Sandbox:hypopituitarism pathophys
|
Hypopituitarism Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Sandbox:hypopituitarism pathophys On the Web |
|
American Roentgen Ray Society Images of Sandbox:hypopituitarism pathophys |
|
Risk calculators and risk factors for Sandbox:hypopituitarism pathophys |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Ahmed Elsaiey, MBBCH [2]
Overview
Pathophysiology
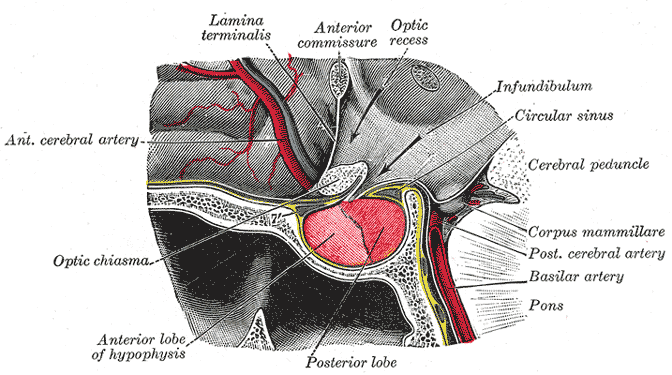
Background on pituitary gland blood supply
- In order to understand the pathophysiology of hypopituitarism, it is necessary to know the blood supply of the pituitary as the disease occurs mainly by ischemia through different mechanisms like hemorrhage, tumors or brain injury.[1][2]
- Pituitary gland is composed of two parts anterior (adenohypophysis) and posterior (neurohypophysis). Both parts are supplied by the carotid arteries.
- Adenohypophysis: It receives blood supply from the long and short hypophyseal arteries which arise from the internal carotid artery and the anterior of circle of willis.
- Neurohypophysis: It receives the blood supply from the inferior and middle hypophyseal arteries.
Pathogenesis
- Hypopituitarism pathogenesis is mainly due to destruction of the gland cells by different ways like ischemia, inflammation or infiltration. However, ischemia is believed to be the cornerstone of hypopituitarism pathogenesis caused via different ways.[3][4]
- Compression of the blood vessels:[5]
- Pituitary adenoma, secretory or non secretory, is one of the common causes that lead to loss of the pituitary function by compression on the hypophyseal vessels resulting in ischemia.
- Large adenomas (more than 1.5 cm) cause loss of function more than microadenomas. They cause compression on the pituitary stalk and the hypophyseal portal vessels which supply the gland with blood.
- The tumor growth in the gland participates in increasing the intrasellar pressure which cause decrease in the hypophyseal blood flow which ends up by decrease of hormonal delivery from the hypothalamus to the pituitary gland.
- Other lesions lead to compression includes carotid artery aneurysm, meningioma and craniopharyngioma.
- Traumatic brain injury (TBI):
- Hypopituitarism occurs either by primary brain injury or secondary events lead to brain injury.
- The anatomical sitting of the pituitary gland increases its susceptibility to get injured from trauma.
References
- ↑ Dusick JR, Wang C, Cohan P, Swerdloff R, Kelly DF (2012). "Pathophysiology of hypopituitarism in the setting of brain injury". Pituitary. 15 (1): 2–9. doi:10.1007/s11102-008-0130-6. PMC 4170072. PMID 18481181.
- ↑ Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla GK, Ghigo E (2007). "Hypopituitarism". Lancet. 369 (9571): 1461–70. doi:10.1016/S0140-6736(07)60673-4. PMID 17467517.
- ↑ Arafah BM (2002). "Medical management of hypopituitarism in patients with pituitary adenomas". Pituitary. 5 (2): 109–17. PMID 12675508.
- ↑ Vance, Mary Lee (1994). "Hypopituitarism". New England Journal of Medicine. 330 (23): 1651–1662. doi:10.1056/NEJM199406093302306. ISSN 0028-4793.
- ↑ Arafah BM, Prunty D, Ybarra J, Hlavin ML, Selman WR (2000). "The dominant role of increased intrasellar pressure in the pathogenesis of hypopituitarism, hyperprolactinemia, and headaches in patients with pituitary adenomas". J Clin Endocrinol Metab. 85 (5): 1789–93. doi:10.1210/jcem.85.5.6611. PMID 10843153.