Sandbox:Retropharyngeal abscess
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Vishal Devarkonda, M.B.B.S[2]
Synonyms and keywords:
Overview
Historical Perspective
- The exact origins of the disease is not clearly known. The term abscess is derived from latin term abscessus(meaning: act of going away)
- In 1926, Guthrie described a case of retropharyngeal abscess in childhood.
- In 1946, Davidson described a case of retrophayngeal abscess in adults.
Classification
There is no established classification system for retropharyngeal abscess. hsiukhiwusn
Pathophysiology
Pathophysiology:[1][2][3][4][5][6][7][8][9][10]
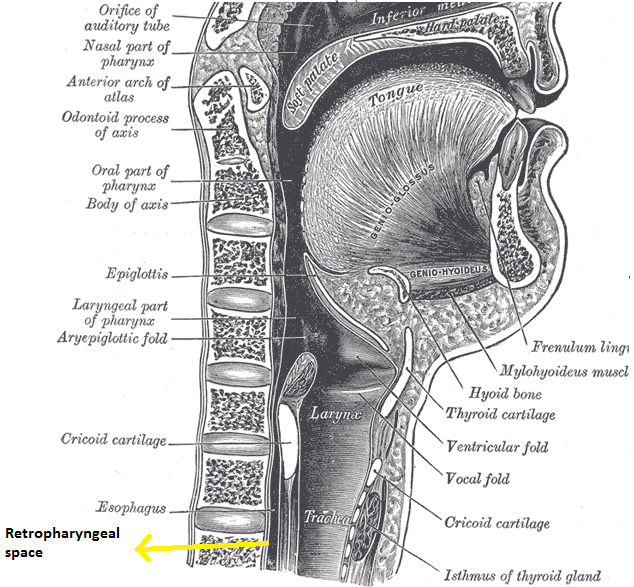
Retropharyngeal space is a deep space in neck extending from the base of skull to the posterior mediastinum. Space is bordered anteriorly by middle layer of the deep cervical fascia(buccopharyngeal fascia), posteriorly by deep layer of deep cervical fascia, laterally by the carotid sheath which contain carotid artery and jugular vein.
The pathophysiology of retropharyngeal abscess can be discussed in following headings:
Transmission
Transmission of the infection to the retropharyngeal space could be by trauma, lymphatic spread or by direct spread.
| Mode of transmission of infection to retropharyngeal space | |
|---|---|
| Lymphatic spread | Retropharyngeal space consists two pair of lymphnodes, which drains nasopharynx, adenoids, posterior paranasal sinuses, middle ear, and eustachian tube. Draining infected can be infected following the upper respiratory tract infection. Lymph node may undergo liquefaction necrosis, which my progress into retropharyngeal cellulitis, which left intreated can progress to abscess formation. However by age 4 years, these lymph node undergo spontaneous atrophy. |
| Direct spread/ Trauma | Adults
In adults, retropharyngeal space can be contaminated by direct trauma(eg, penetrating foreign trauma, endoscopy, dental procedures) or extension of local infection such as odontogenic infection, ludwig's angina, or osteomyelitis of cervical spine Children In children, retropharyngeal space can be contaminated by direct trauma to oropharynx(swallowing a foreign body or running and falling with an object in the mouth). |
Immune response
Introduction of infections into retropharyngeal space either through lymphatic spread or direct spread may lead to suppurative adenitis of retropharyngeal lymph nodes or cellulitis of retropharyngeal space. Cellulitis may progress to form phlegmon, which inturn progress to mature abscess.
Causes
Polymicrobial infection is often responsible for retropharyngeal abscess. The other organisms involved in causes in retropharyngeal abscess include:[1][2][11][12][13][14][15]
Most common causes
- Polymicrobial infections
- Beta-hemolytic streptococcus
- Streptococcus pyogenes (group A streptococcus [GAS])
- Staphylococcus aureus (including methicillin-resistant S. aureus [MRSA]),
- Fusobacteria
- Prevotella
- Veillonella
Less common causes
- Haemophilus Influenzae
- Haemophilus parainfluenzae
- Neisseria species
- Bacteroides
- Fusoabacterium
- Salmonella
- Mycobacterium
- Bartonella henselae
- Porphyromonas species
Epidemiology and Demographics
Epidemiology:
Incidence
There are no comprehensive studies studying the incidence of Retropharyngeal abscess worldwide.
In United states, incidence of retrophyrangeal abscess in kids under age 20 years is 4.10 per 100,000 population for year 2012.
Case Fatality Rate
- There are no comprehensive studies studying the case fatality rate of Retropharyngeal abscess worldwide.
- Few studies have reported case fatality from a low of no fatalities(after reviewing the data from 1321 pediatric admissions with retropharyngeal abscess in year 2003) to high of 2.6%(234 adults with deep space neck infections in adults)
Age
Retropahyngeal abscess commonly affects children, median age being 4 years for children.
Gender
Retropharyngeal abscess is more commonly affects in males than in females. The gender ratio is approximately 1.63.
Race
In year 2015, comprehensive study analysed the 2685 hospital discharges for Parapharyngeal abscess and 6233 hospital discharges for retropharyngeal abscess and reported that for 2012 49.5% were white, 19.2% were black, 21.9 % were hispanic and 9.5% were other race(retro).
Screening
There are no established screening guidelines to screen patient for retropharyngeal abscess.
Natural History, Complications, and Prognosis
Natural history
If appropriate medial or surgical interventions is delayed or left untreated, patients with retropharyngeal abscess may develop life threatening complications which include mediastnitis, sepsis and internal jugular vein thrombophlebitis.
Complications
Complications of retropharyngeal abscess include:
- Epidural abscess
- Mediastinitis
- Carotid artery aneurysm or erosion
- Internal jugular vein thrombophlebitis
- Septic pulmonary embolism
- Cranial nerve dysfunction (IX–XII)
- Cavernous sinus thrombosis
- Aspiration pneumonia
- Life-threatening descending necrotizing mediastinitis
- Sepsis
Prognosis
The prognosis of retropharyngeal abscess is good when detected early and appropriately treated. Relapse may occur in 1 to 5 percent of cases
Diagnosis
History and symptoms
Patients with retropharyngeal abscess may present with:
- Pain in neck
- Fever
- Sore throat
- Mass in neck
- Respiratory distress(stridor)
- Difficulty swallowing (dysphagia)
- Pain with swallowing (odynophagia)
- Unwillingness to move the neck(torticollis)
- Change in voice
- reduced opening of the jaws(Trismus)
- Chest pain
Physical examination
Role of physical examination in diagnosing the retro pharyngeal abscess is limited, as most of the patients aren't able to open the mouth widely.
Patients with suspected retropharyngeal abscess should be examined in a head-down position(trendelenburg) position. It is recommended to perform examination in operation room as it permits to place an aritifical airway if necessary. A midline or unilateral swelling of the posterior pharyngeal wall can be appreciated.
Other physical examination findings include
- Tender anterior cervical lymphadenopathy
- Palpable neck mass
Laboratory findings
Laboratory findings may show non-specific leukocytosis.
Imaging
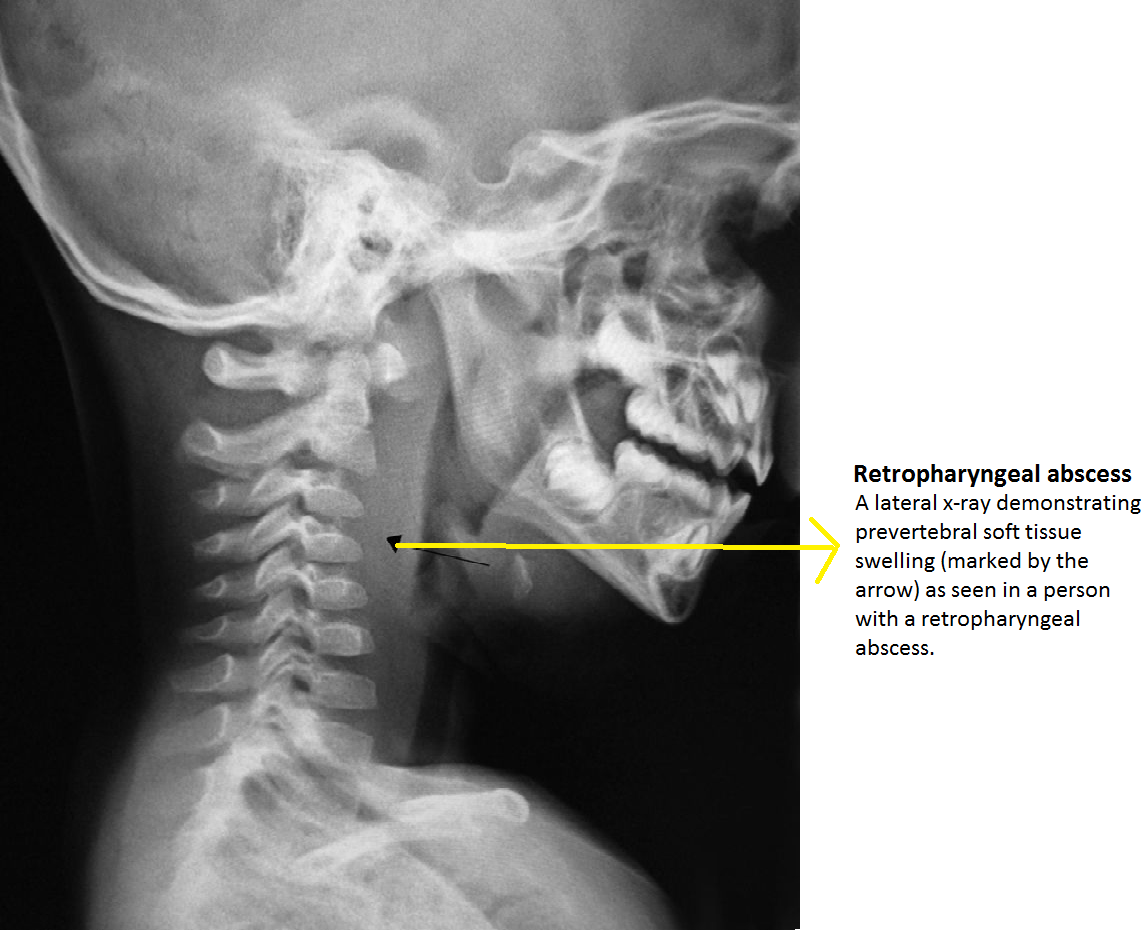
Diagnosis of retropharyngeal abscess should be ultimately supported by radiographic imaging. In suspected patients, an initial lateral and anterio-posterior X-ray of neck should be ordered, which is usually followed with CT scan of the neck with IV contrast. Ct scan not only helps in diagnosing the retropharyngeal abscess but also helps in identifying the position of carotid artery and internal jugular vein in relation to the infectious process.
Plain X-ray
Lateral neck X ray demonstrate thickening of soft tissue with possible gas-fluid levels in the pre-vertebral cervical space.
Pathological widening of retropharyngeal space should be considered if it is greater than 22 mm at C6 in adults and 7 mm at C2 or 14 mm at C6 in children.
Other X ray findings include:
- Reversal of the normal cervical lordosis
- Radiopaque foreign body
- Soft-tissue mass
CT scan
Patients with retropharyngeal abscess, abscess may appear as
- Mass impinging on the posterior pharyngeal wall
- Complete rim enhancement with scalloping is indicative of an abscess
- Low density core, soft tissue swelling, obliterated fat planes are other common CT scan associated with retropharyngeal abscess
Management
There are no comprehensive randomized controlled studies evaluating the management of retropharyngeal infections. Patients should be ideally hospitalized in a setting where intubation or tracheotomy easily accessible in case if there is a respiratory compromise. Management predominantly consists of empiric intravenous antibiotics or combination of surgical drainage and intravenous antibiotics. During hospitalization patient should be regularly monitored for airway patency, hydration status and for potential complications.
Children
Combination of surgical drainage and intravenous antibiotics
Widely accepted indications for surgical drainage of abscess include: airway compromise, or failure to response after 24-24 hrs of administration of empiric anti microbial therapy, or CT scan showing large (>3 cm2) hypodense area(Indicative of mature abscess) or life-threatening complication. Drainage fluid should be sent for culture and sensitivity, for choosing appropriate antibiotics for further management.
Medical therapy
Trail of antimicrobial therapy for initial 24 to 48 hours without surgical drainage should be considered in patients who do not have airway compromise, CT scan showing cross-sectional hypodense area between <2 to 3 cm2 and no life-threatening complications.
Empiric intravenous antibiotic include:
- Ampicillin-sulbactam (50 mg/kg per dose every six hours intravenously), or Clindamycin (15 mg/kg per dose [maximum single dose 900 mg]every eight hours intravenously).
- In patients with moderate or severe disease who do not respond to empiric therapy, additional intravenous Vancomycin (40 to 60 mg/kg per day divided in three to four doses; maximum daily dose 2 to 4 g or Linezolid (<12 years: 30 mg/kg per day divided in three doses; ≥12 years: 20 mg/kg per day in two doses; maximum daily dose 1200 mg) should be considered to optimize the converage againist Gram-positive cocci.
- Once the patients is afebrile and shows signs of clinical improvement a 14 day oral antimicrobial therapy with either Amoxicillin-clavulanate (45 mg/kg per dose every 12 hours), or Clindamycin (13 mg/kg per dose every 8 hours) should be prescribed.
- Antimicrobial therapy should be adequately supplemented with analgesics, antipyretics and intravenous fluids.
Discharge instructions
Patients should be asked to report to the health care provider if the notice any new onset of enlarging mass, difficulty in breathing, worsening pain, fever and any stiffness in neck.
Adults
Combination of surgical drainage and intravenous antibiotics
Widely accepted indications for surgical drainage of abscess include: airway compromise, or failure to response after 24-24 hrs of administration of empiric anti microbial therapy, or CT scan showing large volume abscess or life-threatening complication. Drainage fluid should be sent for culture and sensitivity, for choosing appropriate antibiotics for further management.
Medical therapy
Trail of antimicrobial therapy for initial 24 to 48 hours without surgical drainage should be considered in patients who do not have airway compromise, CT scan showing small volume abscess and no life-threatening complications.
| Antibiotics regimen coverage for deep neck space infections[16] | |
|---|---|
| Antibiotics regimen | Coverage rate (%) |
| Ceftriaxone, clindamycin | 76.40% |
| Ceftriaxone, metronidazole | 70.79% |
| Cefuroxime, clindamycin | 61.80% |
| Penicillin G, metronidazole | 16.85% |
| Penicillin, gentamicin, clindamycin | 67.42% |
Preferred medical therapies
Preferred medical therapy 1
Amipicillin-sulbactam(3 g IV every six hours)
Preferred medical therapy 2
Penicillin G (2 to 4 MU IV every four to six hours) plus metronidazole (500 mg IV every six to eight hours)
Preferred medical therapy 3
Clindamycin (600 mg IV every six to eight hours)
Preferred medical therapy 4
Ceftriaxone 1 g IV every 24 hours plus metronidazole 500 mg IV every six to eight hours
Preferred medical therapy 5
Ciprofloxacin (400 mg IV every 12 hours) plus clindamycin (600 mg IV every six to eight hours)
- In patients with moderate or severe disease or having MRSA risk factors(higher incidence of MRSA in hospital and community, IV drug abuse or comorbid conditions like Diabetes mellitus, living in crowed places) or who do not respond to empiric therapy, additional intravenous vancomycin (15 to 20 mg/kg IV every 12 hours) or linezolid (600 mg orally or IV every 12 hours) should be considered to optimize the converage againist Gram-positive cocci.
- Antimicrobial therapy should be adequately supplemented with analgesics, antipyretics and intravenous fluids.
Duration
Once the patients is afebrile and shows signs of clinical improvement IV antibiotics can be replaced with oral antibiotics. Oral antibiotics should be continued for 2-3 weeks after discharge to prevent recurrence or complications.
Prevention
Primary Prevention
There are no established primary preventive measures for preventing retropharyngeal abscess
Secondary prevention
There are no established secondary prevention measures, but early detection and appropriate medical and surgical intervention can help in early recovery and prevention of complications.
References
- ↑ 1.0 1.1 Asmar BI (1990). "Bacteriology of retropharyngeal abscess in children". Pediatr Infect Dis J. 9 (8): 595–7. PMID 2235179.
- ↑ 2.0 2.1 McClay JE, Murray AD, Booth T (2003). "Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography". Arch Otolaryngol Head Neck Surg. 129 (11): 1207–12. doi:10.1001/archotol.129.11.1207. PMID 14623752.
- ↑ Ungkanont K, Yellon RF, Weissman JL, Casselbrant ML, González-Valdepeña H, Bluestone CD (1995). "Head and neck space infections in infants and children". Otolaryngol Head Neck Surg. 112 (3): 375–82. PMID 7870436.
- ↑ Page NC, Bauer EM, Lieu JE (2008). "Clinical features and treatment of retropharyngeal abscess in children". Otolaryngol Head Neck Surg. 138 (3): 300–6. doi:10.1016/j.otohns.2007.11.033. PMID 18312875.
- ↑ Philpott CM, Selvadurai D, Banerjee AR (2004). "Paediatric retropharyngeal abscess". J Laryngol Otol. 118 (12): 919–26. PMID 15667676.
- ↑ Poluri A, Singh B, Sperling N, Har-El G, Lucente FE (2000). "Retropharyngeal abscess secondary to penetrating foreign bodies". J Craniomaxillofac Surg. 28 (4): 243–6. doi:10.1054/jcms.2000.0151. PMID 11110158.
- ↑ Sethi DS, Chew CT (1991). "Retropharyngeal abscess--the foreign body connection". Ann Acad Med Singapore. 20 (5): 581–8. PMID 1781639.
- ↑ Singh B, Kantu M, Har-El G, Lucente FE (1997). "Complications associated with 327 foreign bodies of the pharynx, larynx, and esophagus". Ann Otol Rhinol Laryngol. 106 (4): 301–4. doi:10.1177/000348949710600407. PMID 9109720.
- ↑ Morrison JE, Pashley NR (1988). "Retropharyngeal abscesses in children: a 10-year review". Pediatr Emerg Care. 4 (1): 9–11. PMID 3283710.
- ↑ Gaglani MJ, Edwards MS (1995). "Clinical indicators of childhood retropharyngeal abscess". Am J Emerg Med. 13 (3): 333–6. doi:10.1016/0735-6757(95)90214-7. PMID 7755832.
- ↑ Wright CT, Stocks RM, Armstrong DL, Arnold SR, Gould HJ (2008). "Pediatric mediastinitis as a complication of methicillin-resistant Staphylococcus aureus retropharyngeal abscess". Arch Otolaryngol Head Neck Surg. 134 (4): 408–13. doi:10.1001/archotol.134.4.408. PMID 18427007.
- ↑ Brook I (2004). "Microbiology and management of peritonsillar, retropharyngeal, and parapharyngeal abscesses". J Oral Maxillofac Surg. 62 (12): 1545–50. PMID 15573356.
- ↑ Inman JC, Rowe M, Ghostine M, Fleck T (2008). "Pediatric neck abscesses: changing organisms and empiric therapies". Laryngoscope. 118 (12): 2111–4. doi:10.1097/MLG.0b013e318182a4fb. PMID 18948832.
- ↑ Abdel-Haq N, Quezada M, Asmar BI (2012). "Retropharyngeal abscess in children: the rising incidence of methicillin-resistant Staphylococcus aureus". Pediatr Infect Dis J. 31 (7): 696–9. doi:10.1097/INF.0b013e318256fff0. PMID 22481424.
- ↑ Cheng J, Elden L (2013). "Children with deep space neck infections: our experience with 178 children". Otolaryngol Head Neck Surg. 148 (6): 1037–42. doi:10.1177/0194599813482292. PMID 23520072.
- ↑ Yang SW, Lee MH, See LC, Huang SH, Chen TM, Chen TA (2008). "Deep neck abscess: an analysis of microbial etiology and the effectiveness of antibiotics". Infect Drug Resist. 1: 1–8. PMC 3108716. PMID 21694873.