Sandbox:Roukoz: Difference between revisions
No edit summary |
No edit summary |
||
| Line 48: | Line 48: | ||
==Pathophysiology== | ==Pathophysiology== | ||
Protein S is a natural anticoagulant that works with other proteins to regulate coagulation in the body. After it gets produced by the hepatocytes, endothelial cells, and megakaryocytes, protein S undergoes activation via vitamin K-dependent gamma-carboxylation. <ref name="pmid21239244">{{cite journal| author=Esmon CT| title=Protein S and protein C Biochemistry, physiology, and clinical manifestation of deficiencies. | journal=Trends Cardiovasc Med | year= 1992 | volume= 2 | issue= 6 | pages= 214-9 | pmid=21239244 | doi=10.1016/1050-1738(92)90027-P | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21239244 }} </ref> | *Protein S is a natural anticoagulant that works with other proteins to regulate coagulation in the body. After it gets produced by the hepatocytes, endothelial cells, and megakaryocytes, protein S undergoes activation via vitamin K-dependent gamma-carboxylation. <ref name="pmid21239244">{{cite journal| author=Esmon CT| title=Protein S and protein C Biochemistry, physiology, and clinical manifestation of deficiencies. | journal=Trends Cardiovasc Med | year= 1992 | volume= 2 | issue= 6 | pages= 214-9 | pmid=21239244 | doi=10.1016/1050-1738(92)90027-P | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21239244 }} </ref> | ||
*It serves as a cofactor for activated protein C, which inactivates procoagulant factors Va and VIIIa, reducing thrombin generation. Protein S also serves as a cofactor for activated protein C in enhancing fibrinolysis and can directly inhibit prothrombin activation via interactions with other coagulation factors | |||
*Mature gamma-carboxylated protein S circulates in two states: free, and bound to the complement component C4b-binding protein (C4b-BP). The free form comprises 30 to 40 percent of total protein S and is the only form of protein S that has cofactor activity for activated protein C | |||
Mature gamma-carboxylated protein S circulates in two states: free, and bound to the complement component C4b-binding protein (C4b-BP). The free form comprises 30 to 40 percent of total protein S and is the only form of protein S that has cofactor activity for activated protein C | |||
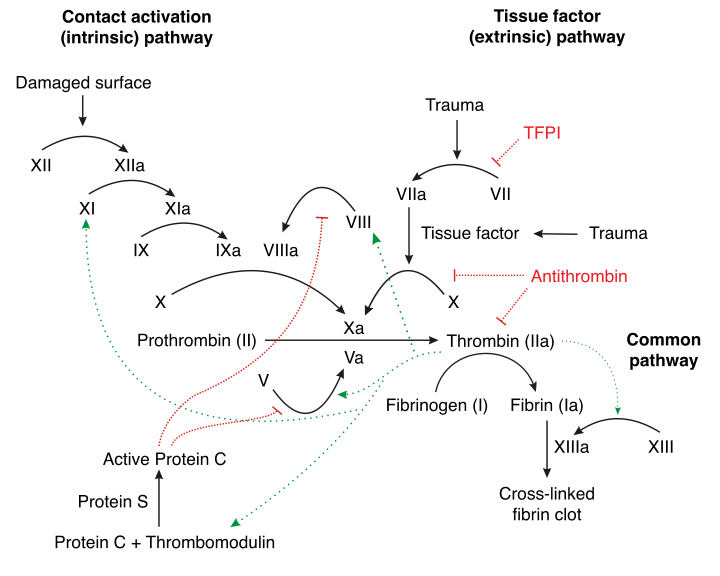
[[File:Coagulation cascade.png|none|thumb|600px|Coagulation cascade - Source: Wikipedia <ref name="urlProtein C - Wikipedia">{{cite web |url=https://en.wikipedia.org/wiki/Protein_C |title=Protein C - Wikipedia |format= |work= |accessdate=}}</ref>]] | [[File:Coagulation cascade.png|none|thumb|600px|Coagulation cascade - Source: Wikipedia <ref name="urlProtein C - Wikipedia">{{cite web |url=https://en.wikipedia.org/wiki/Protein_C |title=Protein C - Wikipedia |format= |work= |accessdate=}}</ref>]] | ||
| Line 64: | Line 61: | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
*The prevalence of protein S deficiency is approximately 90 per 100,000 individuals worldwide. <ref name="pmid24014240">{{cite journal| author=Pintao MC, Ribeiro DD, Bezemer ID, Garcia AA, de Visser MC, Doggen CJ et al.| title=Protein S levels and the risk of venous thrombosis: results from the MEGA case-control study. | journal=Blood | year= 2013 | volume= 122 | issue= 18 | pages= 3210-9 | pmid=24014240 | doi=10.1182/blood-2013-04-499335 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24014240 }} </ref> | |||
===Age=== | ===Age=== | ||
*The age of onset of thromboembolic events varies by heterozygous vs homozygous. | |||
**The thromboembolic events seen in heterozygous protein S deficiency usually occurs in individuals younger that 40-50 years of age. | |||
**The homozygous patients have neonatal purpura fulminans at birth. | |||
===Gender=== | ===Gender=== | ||
*There is no difference in the prevalence of the disease between men and women. | |||
===Race=== | ===Race=== | ||
*Current data shows that protein S deficiency affects Asians 5 to 10 times more than caucasians. | |||
==Risk Factors== | ==Risk Factors== | ||
Revision as of 10:18, 20 September 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Roukoz A. Karam, M.D.[2]
Overview
Protein S deficiency is an autosomal dominant thrombophilia, which leads to an increased risk of thromboembolic events. Protein S is a vitamin K-dependent glycoprotein and plays a role in anticoagulation. It is mainly a cofactor to the activated protein C (APC), which inactivates coagulation factors Va and VIIa and thereby controlling the coagulation cascade.
Historical Perspective
- Protein S was first discovered and purified in Seattle, Washington in 1979, and it was arbitrarily named protein S after the city it was discovered in.
- The function of this protein was still unknown; however, it was hypothesized that protein S plays a role in activating protein C.
- Protein S deficiency was first discovered in 1984 when two related individuals with recurrent thromboembolic events and normal coagulation tests were studied. At the time, protein C deficiency was usually associated with recurrent familial thrombosis. These individuals were found to have diminished anticoagulation activity with normal coagulation tests (including a normal protein C level), and when purified human protein S was added to their plasma, effective anticoagulation was restored. [1]
Classification
Protein S deficiency can be subdivided into three types depending on whether the abnormality affects total protein S level, free protein S level, and/or protein S function:
- Type I: Reduced total protein S, free protein S, and protein S function
It is the classic form of hereditary protein S deficiency. Total protein S levels drop to approximately 50% of normal values while free protein S levels collapse to almost 15% of the normal. On a genetic level, type I deficiency usually results from missense or nonsense mutations. On few occasions, microinsertions, microdeletions, and splice site mutations have occurred with this type. [2]
- Type II: Normal total and free protein S, reduced protein S function
This form results from a qualitative defect and is very rare. The genetics behind this type isn't certain; however, some reports have linked it to missense mutations affecting the protein S's ability to bind to the activated protein C. [3] [4]
- Type III: Normal total protein S, reduced free protein S and protein S function
This is a quantitative defect.
| Type | Total Protein S | Free Protein S | Protein S Function |
|---|---|---|---|
| I | ↓ | ↓ | ↓ |
| II | ↔ | ↔ | ↓ |
| III | ↔ | ↓ | ↓ |
Pathophysiology
- Protein S is a natural anticoagulant that works with other proteins to regulate coagulation in the body. After it gets produced by the hepatocytes, endothelial cells, and megakaryocytes, protein S undergoes activation via vitamin K-dependent gamma-carboxylation. [5]
- It serves as a cofactor for activated protein C, which inactivates procoagulant factors Va and VIIIa, reducing thrombin generation. Protein S also serves as a cofactor for activated protein C in enhancing fibrinolysis and can directly inhibit prothrombin activation via interactions with other coagulation factors
- Mature gamma-carboxylated protein S circulates in two states: free, and bound to the complement component C4b-binding protein (C4b-BP). The free form comprises 30 to 40 percent of total protein S and is the only form of protein S that has cofactor activity for activated protein C
Clinical Features
Differentiating [disease name] from other Diseases
Epidemiology and Demographics
- The prevalence of protein S deficiency is approximately 90 per 100,000 individuals worldwide. [7]
Age
- The age of onset of thromboembolic events varies by heterozygous vs homozygous.
- The thromboembolic events seen in heterozygous protein S deficiency usually occurs in individuals younger that 40-50 years of age.
- The homozygous patients have neonatal purpura fulminans at birth.
Gender
- There is no difference in the prevalence of the disease between men and women.
Race
- Current data shows that protein S deficiency affects Asians 5 to 10 times more than caucasians.
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
Diagnostic Criteria
Symptoms
Physical Examination
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Surgery
Prevention
References
- ↑ Comp PC, Nixon RR, Cooper MR, Esmon CT (1984). "Familial protein S deficiency is associated with recurrent thrombosis". J Clin Invest. 74 (6): 2082–8. doi:10.1172/JCI111632. PMC 425398. PMID 6239877.
- ↑ Schwarz HP, Fischer M, Hopmeier P, Batard MA, Griffin JH (1984). "Plasma protein S deficiency in familial thrombotic disease". Blood. 64 (6): 1297–300. PMID 6238642.
- ↑ Simmonds RE, Ireland H, Kunz G, Lane DA (1996). "Identification of 19 protein S gene mutations in patients with phenotypic protein S deficiency and thrombosis. Protein S Study Group". Blood. 88 (11): 4195–204. PMID 8943854.
- ↑ Gandrille S, Borgel D, Eschwege-Gufflet V, Aillaud M, Dreyfus M, Matheron C; et al. (1995). "Identification of 15 different candidate causal point mutations and three polymorphisms in 19 patients with protein S deficiency using a scanning method for the analysis of the protein S active gene". Blood. 85 (1): 130–8. PMID 7803790.
- ↑ Esmon CT (1992). "Protein S and protein C Biochemistry, physiology, and clinical manifestation of deficiencies". Trends Cardiovasc Med. 2 (6): 214–9. doi:10.1016/1050-1738(92)90027-P. PMID 21239244.
- ↑ "Protein C - Wikipedia".
- ↑ Pintao MC, Ribeiro DD, Bezemer ID, Garcia AA, de Visser MC, Doggen CJ; et al. (2013). "Protein S levels and the risk of venous thrombosis: results from the MEGA case-control study". Blood. 122 (18): 3210–9. doi:10.1182/blood-2013-04-499335. PMID 24014240.