibility of Telithromycin in the drug label.
Overdosage
- In the event of acute overdosage, the stomach should be emptied by gastric lavage. The patient should be carefully monitored (e.g., ECG, electrolytes) and given symptomatic and supportive treatment. Adequate hydration should be maintained. The effectiveness of hemodialysis in an overdose situation with KETEK is unknown.
Pharmacology
There is limited information regarding Telithromycin Pharmacology in the drug label.
Mechanism of Action
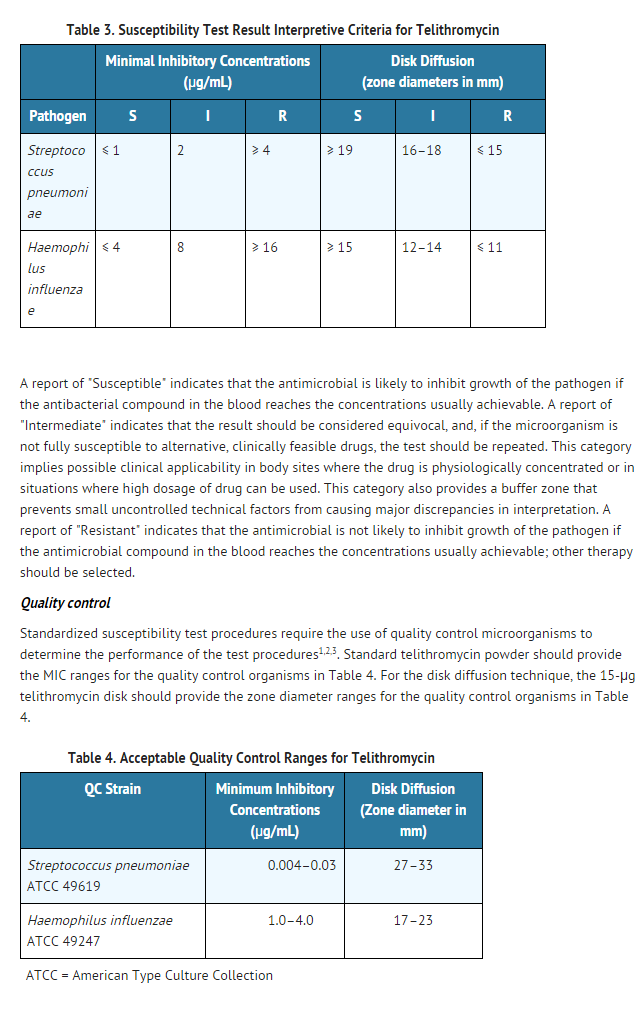
- Telithromycin blocks protein synthesis by binding to domains II and V of 23S rRNA of the 50S ribosomal subunit. By binding at domain II, telithromycin retains activity against gram-positive cocci (e.g., Streptococcus pneumoniae) in the presence of resistance mediated by methylases (erm genes) that alter the domain V binding site of telithromycin. Telithromycin may also inhibit the assembly of nascent ribosomal units.
Mechanism of Resistance
- Staphylococcus aureus and Streptococcus pyogenes with the constitutive macrolide-lincosamide-streptogramin B (cMLSB) phenotype are resistant to telithromycin.
- Mutants of Streptococcus pneumoniae derived in the laboratory by serial passage in subinhibitory concentrations of telithromycin have demonstrated resistance based on L22 riboprotein mutations (telithromycin MICs are elevated but still within the susceptible range), one of two reported mutations affecting the L4 riboprotein, and production of K-peptide. The clinical significance of these laboratory mutants is not known.
Cross Resistance
- Telithromycin does not induce resistance through methylase gene expression in erythromycin-inducibly resistant bacteria, a function of its 3-keto moiety. Telithromycin has not been shown to induce resistance to itself.
List of Microorganisms
- Telithromycin has been shown to be active against most strains of the following microorganisms.
- Aerobic gram-positive microorganisms
- Streptococcus pneumoniae (including multi-drug resistant isolates [MDRSP2])
- Aerobic gram-negative microorganisms
- Haemophilus influenzae
- Moraxella catarrhalis
- Other microorganisms
- Chlamydophila (Chlamydia) pneumoniae
- Mycoplasma pneumoniae
- The following in vitro data are available, but their clinical significance is unknown.
- At least 90% of the following microorganisms exhibit in vitro minimum inhibitory concentrations (MICs) less than or equal to the susceptible breakpoint for telithromycin. However, the safety and efficacy of telithromycin in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled clinical trials.
Aerobic gram-positive microorganisms
- Staphylococcus aureus (methicillin and erythromycin susceptible isolates only)
- Streptococcus pyogenes (erythromycin susceptible isolates only)
- Streptococci (Lancefield groups C and G)
Other microorganisms
- Legionella pneumophila
- 2 MDRSP=Multi-drug resistant Streptococcus pneumoniae includes isolates known as PRSP (penicillin-resistant S. pneumoniae), and are isolates resistant to two or more of the following antimicrobials: penicillin, 2 nd generation cephalosporins (e.g., cefuroxime), macrolides, tetracyclines, and trimethoprim/sulfamethoxazole.
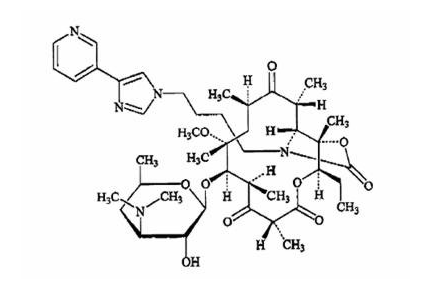
Structure
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Telithromycin in the drug label.
Pharmacokinetics
Absorption
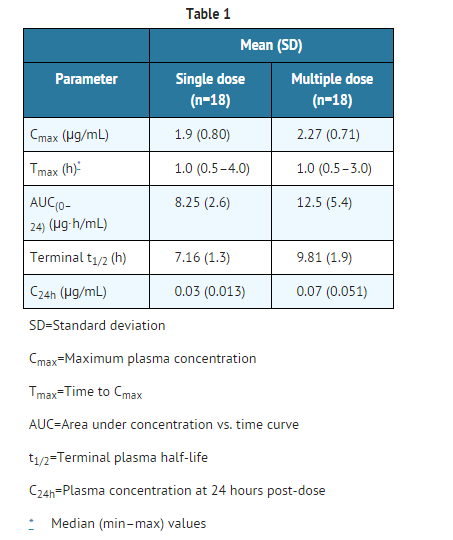
- Following oral administration, telithromycin reached maximal concentration at about 1 hour (0.5 – 4 hours).
- It has an absolute bioavailability of 57% in both young and elderly subjects.
- The rate and extent of absorption are unaffected by food intake, thus KETEK tablets can be given without regard to food.
- In healthy adult subjects, peak plasma telithromycin concentrations of approximately 2 µg/mL are attained at a median of 1 hour after an 800-mg oral dose.
- Steady-state plasma concentrations are reached within 2 to 3 days of once daily dosing with telithromycin 800 mg.
- Following oral dosing, the mean terminal elimination half-life of telithromycin is 10 hours.
- The pharmacokinetics of telithromycin after administration of single and multiple (7 days) once daily 800-mg doses to healthy adult subjects are shown in Table 1.
- Telithromycin concentration in white blood cells exceeds the concentration in plasma and is eliminated more slowly from white blood cells than from plasma. Mean white blood cell concentrations of telithromycin peaked at 72.1 µg/mL at 6 hours, and remained at 14.1 µg/mL 24 hours after 5 days of repeated dosing of 600 mg once daily. After 10 days, repeated dosing of 600 mg once daily, white blood cell concentrations remained at 8.9 µg/mL 48 hours after the last dose.
Metabolism
- In total, metabolism accounts for approximately 70% of the dose. In plasma, the main circulating compound after administration of an 800-mg radio-labeled dose was parent compound, representing 56.7% of the total radioactivity. The main metabolite represented 12.6% of the AUC of telithromycin. Three other plasma metabolites were quantified, each representing 3% or less of the AUC of telithromycin.
- It is estimated that approximately 50% of its metabolism is mediated by CYP 450 3A4 and the remaining 50% is CYP 450-independent.
Elimination
- The systemically available telithromycin is eliminated by multiple pathways as follows: 7% of the dose is excreted unchanged in feces by biliary and/or intestinal secretion; 13% of the dose is excreted unchanged in urine by renal excretion; and 37% of the dose is metabolized by the liver.
Nonclinical Toxicology
There is limited information regarding Nonclinical Toxicology of Telithromycin in the drug label.
Clinical Studies
Community-acquired pneumonia (CAP)
- KETEK was studied in four randomized, double-blind, controlled studies and four open-label studies for the treatment of community-acquired pneumonia. Patients with mild to moderate CAP who were considered appropriate for oral outpatient treatment were enrolled in these trials. Patients with severe pneumonia were excluded based on any one of the following: ICU admission, need for parenteral antibiotics, respiratory rate > 30/minute, hypotension, altered mental status, < 90% oxygen saturation by pulse oximetry, or white blood cell count < 4000/mm3. Total number of clinically evaluable patients in the telithromycin group included 2016 patients.
- Clinical cure rates for patients with CAP due to Streptococcus pneumoniae were determined from patients in controlled and uncontrolled trials. Of 333 evaluable patients with CAP due to Streptococcus pneumoniae, 312 (93.7%) achieved clinical success. Only patients considered appropriate for oral outpatient therapy were included in these trials. More severely ill patients were not enrolled. Blood cultures were obtained in all patients participating in the clinical trials of mild to moderate community-acquired pneumonia. In a limited number of outpatients with incidental pneumococcal bacteremia treated with KETEK, a clinical cure rate of 88% (67/76) has been observed. KETEK is not indicated for the treatment of severe community-acquired pneumonia or suspected pneumococcal bacteremia.
- Clinical cure rates for patients with CAP due to multi-drug resistant Streptococcus pneumoniae (MDRSP*) were determined from patients in controlled and uncontrolled trials. Of 36 evaluable patients with CAP due to MDRSP, 33 (91.7%) achieved clinical success.
- MDRSP: Multi-drug resistant Streptococcus pneumoniae includes isolates known as PRSP (penicillin-resistant Streptococcus pneumoniae), and are isolates resistant to two or more of the following antibiotics: penicillin, 2nd generation cephalosporins, e.g., cefuroxime, macrolides, tetracyclines and trimethoprim/sulfamethoxazole.
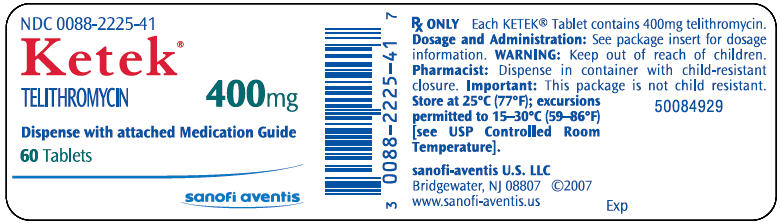
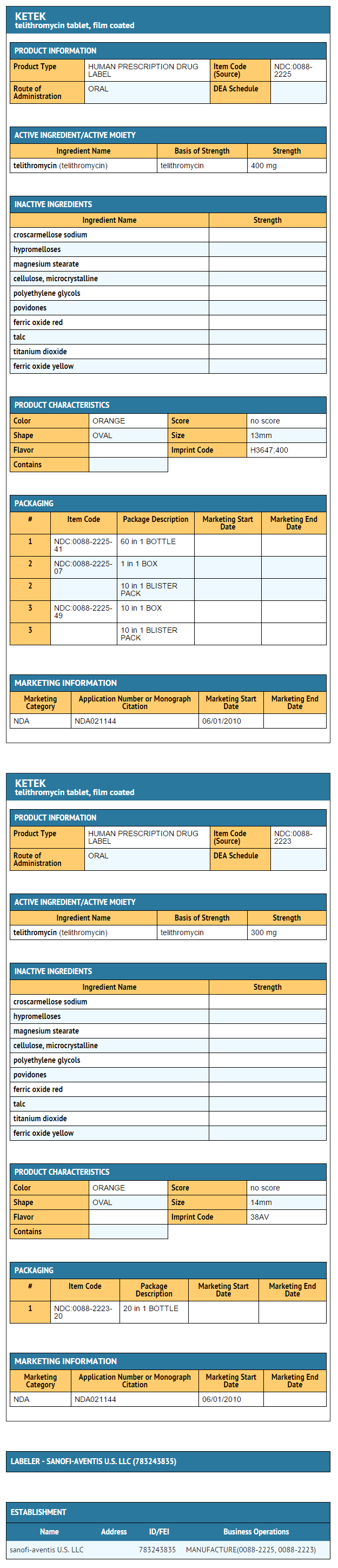
How Supplied
- KETEK® 400 mg tablets are supplied as light-orange, oval, film-coated tablets, imprinted "H3647" on one side and "400" on the other side. These are packaged in bottles as follows:
- Bottles of 60 :* (NDC 0088-2225-41)
- KETEK® 300 mg tablets are supplied as light-orange, oval, film-coated tablets, imprinted "38AV" on one side and blank on the other side. These are packaged in bottles as follows:
- Bottles of 20 :* (NDC 0088-2223-20)
Storage
- Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F)
Images
Drug Images
{{#ask: Page Name::Telithromycin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
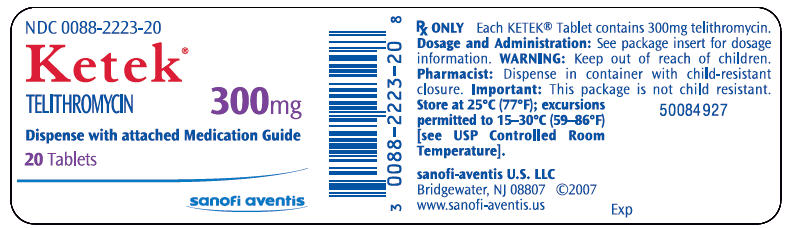
{{#ask: Label Page::Telithromycin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Patient Counseling Information of Telithromycin in the drug label.
Precautions with Alcohol
- Alcohol-Telithromycin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- KETEK®[1]
Look-Alike Drug Names
There is limited information regarding Telithromycin Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.