Sugammadex
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Sugammadex is a modified gamma cyclodextrin that is FDA approved for the of reversal of neuromuscular blockade induced by rocuronium bromide and vecuronium bromide in adults undergoing surgery. Common adverse reactions include vomiting, pain, nausea, hypotension, and headache (≥10%).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Sugammadex is indicated for the reversal of neuromuscular blockade induced by rocuronium bromide and vecuronium bromide in adults undergoing surgery.
Dosage
Sugammadex injection, for intravenous use, should be administered by trained healthcare providers familiar with the use, actions, characteristics, and complications of neuromuscular blocking agents (NMBA) and neuromuscular block reversal agents.
Doses and timing of Sugammadex administration should be based on monitoring for twitch responses and the extent of spontaneous recovery that has occurred.
Administer Sugammadex intravenously as a single bolus injection. The bolus injection may be given over 10 seconds, into an existing intravenous line. Sugammadex has only been administered as a single bolus injection in clinical trials.
From the time of Sugammadex administration until complete recovery of neuromuscular function, monitor the patient to assure adequate ventilation and maintenance of a patent airway. Satisfactory recovery should be determined through assessment of skeletal muscle tone and respiratory measurements in addition to the response to peripheral nerve stimulation.
The recommended dose of Sugammadex does not depend on the anesthetic regimen.
- Recommended Dosing
Sugammadex can be used to reverse different levels of rocuronium- or vecuronium-induced neuromuscular blockade.
- For rocuronium and vecuronium:
- A dose of 4 mg/kg Sugammadex is recommended if spontaneous recovery of the twitch response has reached 1 to 2 post-tetanic counts (PTC) and there are no twitch responses to train-of-four (TOF) stimulation following rocuronium- or vecuronium-induced neuromuscular blockade.
- A dose of 2 mg/kg Sugammadex is recommended if spontaneous recovery has reached the reappearance of the second twitch (T2) in response to TOF stimulation following rocuronium- or vecuronium-induced neuromuscular blockade.
- For rocuronium only:
- A dose of 16 mg/kg Sugammadex is recommended if there is a clinical need to reverse neuromuscular blockade soon (approximately 3 minutes) after administration of a single dose of 1.2 mg/kg of rocuronium. The efficacy of the 16 mg/kg dose of Sugammadex following administration of vecuronium has not been studied.
Sugammadex dosing is based on actual body weight.
- Drug Compatibility
May inject Sugammadex into the intravenous line of a running infusion with the following intravenous solutions:
- 0.9% sodium chloride
- 5% dextrose
- 0.45% sodium chloride and 2.5% dextrose
- 5% dextrose in 0.9% sodium chloride
- isolyte P with 5% dextrose
- Ringer's lactate solution
- Ringer's solution
Ensure the infusion line is adequately flushed (e.g., with 0.9% sodium chloride) between administration of Sugammadex and other drugs.
Do not mix Sugammadex with other products except those listed above.
Sugammadex is physically incompatible with verapamil, ondansetron, and ranitidine.
Visually inspect parenteral drug products for particulate matter and discoloration prior to administration, whenever the solution and container permit.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sugammadex in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sugammadex in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and efficacy of Sugammadex in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Sugammadex in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Sugammadex in pediatric patients.
Contraindications
Sugammadex is contraindicated in patients with known hypersensitivity to Sugammadex or any of its components. Hypersensitivity reactions that occurred varied from isolated skin reactions to serious systemic reactions (i.e., anaphylaxis, anaphylactic shock) and have occurred in patients with no prior exposure to Sugammadex.
Warnings
Anaphylaxis and Hypersensitivity
Clinicians should be prepared for the possibility of drug hypersensitivity reactions (including anaphylactic reactions) and take the necessary precautions.
Potentially serious hypersensitivity reactions, including anaphylaxis, have occurred in patients treated with Sugammadex. The nature and frequency of anaphylaxis and hypersensitivity associated with Sugammadex administration were evaluated in a randomized, double-blind, placebo-controlled, parallel-group, repeat-dose study in which 375 subjects were randomized to receive 3 doses of Sugammadex IV with a 5 week washout period: 151 subjects received 4 mg/kg, 148 received 16 mg/kg and 76 received placebo. The frequency of anaphylaxis for the 299 healthy volunteers treated with intravenous Sugammadex was 0.3% (n=1 in the Sugammadex 16 mg/kg group on the first dose). Signs and symptoms included conjunctival edema, urticaria, erythema, swelling of the uvula and reduction in peak expiratory flow within 5 minutes of dose administration. The most common hypersensitivity adverse reactions reported were nausea, pruritus and urticaria and showed a dose response relationship, occurring more frequently in the 16 mg/kg group compared to the 4 mg/kg and placebo groups.
Anaphylaxis has also been reported in the post-marketing setting, including at doses less than 16 mg/kg. The most commonly described clinical features in reports of anaphylaxis were dermatologic symptoms (including urticaria, rash, erythema, flushing and skin eruption); and clinically important hypotension often requiring the use of vasopressors for circulatory support. In addition prolonged hospitalization and/or the use of additional respiratory support until full recovery (re-intubation, prolonged intubation, manual or mechanical ventilation) have been noted in a number of the anaphylaxis reports.
Marked Bradycardia
Cases of marked bradycardia, some of which have resulted in cardiac arrest, have been observed within minutes after the administration of Sugammadex. Patients should be closely monitored for hemodynamic changes during and after reversal of neuromuscular blockade. Treatment with anticholinergic agents, such as atropine, should be administered if clinically significant bradycardia is observed.
Respiratory Function Monitoring During Recovery
Ventilatory support is mandatory for patients until adequate spontaneous respiration is restored and the ability to maintain a patent airway is assured. Even if recovery from neuromuscular blockade is complete, other drugs used in the peri- and post-operative period could depress respiratory function and therefore ventilatory support might still be required.
Should neuromuscular blockade persist after Sugammadex administration or recur following extubation, take appropriate steps to provide adequate ventilation.
Risk of Prolonged Neuromuscular Blockade
In clinical trials, a small number of patients experienced a delayed or minimal response to the administration of Sugammadex. Thus, it is important to monitor ventilation until recovery occurs.
Waiting Times for Re-Administration of Neuromuscular Blocking Agents for Intubation Following Reversal with Sugammadex
A minimum waiting time is necessary before administration of a steroidal neuromuscular blocking agent after administration of Sugammadex.
- Table 1: Re-administration of Rocuronium or Vecuronium after Reversal (up to 4 mg/kg Sugammadex)
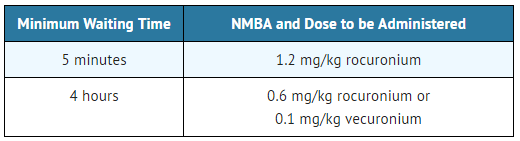
When rocuronium 1.2 mg/kg is administered within 30 minutes after reversal with Sugammadex, the onset of neuromuscular blockade may be delayed up to approximately 4 minutes and the duration of neuromuscular blockade may be shortened up to approximately 15 minutes.
The recommended waiting time in patients with mild or moderate renal impairment for re-use of 0.6 mg/kg rocuronium or 0.1 mg/kg vecuronium after reversal with up to 4 mg/kg Sugammadex should be 24 hours. If a shorter waiting time is required, the rocuronium dose for a new neuromuscular blockade should be 1.2 mg/kg.
For re-administration of rocuronium or administration of vecuronium after reversal of rocuronium with 16 mg/kg Sugammadex, a waiting time of 24 hours is suggested.
If neuromuscular blockade is required before the recommended waiting time has elapsed, use a nonsteroidal neuromuscular blocking agent. The onset of a depolarizing neuromuscular blocking agent might be slower than expected, because a substantial fraction of postjunctional nicotinic receptors can still be occupied by the neuromuscular blocking agent.
Interactions Potentially Affecting the Efficacy of Other Drugs
Due to the administration of Sugammadex, certain drugs, including hormonal contraceptives, could become less effective due to a lowering of the (free) plasma concentrations. In this situation, consider the re-administration of the other drug, the administration of a therapeutically equivalent drug (preferably from a different chemical class), and/or non-pharmacological interventions as appropriate.
Risk of Recurrence of Neuromuscular Blockade Due to Displacement Interactions
Recurrence of neuromuscular blockade may occur due to displacement of rocuronium or vecuronium from Sugammadex by other drugs. In this situation the patient may require mechanical ventilation. Administration of the drug which caused displacement should be stopped in case of an infusion. The risk of displacement reactions will be the highest in the time period equivalent to 3 times the half-life of Sugammadex.
Risk of Recurrence of Neuromuscular Blockade with Lower Than Recommended Dosing
The use of lower than recommended doses of Sugammadex may lead to an increased risk of recurrence of neuromuscular blockade after initial reversal and is not recommended.
Risk of Recurrence of Neuromuscular Blockade Due to the Administration of Drugs that Potentiate Neuromuscular Blockade
When drugs which potentiate neuromuscular blockade are used in the post-operative phase, special attention should be paid to the possibility of recurrence of neuromuscular blockade. Refer to the package insert for rocuronium or vecuronium for a list of the specific drugs which potentiate neuromuscular blockade. In case recurrence of neuromuscular blockade is observed, the patient may require mechanical ventilation.
Risk of Coagulopathy and Bleeding
Sugammadex doses up to 16 mg/kg were associated with increases in the coagulation parameters activated partial thromboplastin time (aPTT) and prothrombin time/international normalized ratio [PT(INR)] of up to 25% for up to 1 hour in healthy volunteers.
In patients undergoing major orthopedic surgery of the lower extremity who were concomitantly treated with heparin or low molecular weight heparin for thromboprophylaxis, increases in aPTT and PT(INR) of 5.5% and 3.0%, respectively, were observed in the hour following Sugammadex 4 mg/kg administration. This clinical trial did not demonstrate an increased blood loss or anemia incidence with Sugammadex compared with usual treatment. The rate of adjudicated bleeding events within 24 hours was 2.9% for Sugammadex and 4.1% for usual care. The rate of post-operative anemia was 21% for Sugammadex and 22% for usual care. The mean 24-hour drainage volume was 0.46 L for Sugammadex and 0.48 L for usual care. The need for any post-operative transfusion was 37% for Sugammadex and 39% for usual care.
In vitro experiments demonstrated additional aPTT and PT(INR) prolongations for Sugammadex in combination with vitamin K antagonists, unfractionated heparin, low molecular weight heparinoids, rivaroxaban, and dabigatran up to ~25% and ~50% at Cmax levels of Sugammadex corresponding to 4 mg/kg and 16 mg/kg doses, respectively.
Since bleeding risk has been studied systematically with only heparin and low molecular weight heparin thromboprophylaxis and 4 mg/kg doses of Sugammadex coagulation parameters should be carefully monitored in patients with known coagulopathies, being treated with therapeutic anticoagulation, receiving thromboprophylaxis drugs other than heparin and low molecular weight heparin, or receiving thromboprophylaxis drugs and who then receive a dose of 16 mg/kg Sugammadex.
Renal Impairment
Sugammadex is not recommended for use in patients with severe renal impairment, including those requiring dialysis. With regard to the recommended waiting time for re-administration in patients with mild or moderate renal impairment, see Waiting Times for Re-administration of Neuromuscular Blocking Agents for Intubation Following Reversal with Sugammadex.
Light Anesthesia
When neuromuscular blockade was reversed intentionally in the middle of anesthesia in clinical trials, e.g., when investigating urgent reversal, signs of light anesthesia were noted occasionally (movement, coughing, grimacing and suckling of the tracheal tube).
Reversal after Rocuronium or Vecuronium Administration in the ICU
Sugammadex has not been studied for reversal following rocuronium or vecuronium administration in the ICU.
Reversal of Neuromuscular Blocking Agents Other Than Rocuronium or Vecuronium
Do not use BRIDION to reverse blockade induced by nonsteroidal neuromuscular blocking agents such as succinylcholine or benzylisoquinolinium compounds.
Do not use Sugammadex to reverse neuromuscular blockade induced by steroidal neuromuscular blocking agents other than rocuronium or vecuronium.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The data described below reflect 2914 subjects exposed to 2, 4, or 16 mg/kg Sugammadex and 544 to placebo in pooled Phase 1-3 studies. The population was 18 to 92 years old, 47% male and 53% female, 34% ASA (American Society of Anesthesiologists) Class 1, 51% ASA Class 2, and 14% ASA Class 3, and 82% Caucasian. Most subjects received a single dose of Sugammadex 2 mg/kg or 4 mg/kg.
Adverse reactions reported in ≥10% of patients at a 2, 4, or 16 mg/kg Sugammadex dose with a rate higher than the placebo rate are: vomiting, pain, nausea, hypotension, and headache.
All adverse reactions occurring in ≥2% of subjects treated with Sugammadex and more often than placebo for adult subjects who received anesthesia and/or neuromuscular blocking agent in pooled Phase 1 to 3 studies are presented in Table 2.
- Table 2: Percent of Subject Exposures in Pooled Phase 1 to 3 Studies with Adverse Reactions Incidence ≥ 2%

Hypersensitivity reactions, including anaphylaxis, have occurred in both premarketing clinical trials and in post-marketing spontaneous reports. In a dedicated hypersensitivity study in healthy volunteers, the frequency of anaphylaxis was 0.3%. These reactions varied from isolated skin reactions to serious systemic reactions (i.e., anaphylaxis, anaphylactic shock) and have occurred in patients with no prior exposure to Sugammadex.
Symptoms associated with these reactions can include: flushing, urticaria, erythematous rash, (severe) hypotension, tachycardia, swelling of tongue, swelling of pharynx, bronchospasm and pulmonary obstructive events. Severe hypersensitivity reactions can be fatal.
A randomized, double-blind study examined the incidence of drug hypersensitivity reactions in healthy volunteers given up to 3 doses of placebo (N=76), Sugammadex 4 mg/kg (N=151) or Sugammadex 16 mg/kg (N=148). Reports of suspected hypersensitivity were adjudicated by a blinded committee. The incidence of adjudicated hypersensitivity was 1%, 7% and 9% in the placebo, Sugammadex 4 mg/kg and Sugammadex 16 mg/kg groups, respectively. There were no reports of anaphylaxis after placebo or Sugammadex 4 mg/kg. There was a single case of adjudicated anaphylaxis after the first dose of Sugammadex 16 mg/kg. The frequency of anaphylaxis for the 299 healthy volunteers treated with intravenous Sugammadex was 0.3%. There was no evidence of increased frequency or severity of hypersensitivity with repeat dosing.
In a previous study of similar design, there were three adjudicated cases of anaphylaxis, all after Sugammadex 16 mg/kg (incidence 1% in the 298 healthy volunteers treated with Sugammadex).
- Recurrence of Neuromuscular Blockade
In clinical studies with subjects treated with rocuronium or vecuronium, where Sugammadex was administered using a dose labeled for the depth of neuromuscular blockade (N=2022), an incidence of <1% was observed for recurrence of neuromuscular blockade as based on neuromuscular monitoring or clinical evidence.
In one dedicated clinical trial and in post-marketing data, in patients with a history of pulmonary complications, bronchospasm was reported as a possibly related adverse event.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of Sugammadex. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Cardiac Disorders: Cases of marked bradycardia and bradycardia with cardiac arrest have been observed within minutes after administration of Sugammadex. Other cardiac rhythm abnormalities have included atrial fibrillation, atrioventricular block, cardiac/cardiorespiratory arrest, ST segment changes, supraventricular tachycardia/extrasystoles, tachycardia, ventricular fibrillation, and ventricular tachycardia.
- General Disorders and Administration Site Conditions: Cases of Sugammadex not having the intended effect.
- Immune System Disorders: Hypersensitivity events including anaphylactic shock, anaphylactic reaction, anaphylactoid reaction, and Type 1 hypersensitivity have been reported.
- Respiratory, Thoracic, and Mediastinal Disorders: Events of laryngospasm, dyspnea, wheezing, pulmonary edema, and respiratory arrest have been reported.
Drug Interactions
- Summary
The information reported in the next sections is based on binding affinity between Sugammadex and other drugs, preclinical experiments, clinical studies and simulations of a pharmacokinetic-pharmacodynamic (PK-PD) model. Based on these considerations, no clinically significant pharmacodynamic interactions with other drugs are expected, with the exception of toremifene and hormonal contraceptives.
- Interactions Potentially Affecting the Efficacy of Sugammadex
For toremifene, which has a relatively high binding affinity for Sugammadex and for which relatively high plasma concentrations might be present, some displacement of vecuronium or rocuronium from the complex with Sugammadex could occur. The recovery to TOF ratio to 0.9 could therefore be delayed in patients who have received toremifene on the same day of surgery.
- Interaction Potentially Affecting the Efficacy of Hormonal Contraceptives
In vitro binding studies indicate that Sugammadex may bind to progestogen, thereby decreasing progestogen exposure. Therefore, the administration of a bolus dose of Sugammadex is considered to be equivalent to missing dose(s) of oral contraceptives containing an estrogen or progestogen. If an oral contraceptive is taken on the same day that Sugammadex is administered, the patient must use an additional, non-hormonal contraceptive method or back-up method of contraception (such as condoms and spermicides) for the next 7 days.
In the case of non-oral hormonal contraceptives, the patient must use an additional, non-hormonal contraceptive method or back-up method of contraception (such as condoms and spermicides) for the next 7 days.
- Interference with Laboratory Tests
Sugammadex may interfere with the serum progesterone assay. Interference with this test was observed at Sugammadex plasma concentrations of 100 mcg/mL, which may be observed for up to 30 minutes after a 16 mg/kg dose.
Use in Specific Populations
Pregnancy
- Risk Summary
There are no data on Sugammadex use in pregnant women to inform any drug-associated risks. In animal reproduction studies, there was no evidence of teratogenicity following daily intravenous administration of Sugammadex to rats and rabbits during organogenesis at exposures of up to 6 and 8 times, respectively, the maximum recommended human dose (MRHD) of 16 mg/kg. However, there was an increase in the incidence of incomplete ossification of the sternebra and reduced fetal body weights in the rabbit study at 8 times the MRHD, which is a dose level in which maternal toxicity was also observed. In a pre- and postnatal development study, Sugammadex treatment resulted in an increase in early postnatal loss, which correlated with maternal behavior (increased incidence of pup cannibalism), at exposures equivalent to the MRHD and higher. The background risk of major birth defects and miscarriage for the indicated population are unknown. However, the background risk in the U.S. general population of major birth defects is 2-4% and of miscarriage is 15-20% of clinically recognized pregnancies.
- Data
- Animal Data
In an embryofetal development study in rats, pregnant animals received daily intravenous administration of Sugammadex at 0, 20, 100, and 500 mg/kg (0.2, 1, and 6-times the MRHD of 16 mg/kg/day, respectively, based on AUC comparison) during organogenesis (Gestational Days 6 - 17). No treatment-related maternal and embryofetal changes were observed.
In another embryofetal development study, pregnant New Zealand white rabbits received daily intravenous administration of Sugammadex at 0, 20, 65, 200 mg/kg (0.6, 2, and 8 times the MRHD, respectively, based on AUC comparison) during organogenesis (Gestational Days 6-18). Fetal body weight decreases (10 and 14%, respectively) were observed in the offspring at maternal doses of 65 mg/kg and 200 mg/kg. In addition, incomplete ossification of sternebra, and unossified 1st metacarpal were noted at a maternal dose of 200 mg/kg/day. Maternal toxicity was also observed at 200 mg/kg. Considering the observed effects of Sugammadex on bone, it is possible that these findings may be attributable to drug. There was no evidence of teratogenicity at any dose.
In a prenatal and postnatal development study, pregnant rats were administered Sugammadex intravenously at 0, 30, 120, and 500 mg/kg (0.3, 1, and 6 times the MRHD, respectively, based on AUC comparison) from Gestational Day (GD) 6 to Postnatal Day (PND) 21 (corresponding to the beginning of organogenesis through parturition and subsequent pup weaning). Postnatal loss during PND 1-4 was noted across control litters and treated litters from dams receiving Sugammadex as a result of pup cannibalization by dams. Overall incidence of affected litters was 2, 1, 4, and 3 litters, respectively, at 0, 30, 120, or 500 mg/kg/day. The reason for the increased cannibalization is not known. An effect of Sugammadex on steroidal hormones and/or pheromones cannot be ruled out. In addition, there were no drug-related effects on parturition in rats during evaluations for prenatal or postnatal development.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Sugammadex in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Sugammadex during labor and delivery.
Nursing Mothers
- Risk Summary
No data are available regarding the presence of Sugammadex in human milk, the effects of Sugammadex on the breast fed infant, or the effects of Sugammadex on milk production. However, Sugammadex is present in rat milk. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for Sugammadex and any potential adverse effects on the breastfed infant from Sugammadex or from the underlying maternal condition.
- Data
In a milk excretion study in rat dams following single intravenous dose of 20 mg/kg Sugammadex on Postnatal Day 9, the maximum drug level was achieved at about 30 minutes after dosing with a ratio of milk to plasma level approximately 1:1. The oral exposure via milk did not induce effects on survival, body weight and physical or the behavioral developmental parameters monitored in rats in the prenatal and postnatal development studies.
Pediatric Use
The safety and efficacy of Sugammadex in pediatric patients have not been established.
- Juvenile Animal Studies
In a bone deposition study, Sugammadex concentrations were significantly higher in juvenile rats compared to adult rats (13% vs. 3% of the administered dose, respectively) following a single intravenous (IV) dose at 30 mg/kg (0.3 times the MRHD based on adult AUC comparison).
In a juvenile animal bone toxicity study, 7-day old rats were dosed intravenously once daily for 28 days with 0, 30, 120, and 500 mg/kg Sugammadex (approximately 0.1, 0.6, and 3 times the MRHD, respectively, by adult AUC comparison). Sugammadex at 120 and 500 mg/kg decreased ulna and femur bone lengths by approximately 3%, which did not recover after an 8-week treatment-free period. Reversible whitish discoloration and disturbance of enamel formation were also observed in the incisors at these dose levels. In molars, this effect was only observed at 500 mg/kg. The no-observed-effect-level (NOEL) was 30 mg/kg.
In a second juvenile animal bone toxicity study, 7-day old rats were dosed once weekly for 8 weeks with 0, 7.5, 30, and 120 mg/kg (up to 1.2 times the MRHD of 16 mg/kg based on adult AUC comparison). No adverse effects on bone or teeth were noted.
Geriatic Use
Sugammadex has been administered in a dedicated clinical study to a total 102 geriatric patients that compared the time to recovery from neuromuscular blockade induced by rocuronium (0.6 mg/kg) following administration of 2 mg/kg Sugammadex given at the reappearance of T2 in 65-74 year-olds (N=62) and ≥75 year-olds (N=40) compared with 18-64 year-olds (N=48). The median time to recovery of the TOF (T4/T1) ratio to 0.9 in 18-64 year-olds was 2.2 minutes; in 65-74 year-olds it was 2.5 minutes, and in ≥75 year-olds it was 3.6 minutes. For time to recovery from neuromuscular blockade induced by rocuronium following administration of 4 mg/kg Sugammadex given at 1-2 PTCs, results across clinical trials revealed a median recovery of 2.5 minutes for geriatric patients (≥65 years, N=63) versus 2.0 minutes, for adults aged 18-64 years (N=359). Hence no dose adjustment is necessary in geriatric patients with normal organ function.
This drug is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Sugammadex with respect to specific gender populations.
Race
There is no FDA guidance on the use of Sugammadex with respect to specific racial populations.
Renal Impairment
This drug is known to be substantially excreted by the kidney. Effect of mild or moderate renal impairment (creatine clearance ≥30 and ≤80 mL/min) on Sugammadex PK and PD was obtained from a study in elderly patients. Although clearance of drug decreased in elderly subjects with mild and moderate renal impairment, there was no significant difference in the ability of Sugammadex to reverse the pharmacodynamic effect of rocuronium. Hence, no dosage adjustment is necessary for mild and moderate renal impairment. Sugammadex is not recommended for use in patients with severe renal impairment (creatine clearance <30 mL/min) due to insufficient safety information combined with the prolonged and increased overall exposure in these patients.
Hepatic Impairment
Sugammadex is not metabolized nor excreted by the liver; therefore, dedicated trials in patients with hepatic impairment have not been conducted. Exercise caution when administering Sugammadex to patients with hepatic impairment accompanied by coagulopathy or severe edema.
Females of Reproductive Potential and Males
- Contraception
Upon administration of Sugammadex, the efficacy of hormonal contraceptives may be reduced for up to 7 days. Advise female patients of reproductive potential using hormonal contraceptives to use an additional, non-hormonal contraceptive for the next 7 days following Sugammadex administration.
Immunocompromised Patients
There is no FDA guidance one the use of Sugammadex in patients who are immunocompromised.
Pulmonary Patients
One trial of 77 patients who were diagnosed with or have a history of pulmonary complications investigated the time to recovery from neuromuscular blockade induced by rocuronium (0.6 mg/kg) following administration of 2 mg/kg or 4 mg/kg Sugammadex given at the first signs of recovery (reappearance of T2). The trial showed that for these patients the median time to recovery of the T4/T1 ratio to 0.9 was 2.1 minutes after a dose of 2 mg/kg Sugammadex and 1.9 minutes after a dose of 4 mg/kg Sugammadex. This is similar to the median values observed in the other trials; therefore, no dosage adjustment is necessary.
Administration and Monitoring
Administration
Sugammadex injection, for intravenous use, should be administered by trained healthcare providers familiar with the use, actions, characteristics, and complications of neuromuscular blocking agents (NMBA) and neuromuscular block reversal agents.
Doses and timing of Sugammadex administration should be based on monitoring for twitch responses and the extent of spontaneous recovery that has occurred.
Administer Sugammadex intravenously as a single bolus injection. The bolus injection may be given over 10 seconds, into an existing intravenous line. Sugammadex has only been administered as a single bolus injection in clinical trials.
From the time of Sugammadex administration until complete recovery of neuromuscular function, monitor the patient to assure adequate ventilation and maintenance of a patent airway. Satisfactory recovery should be determined through assessment of skeletal muscle tone and respiratory measurements in addition to the response to peripheral nerve stimulation.
The recommended dose of Sugammadex does not depend on the anesthetic regimen.
Monitoring
There is limited information regarding Sugammadex Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Sugammadex and IV administrations.
Overdosage
In premarketing clinical trials, one case of accidental overdose with 40 mg/kg Sugammadex was reported without significant effects.
Sugammadex can be removed using hemodialysis with a high-flux filter, but not with a low-flux filter. Based upon clinical studies, Sugammadex concentrations in plasma are reduced with a high-flux filter by about 70% after a 3- to 6-hour dialysis session.
Pharmacology
| |
| |
Sugammadex
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | |
| ATC code | V03 |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 2178 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Licence data |
|
| Pregnancy cat. |
? |
| Legal status |
POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Intravenous |
Mechanism of Action
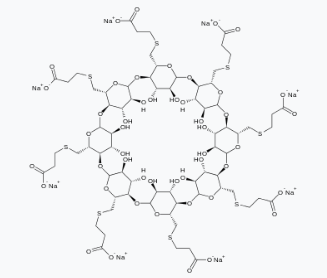
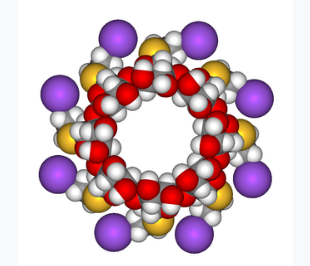
Sugammadex is a modified gamma cyclodextrin. It forms a complex with the neuromuscular blocking agents rocuronium and vecuronium, and it reduces the amount of neuromuscular blocking agent available to bind to nicotinic cholinergic receptors in the neuromuscular junction. This results in the reversal of neuromuscular blockade induced by rocuronium and vecuronium.
Structure
There is limited information regarding Sugammadex Structure in the drug label.
Pharmacodynamics
Sugammadex has been administered in doses ranging from 0.5 mg/kg to 16 mg/kg in dose response trials of rocuronium-induced blockade (0.6, 0.9, 1 and 1.2 mg/kg with and without maintenance doses) and vecuronium-induced blockade (0.1 mg/kg with or without maintenance doses) at different time points/depths of block. In these trials a clear dose-response relationship was observed.
Sugammadex may contain up to 7% of the mono OH-derivative of Sugammadex. In preclinical pharmacology studies, the mono OH-derivative was demonstrated to have ~50% of the affinity as Sugammadex for rocuronium and vecuronium and that product with up to 7% of the mono OH-derivative has nearly similar efficacy in reversing rocuronium- or vecuronium-induced blockade.
Although Sugammadex has greatest affinity for aminosteroid neuromuscular blocking agents such as rocuronium and vecuronium, plasma levels of endogenous or exogenous compounds with a similar steroidal structure, such as some hormones, hormonal contraceptives, and pheromones may also be reduced following administration of Sugammadex.
At a dose 2 times the maximum recommended dose, Sugammadex does not prolong the QTc interval to any clinically relevant extent.
Pharmacokinetics
The Sugammadex pharmacokinetic parameters were calculated from the total sum of non-complex-bound and complex-bound concentrations of Sugammadex. Pharmacokinetic parameters as clearance and volume of distribution are assumed to be the same for non-complex-bound and complex-bound Sugammadex in anesthetized patients.
The observed steady-state volume of distribution of Sugammadex is approximately 11 to 14 liters in adult patients with normal renal function (based on conventional, non-compartmental pharmacokinetic analysis). Neither Sugammadex nor the complex of Sugammadex and rocuronium binds to plasma proteins or erythrocytes, as was shown in vitro using male human plasma and whole blood. Sugammadex exhibits linear kinetics in the dosage range of 1 to 16 mg/kg when administered as an IV bolus dose.
In nonclinical drug distribution studies, Sugammadex is retained in sites of active mineralization, such as bone and teeth, with a mean half-life of 172 and 8 days, respectively.
In clinical studies, no metabolites of Sugammadex have been observed and only renal excretion of the unchanged product was observed as the route of elimination.
In adult anesthetized patients with normal renal function, the elimination half-life (t1/2) of Sugammadex is about 2 hours and the estimated plasma clearance is about 88 mL/min (based on compartmental pharmacokinetic analysis). A mass balance study demonstrated that >90% of the dose was excreted within 24 hours. Ninety-six percent (96%) of the dose was excreted in urine, of which at least 95% could be attributed to unchanged Sugammadex. Excretion via feces or expired air was less than 0.02% of the dose. Administration of Sugammadex to healthy volunteers resulted in increased renal elimination of rocuronium in complex.
- Patients with Renal Impairment
Sugammadex is known to be substantially excreted by the kidney. The half-life of Sugammadex in patients with mild, moderate and severe renal impairment is 4, 6, and 19 hours, respectively.
In one study, exposure to Sugammadex was prolonged, leading to 17-fold higher overall exposure in patients with severe renal impairment. Low concentrations of sugammadex are detectable for at least 48 hours post-dose in patients with severe renal impairment.
In a second study comparing subjects with moderate or severe renal impairment to subjects with normal renal function, Sugammadex clearance progressively decreased and t1/2 was progressively prolonged with declining renal function. Exposure was 2-fold and 5-fold higher in subjects with moderate and severe renal impairment, respectively. Sugammadex concentrations were no longer detectable beyond 7 days post-dose in subjects with severe renal impairment.
- Age: Geriatric Population
Geriatric patients may have mild or moderate renal impairment. Population pharmacokinetic analysis indicated that, beyond the effects of a decreased creatinine clearance, increased age has limited impact on Sugammadex PK parameters.
- Sex
No pharmacokinetic differences between male and female subjects were observed.
- Race
In a study in healthy Japanese and Caucasian subjects no clinically relevant differences in pharmacokinetic parameters were observed. Limited data do not indicate differences in pharmacokinetic parameters in Black or African Americans.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term animal studies to evaluate the carcinogenic potential of Sugammadex have not been conducted.
Sugammadex and its mono OH-derivative tested negatively in in vitro bacterial reverse mutation assays (Ames test), in vitro chromosomal aberration assays in human peripheral blood lymphocytes, and in vivo micronucleus assays in mice and rats.
- Impairment of Fertility
A fertility and early embryonic development study in Sprague-Dawley rats in which male rats were treated daily for 29 days prior to mating and through the mating period and female rats were treated daily for 14 days prior to mating to Day 5 post-coitum via intravenous administration of Sugammadex at 20, 100, and 500 mg/kg (0.2, 1, and 6 times the MRHD of 16 mg/kg, respectively, based on AUC comparison) did not show adverse effects on fertility.
Animal Toxicology and/or Pharmacology
Bone and teeth retention of Sugammadex occurred in rats after intravenous injection, with mean half-lives of 172 and 8 days, respectively. Sugammadex bound to hydroxyapatite in an in vitro study and distributed in the bone formation area where hydroxyapatite is present for mineralization in vivo.
In adult rat bone toxicity studies, a single dose of Sugammadex at 2000 mg/kg (approximately 24 times the maximum recommended human dose (MRHD) of 16 mg/kg by AUC comparison) administered to adult rats caused a slight increase in bone resorption, but had no effect on teeth color. No adverse bone effects were seen following a single dose of Sugammadex at 500 mg/kg (4 times the MRHD dose of 16 mg/kg based on plasma AUC comparison).
In a bone repair study, adult rats were treated with intravenous Sugammadex weekly for 6 weeks at 0, 30, 120, and 500 mg/kg (approximately 0.4, 1, and 6 times the MRHD, respectively, by AUC comparison). Based on histological data, high dose animals with post-fracture treatment, showed a statistically significant increase in callus formation and decrease in bone formation, suggesting a potential for a slight delay in the bone healing process. However there were no statistically significant effects on bone volume or bone mineral density.
In juvenile animal studies, bone and teeth deposition was significantly higher in juvenile rats compared to adults. In addition, Sugammadex administered to juvenile rats daily for 4 weeks caused slight bone length decrease (approximately 3%), which did not recover after an 8-week treatment-free period, and reversible whitish discoloration of the teeth at a dose approximately 0.6 times the MRHD, while weekly administration for 8 weeks did not produce similar changes in bone and teeth at doses up to 1.2 times the MRHD.
Clinical Studies
- Controlled Clinical Studies
- Comparative Study of Sugammadex versus Neostigmine as a Reversal Agent for Neuromuscular Blockade Induced by Rocuronium or Vecuronium at Reappearance of T2 (Moderate Blockade)
A multicenter, randomized, parallel-group, active-controlled, safety-assessor blinded study comparing Sugammadex and neostigmine enrolled 189 patients (87 women and 102 men, 95% were ASA class 1 and 2 and 99% were Caucasian, median weights were 72 kg and 76 kg and median ages were 50 years and 51 years in the rocuronium and vecuronium groups, respectively). Patients were randomly assigned to the rocuronium or vecuronium group and underwent elective surgical procedures under general anesthesia that required endotracheal intubation and maintenance of neuromuscular blockade. The surgical procedures were mainly endocrine, ocular, ENT, abdominal (gynecological, colorectal, urological), orthopedic, vascular, or dermatological. At the reappearance of T2, after the last dose of rocuronium or vecuronium, 2 mg/kg Sugammadex or 50 mcg/kg neostigmine was administered in a randomized order as a single bolus injection. The time from start of administration of Sugammadex or neostigmine to recovery of the TOF (T4/T1) ratio to 0.9 was assessed. Generally, a T4/T1 ratio ≥0.9 correlates with recovery from neuromuscular blockade.
Return of the T4/T1 ratio to 0.9 after the reappearance of T2 was overall faster with Sugammadex 2 mg/kg as compared to neostigmine 50 mcg/kg in the setting of rocuronium or vecuronium-induced neuromuscular blockade (Figures 1 and 2).
- Figure 1: Time (Minutes) from Administration of Sugammadex or Neostigmine at the Reappearance of T2 after Rocuronium to Recovery of the T4/T1 Ratio to 0.9

- Figure 2: Time (Minutes) from Administration of Sugammadex or Neostigmine at the Reappearance of T2 after Vecuronium to Recovery of the T4/T1 Ratio to 0.9

- Comparative Study of Sugammadex versus Neostigmine as a Reversal Agent for Neuromuscular Blockade Induced by Rocuronium or Vecuronium at 1 to 2 PTCs (Deep Blockade)
A multicenter, randomized, parallel-group, active-controlled, safety-assessor blinded study comparing Sugammadex and neostigmine enrolled 157 patients (86 women and 71 men; 8% ASA class 1, 71% class 2, and 21% class 3; 79% Caucasian; median weights of 81 kg and 84 kg, and median ages of 54 years and 56 years in the rocuronium and vecuronium groups, respectively). Patients were randomly assigned to the rocuronium or vecuronium group and underwent elective surgical procedures under general anesthesia that required endotracheal intubation and maintenance of neuromuscular blockade. The surgical procedures were mainly abdominal (gynecological, colorectal, urological), orthopedic, reconstructive, or neurological. At 1 to 2 PTCs, after the last dose of rocuronium or vecuronium, 4 mg/kg Sugammadex or 70 mcg/kg neostigmine was administered in a randomized order as a single bolus injection. The time from start of administration of Sugammadex or neostigmine to recovery of the TOF (T4/T1) ratio to 0.9 was assessed, although neostigmine was not expected to reverse neuromuscular blockade at a depth of 1 to 2 PTCs. Generally, a T4/T1 ratio ≥0.9 correlates with recovery from neuromuscular blockade.
Return of the T4/T1 ratio to 0.9 in patients with 1 to 2 PTCs with Sugammadex 4 mg/kg had a wider range of recovery times but the median time to recovery was comparable to the study of reversal at T2 (2.7 minutes with 25th and 75th percentiles of 2.1 and 4.3 minutes for rocuronium [N=37], and 3.3 minutes with 25th and 75th percentiles of 2.3 and 6.6 minutes for vecuronium [N=47]). There were 7 and 6 censored observations in the rocuronium and vecuronium groups, respectively.
- Reversal of Neuromuscular Blockade 3 Minutes after Rocuronium 1.2 mg/kg
Time to recovery from neuromuscular blockade induced by succinylcholine compared with recovery from neuromuscular blockade induced by rocuronium followed 3 minutes later with Sugammadex was assessed in a multicenter, randomized, parallel-group, active-controlled, safety-assessor blinded study. The study was conducted in 110 patients (64 women and 46 men, ASA class 1 and 2, 78% were Caucasian, median weight was 70 kg, median age was 43 years). Patients underwent elective surgical procedures under general anesthesia that required endotracheal intubation and a short duration of neuromuscular relaxation. The laparoscopic or open surgical procedures were mainly gynecological, orthopedic, or reconstructive. Return of the first twitch in a TOF (T1) to 10% of baseline was compared between Sugammadex 16 mg/kg for reversal of rocuronium 1.2 mg/kg versus spontaneous recovery from succinylcholine 1 mg/kg.
Recovery to T1 of 10% of baseline (relative to the time of administration of rocuronium or succinylcholine) was overall faster in the rocuronium/Sugammadex group compared with succinylcholine alone (Table 3).
- Table 3: Time (minutes) from Start of Administration of Rocuronium or Succinylcholine to Recovery of T1 to 10% of Baseline

BRIDION: Sugammadex's Brand name
How Supplied
- Sugammadex 2-mL single-dose vials containing 200 mg Sugammadex (100 mg/mL)
Box of 10 NDC 0006-5423-12
- Sugammadex 5-mL single-dose vials containing 500 mg Sugammadex (100 mg/mL)
Box of 10 NDC 0006-5423-15
The packaging of this product is not made with natural rubber latex.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light. When not protected from light, the vial should be used within 5 days.
Images
Drug Images
{{#ask: Page Name::Sugammadex |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel

{{#ask: Label Page::Sugammadex |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise females of reproductive potential using hormonal contraceptives that Sugammadex may reduce the contraceptive effect. Instruct females to use an additional, non-hormonal method of contraception for the next 7 days following Sugammadex administration
Precautions with Alcohol
Alcohol-Sugammadex interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
BRIDION®
Look-Alike Drug Names
There is limited information regarding Sugammadex Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.