Secondary hyperaldosteronism pathophysiology: Difference between revisions
No edit summary |
Ahmed Younes (talk | contribs) |
||
| (One intermediate revision by one other user not shown) | |||
| Line 7: | Line 7: | ||
=== Renin-angiotensin system components === | === Renin-angiotensin system components === | ||
Renin: | [[Renin]]: | ||
* In each kidney there is a specialized system called juxtaglomerular | * In each [[kidney]] there is a specialized system called [[juxtaglomerular apparatus]], which is located in [[afferent arteriole]] of each [[glomerulus]]. | ||
* | * [[Juxtaglomerular apparatus]] synthesizes prorenin, and then later it converts into [[renin]] with mediation of a [[proteolytic enzyme]]. | ||
* Renin stores in and then may be released from secretory granules, in response to various factors. | * [[Renin]] stores in and then may be released from secretory [[granules]], in response to various factors. | ||
* Renin releasing starts a cascade of steps, and the first step is the cleavage of the angiotensin I from angiotensinogen (renin substrate). | * [[Renin]] releasing starts a cascade of steps, and the first step is the cleavage of the [[angiotensin]] I from [[angiotensinogen]] ([[renin]] substrate). | ||
* Angiotensinogen is an alpha-2-globulin that is produced in the liver and kidney and other organs. | * [[Angiotensinogen]] is an alpha-2-globulin that is produced in the [[liver]] and [[kidney]] and other organs. | ||
* The first step is the rate-limiting step of the renin-angiotensin cascade. | * The first step is the rate-limiting step of the [[Renin-angiotensin system|renin-angiotensin]] cascade. | ||
* Most important stimuli to renin secretion are : | * Most important stimuli to [[renin]] secretion are : | ||
** Renal hypoperfusion, due to hypotension or volume depletion | ** [[Renal]] hypoperfusion, due to hypotension or [[volume depletion]] | ||
** Increased sympathetic activity. | ** Increased [[sympathetic]] activity. | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 67: | Line 67: | ||
[[Image:Renin-angiotensin system in man shadow.png|600px|center|Renin angiotensin system, by Mikael Häggström - https://commons.wikimedia.org/w/index.php?curid=8458370]] | [[Image:Renin-angiotensin system in man shadow.png|600px|center|thumb|Renin angiotensin system, by Mikael Häggström - https://commons.wikimedia.org/w/index.php?curid=8458370]] | ||
Latest revision as of 21:38, 28 September 2017
|
Secondary hyperaldosteronism Microchapters |
|
Differentiating Secondary Hyperaldosteronism from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Secondary hyperaldosteronism pathophysiology On the Web |
|
American Roentgen Ray Society Images of Secondary hyperaldosteronism pathophysiology |
|
Risk calculators and risk factors for Secondary hyperaldosteronism pathophysiology |
Overview
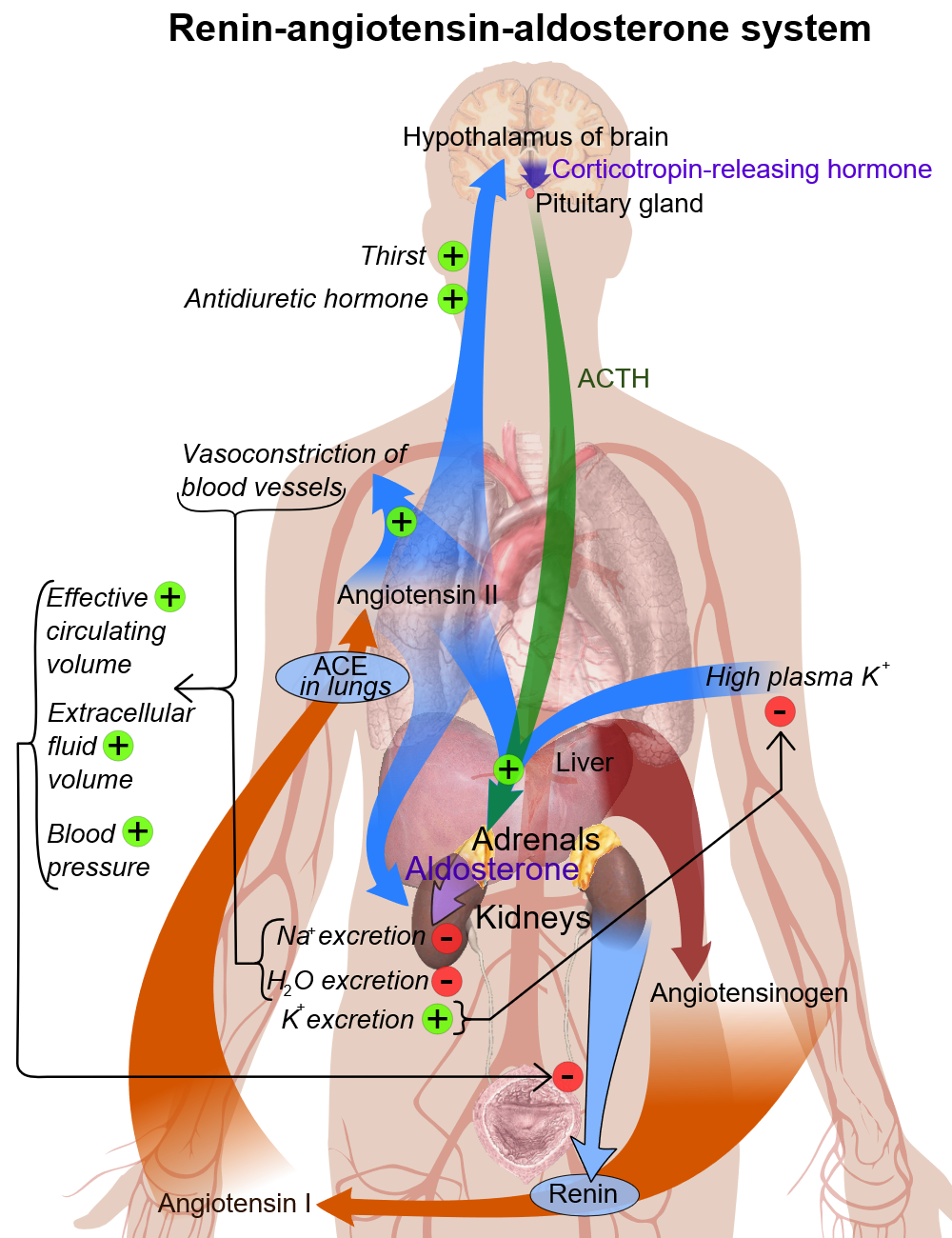
Secondary hyperaldosteronism is a disease of increasing aldosterone or other mineralocorticoid levels. The resulting Na+ retention produces hypertension, and elevated K+ excretion may cause hypokalemia.
Pathophysiology
Renin-angiotensin system components
- In each kidney there is a specialized system called juxtaglomerular apparatus, which is located in afferent arteriole of each glomerulus.
- Juxtaglomerular apparatus synthesizes prorenin, and then later it converts into renin with mediation of a proteolytic enzyme.
- Renin stores in and then may be released from secretory granules, in response to various factors.
- Renin releasing starts a cascade of steps, and the first step is the cleavage of the angiotensin I from angiotensinogen (renin substrate).
- Angiotensinogen is an alpha-2-globulin that is produced in the liver and kidney and other organs.
- The first step is the rate-limiting step of the renin-angiotensin cascade.
- Most important stimuli to renin secretion are :
- Renal hypoperfusion, due to hypotension or volume depletion
- Increased sympathetic activity.
| Renin-angiotensin system components | Secretion control | Measurement | Inhibition |
|---|---|---|---|
| Renin |
|
|
|
| Angiotensinogen | |||
| Angiotensin-converting enzyme | |||
| Angiotensin II | |||
| Aldosterone |
Basic physiology of aldosterone
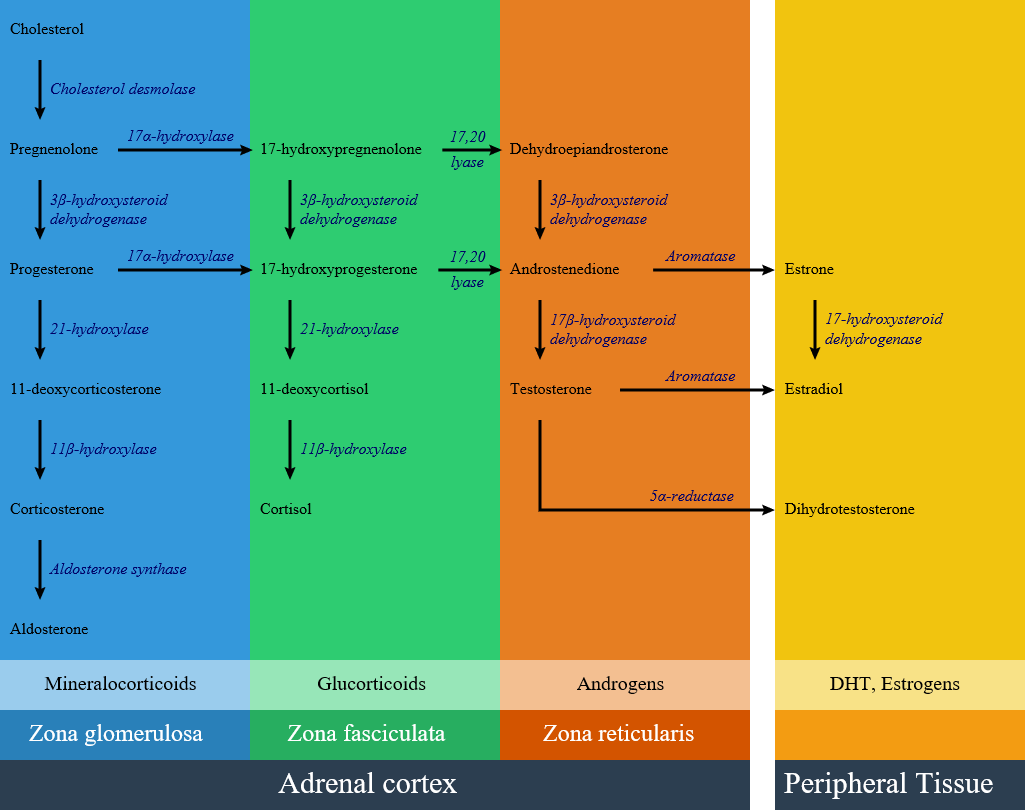
Circulating aldosterone is principally made in the zona glomerulosa of the adrenal cortex (outer layer of the cortex) by a cascade of enzyme steps leading to the conversion of cholesterol to aldosterone.
- Aldosterone's production is regulated at two critical enzyme steps:
- (1) early in its biosynthetic pathway (the conversion of cholesterol to pregnenolone by cholesterol side chain cleavage enzyme) and
- (2) late (the conversion of corticosterone to aldosterone by aldosterone synthase).
- A variety of factors modify aldosterone secretion--the most important are angiotensin II (AngII), the end-product of the renin-angiotensin system (RAS), and potassium. However ACTH, neural mediators and natriuretic factors also play part in the feedback mechanism.
- Aldosterone's classical epithelial effect is to increase the transport of sodium across the cell in exchange for potassium and hydrogen ions. [1]
Pathogenesis
Secondary hyperaldosteronism syndrome is a disease of increasing aldosterone or other mineralocorticoid levels. The resulting Na+ retention produces hypertension, and elevated K+ excretion may cause hypokalemia. Patients with Secondary hyperaldosertonism may have:
- Renin-producing tumors
- Renal artery stenosis
- Cushing syndrome
- Liddle's syndrome
- Ectopic ACTH production
- Licorice ingestion
- Other mineralocorticoids excess:
Genetics
References
- ↑ Williams GH (2005). "Aldosterone biosynthesis, regulation, and classical mechanism of action". Heart Fail Rev. 10 (1): 7–13. doi:10.1007/s10741-005-2343-3. PMID 15947886.
- ↑ "File:Adrenal Steroids Pathways.svg - Wikimedia Commons".