ST elevation myocardial infarction electrocardiogram
| Myocardial infarction electrocardiogram | |
 | |
|---|---|
| Illustration of ST segment elevation with measurement of the magnitude of ST elevation 60 milliseconds after the J point. | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
A primary purpose of the electrocardiogram is to detect ischemia or acute coronary injury in broad, symptomatic emergency department populations. The 12 lead ECG is used to classify patients into one of three groups:
- Those with ST segment elevation or new bundle branch block (suspicious for acute injury and a possible candidate for acute reperfusion therapy with thrombolytics or primary PCI),
- Those with ST segment depression or T wave inversion (suspicious for ischemia), and
- Those with a so-called non-diagnostic or normal ECG.[1]
A normal ECG does not rule out the presence of acute myocardial infarction. Sometimes the earliest presentation of acute myocardial infarction is instead the hyperacute T wave.[2] In clinical practice, hyperacute T waves are rarely seen, because they exists for only 2-30 minutes after the onset of infarction.[3] Hyperacute T waves need to be distinguished from the peaked T waves associated with hyperkalemia.[4]
Definition of ST Elevation
The current guidelines for the ECG diagnosis of acute myocardial infarction require at least 1 mm (0.1 mV) of ST segment elevation in 2 or more anatomically contiguous leads.[1] This criterion is problematic, however, as acute myocardial infarction is not the most common cause of ST segment elevation in chest pain patients.[5]
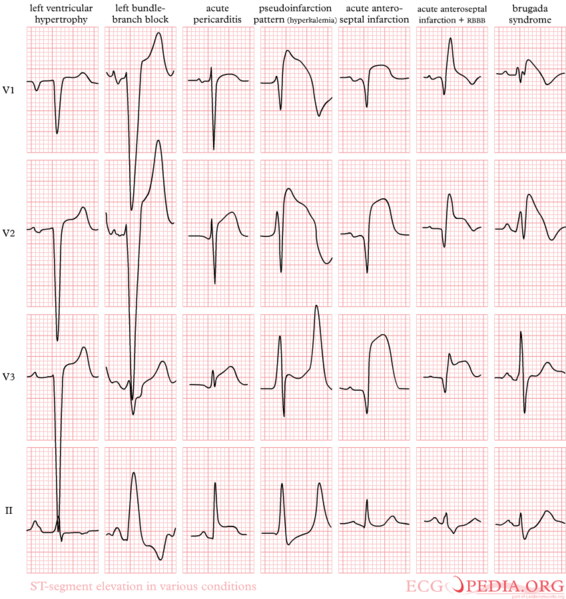
Differential Diagnosis of Causes of ST Segment Elevation in the Absence of Myonecrosis
ST Segment Elevation Does Not Always Signify a Myocardial Infarction. ST segment elevation should alert the clinician to the possibility of myocardial injury, however, there are a variety of conditions that cause ST segment elevation which are not associated with myonecrosis. Indeed, over 90% of healthy men have at least 1 mm (0.1 mV) of ST segment elevation in at least one precordial lead.[6] The clinician must therefore be well versed in recognizing the so-called ECG mimics of acute myocardial infarction, which include left ventricular hypertrophy, left bundle branch block, paced rhythm, benign early repolarization, pericarditis, hyperkalemia, and ventricular aneurysm.[7][8][6]
Left bundle branch block and pacing can interfere with the electrocardiographic diagnosis of acute myocadial infarction. The GUSTO investigators Sgarbossa et al. developed a set of criteria for identifying acute myocardial infarction in the presence of left bundle branch block and paced rhythm. They include concordant ST segment elevation > 1 mm (0.1 mV), discordant ST segment elevation > 5 mm (0.5 mV), and concordant ST segment depression in the left precordial leads.[9] The presence of reciprocal changes on the 12 lead ECG may help distinguish true acute myocardial infarction from the mimics of acute myocardial infarction. The contour of the ST segment may also be helpful, with a straight or upwardly convex (non-concave) ST segment favoring the diagnosis of acute myocardial infarction.[10]
Acute epicardial artery occlusion by thrombus is certainly one cause of ST segment elevation, but other causes of ST segment elevation which are not associated with myonecrosis include the following: (listed in alphabetical order) [11] [12]
- Aneurysm of the ventricle can result in persistent ST segment elevation that can be exacerbated with tachycardia.
- Balloon inflation in a coronary artery during percutaneous coronary intervention
- Coronary artery rupture during percutaneous coronary intervention
- Early repolarization is a normal variant that can result in ST segment elevation. It is more common in males of younger age. The ST elevation is exacerbated by bradycardia.
- Hyperkalemia known as the "dialyzable current of njury" hyperkalemia may cause hyperacute ECG changes due to changes in membrane polarity
- Left bundle branch block is associated with ST segment elevation in those leads that are discordant to the QRS. Stated differently, if the QRS is predominantly of a negative deflection, it is normal to observe ST segment elevation in the same leads. The presence of ST elevation in leads where the QRS deflection is upright (concordance) may be a marker of myocardial injury.
- Myopericarditis can cause injury to the subepicardial myocytes and ST segment elevation.
- Myocarditis can cause injury to the subepicardial myocytes and ST segment elevation.
- Pericardiocentesis when the needle comes into contact with the myocardium, there can be ST segment elevation reflecting local injury of the myocardium.
- Pericarditis can cause injury to the subepicardial myocytes and ST elevation.
- Prinzmetal's angina is associated with ST segment elevation due to transient epicardial coronary artery spasm either in the absence or presence of atherosclerosis. If the condition persists long enough, myonecrosis can be observed.
- Stroke Intracranial hemorrhage can in some cases cause ST segment elevation due to direct myocyte injury from a hyperadrenergic stimulation emanating from the central nervous system.
Differential Diagnosis of Causes of ST Segment Elevation in the Presence of Myonecrosis (STEMI)
While plaque rupture is the most common cause of ST segment elevation MI, other conditions can cause ST elevation and myocardial necrosis. In order to expeditiously treat an alternate underlying cause of myonecrosis, it is important to rpadily identify conditions other than plaque rupture that may also cause ST elevation and myonecrosis. Indeed, the management of some of these conditions might be differ substantially from that of plaque rupture: cocaine induced STEMI would not be treated with beta-blockers, and myocardial contusion would not be treated with an antithrombin. These conditions include the following:
| Cardiovascular | Aortic dissection more often extends to occlude the ostium of the right coronary artery
Aortic stenosis can cause subendocardial ischemia and infarction if demand grossly exceeds supply
|
| Chemical / poisoning | Carbon monoxide poisoning |
| Dermatologic | No underlying causes |
| Drug Side Effect | Oral contraceptive pills, particularly among women who smoke |
| Ear Nose Throat | A recent upper respiratory tract infections has been associated with a 4.9 fold rise in the risk of MI |
| Endocrine | Thyrotoxicosis |
| Environmental | Blizzards and snow shoveling, and inhalation of fine particulate matter in areas with air pollution and high traffic have been identified as triggers of MI. |
| Gastroenterologic | A heavy meal has been associated with a 4 fold rise in the risk of MI, and it is not clear if this is mediated by hyperadrenergic tone [13]; |
| Genetic | Familial hypercholesterolemia |
| Hematologic | Disseminated intravascular coagulation (DIC) |
| Iatrogenic | Epinephrine overdose
Sudden withdrawal of Beta blockers or nitrates |
| Infectious Disease | A recent upper respiratory tract infections has been associated with a 4.9 fold rise in the risk of MI
Infectious endocarditis may STEMI as a result of embolization |
| Musculoskeletal / Ortho | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional / Metabolic | A heavy meal has been associated with a 4 fold rise in the risk of MI and it is not clear if this is mediated by hyperadrenergic tone [14];
Mucopolysaccharidoses or Hurler disease Thiamine deficiency has been associated with ST elevation and myonecrosis [15] [16] [17] |
| Obstetric/Gynecologic | Spontaneous coronary dissection in the setting of pregnancy |
| Oncologic | Radiation therapy can accelerate atherosclerosis particularly in the distribution of the left anterior descending artery; |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | Cocaine ingestion which may result in direct myocyte injury due to an adrendergic surge, vasoconstriction of the microvasculature or plaque rupture and thrombus formation;
Marijuana ingestion has been identified as a trigger of MI. |
| Psychiatric | Anger, anxiety, bereavement, work-related stress, earthquakes, bombings and other psychosocial stressors have been identified as triggers of MI, and it is not clear if the mechanism is plaque rupture or hyperadrenergic tone;
Stress cardiomyopathy or Broken heart syndrome causes ST segment elevation most often in the anterior precordium and is thought to be due to direct myocyte injury from a hyperadrenergic stimulation emanating from the central nervous system. |
| Pulmonary | A recent upper respiratory tract infections has been associated with a 4.9 fold rise in the risk of MI |
| Renal / Electrolyte | Homocystinuria |
| Rheum / Immune / Allergy | Takayasus |
| Sexual | Sexual activity has been identified as a trigger of MI |
| Trauma | Both penetrating and non-penetrating trauma to the heart or myocardial contusion, commotio cordis can be associated with ST elevation and myonecrosis. |
| Urologic | No underlying causes |
| Miscellaneous | Hypotension particularly if it is prolonged |
Limitations of the 12 lead ECG
However, the standard 12 lead ECG has several limitations. An ECG represents a brief sample in time. Because unstable ischemic syndromes have rapidly changing supply versus demand characteristics, a single ECG may not accurately represent the entire picture. It is therefore desirable to obtain serial 12 lead ECGs, particularly if the first ECG is obtained during a pain-free episode. Alternatively, many emergency departments and chest pain centers use computers capable of continuous ST segment monitoring.[18] It should also be appreciated that the standard 12 lead ECG does not directly examine the right ventricle, and does a relatively poor job of examining the posterior basal and lateral walls of the left ventricle. In particular, acute myocardial infarction in the distribution of the circumflex artery is likely to produce a nondiagnostic ECG. The use of non-standard ECG leads like right-sided lead V4R and posterior leads V7, V8, and V9 may improve sensitivity for right ventricular and posterior myocardial infarction. In spite of these limitations, the 12 lead ECG stands at the center of risk stratification for the patient with suspected acute myocardial infarction. Mistakes in interpretation are relatively common, and the failure to identify high risk features has a negative effect on the quality of patient care.[19]
Localization of the infarct using the 12 lead ECG
The constellation of leads with ST segment elevation enables the clinician to identify what area of the heart is injured, which in turn helps predict the so-called culprit artery.
As the myocardial infarction evolves, there may be loss of R wave height and development of pathological Q waves. T wave inversion may persist for months or even permanently following acute myocardial infarction.[20] Typically, however, the T wave recovers, leaving a pathological Q wave as the only remaining evidence that an acute myocardial infarction has occurred.

| Figure | change | |
|---|---|---|
| minutes | 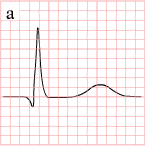
|
hyperacute T waves (peaked T waves)
ST-elevation |
| hours | 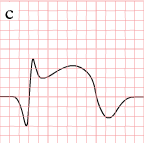
|
ST-elevation, with terminal negative T wave
negative T wave (these can last for months) |
| days | 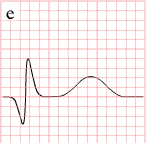
|
Pathologic Q Waves |
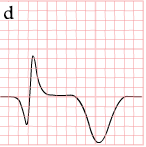
Measurement of the Magnitude of ST Elevation: 60 Milliseconds after the J point

The optimal time after the J point to measure ST elevation is debated. This example shows the technique of measuring the magnitude of ST elevation 60 milliseconds or 1.5 small boxes after the J point.
Distinguishing Early Repolarization and Other Normal Variants from Pathologic ST Elevation

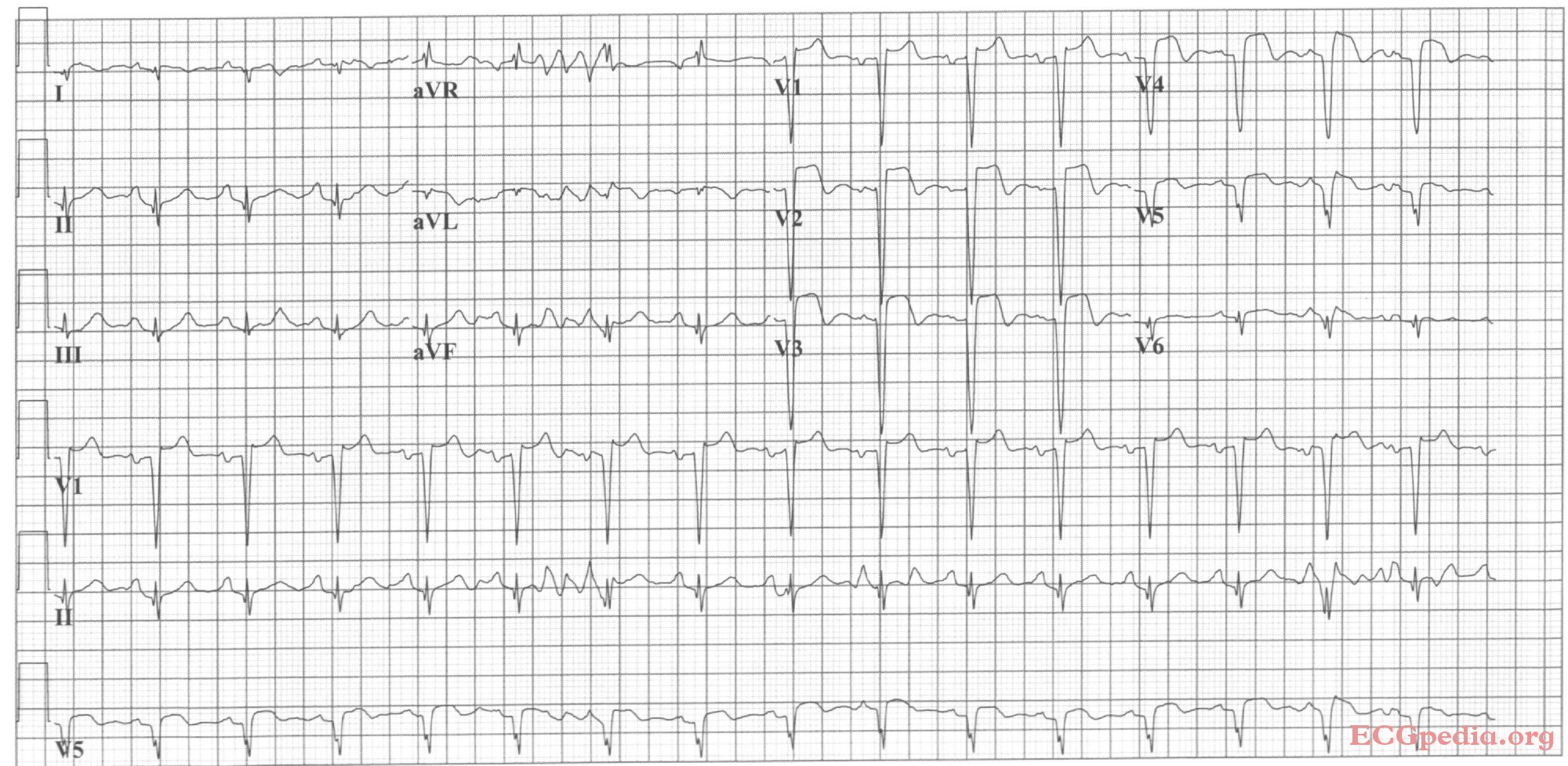
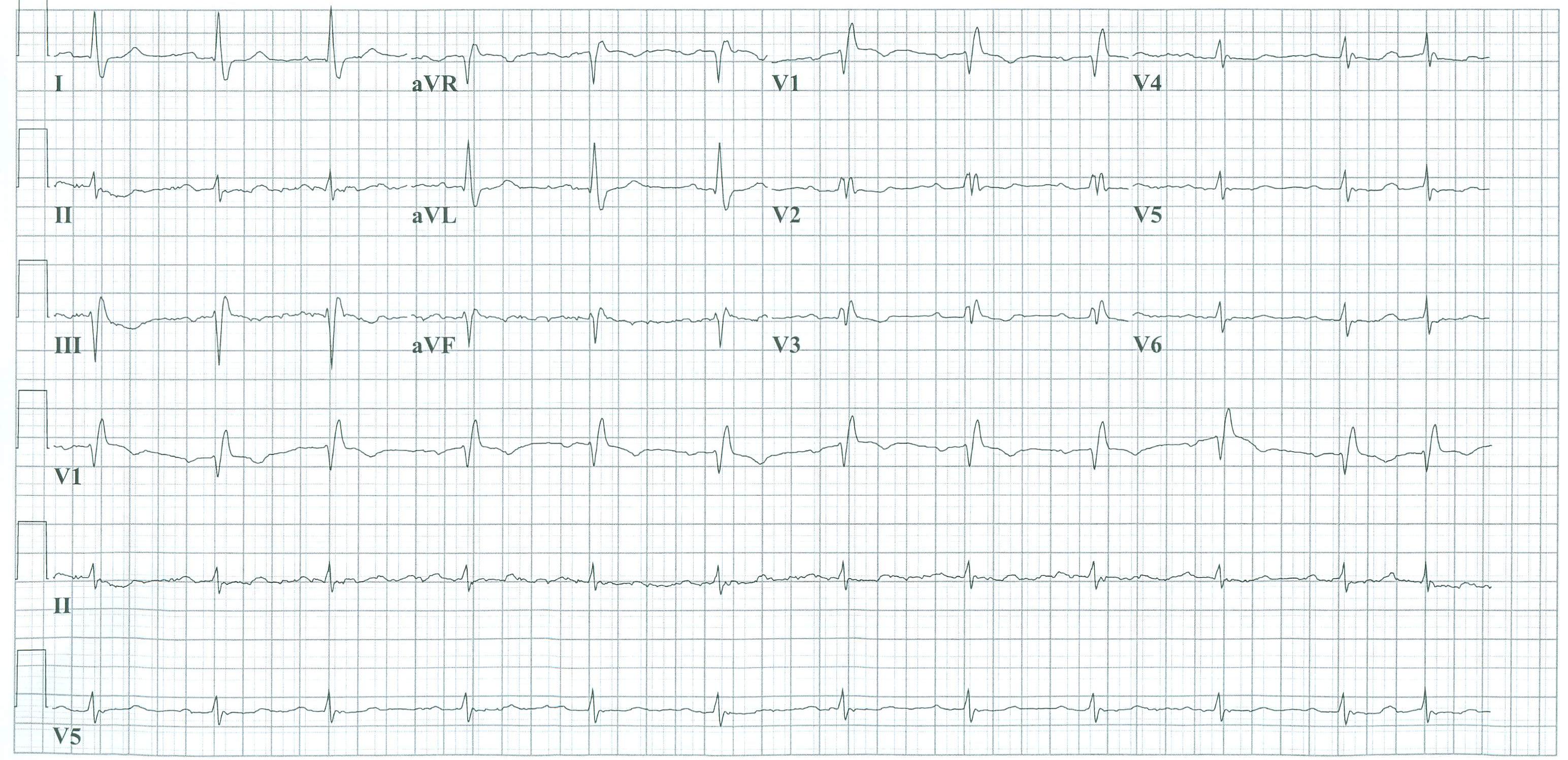
EKG Examples
-
The evolution of an infarct on the ECG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave
-
Pathologic ST elevation
-
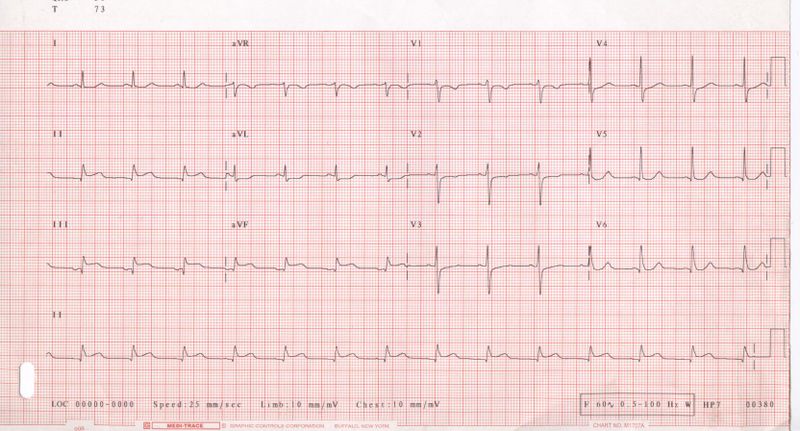
12-lead electrocardiogram (ECG) showing acute inferior ST segment elevation MI (STEMI). Note the ST segment elevation in leads II, III, and aVF along with reciprocal ST segment depression in leads I and aVL.
-
Acute inferior myocardial infarction with RV involvement.
-
Acute inferoposterior MI: ST elevation in II, III, AVF (in III > II). ST depression in I, AVL, V2. Tall R in V2, otherwise normal QRS morphology.
-
Acute inferior MI
-
Acute posterolateral MI
-
Acute inferolateral MI: ST depression in V1, V4, tall R in V2. ST elevation in II, III, AVF, V5 and V6.
-
Acute anterior MI. Loss of R waves throughout the anterior wall (V1-V6). QS complexes in V3-V5. ST elevation in V1-V5 with terminal negative T waves.
-
Sinus bradycardia with first degree AV block and inferior-posterior-lateral myocardial infarction.
-
Sinus bradycardia with inferior-lateral myocardial infarction.
-
Acute anterior MI. LAD artery occlusion
-
Sinus rhythm with anteroseptal myocardial infarction.
-
Sinus rhythm with left bundle branch block, comparison with an old EKG is mandatory to evaluate whether the LBBB is new (a sign of myocardial infarction) or old.
-
Inferior-posterior myocardial infarction with complete AV block and ventricular excape rhythm with RBBB pattern and left axis, followed by sinus rhythm.
-
Acute anterior myocardial infarction and left anterior hemiblock. Image courtesy of Dr Jose Ganseman
-
Old anterior myocardial infarction and bifascicular block (RBBB and LAHB) Image courtesy of Dr Jose Ganseman
-
Acute MI with proximal LAD occlusion
-
A 2 days old anterior infarction with Q waves in V1-V4 with persisting ST elevation, a sign of left ventricular aneurysm formation.
-
A 2 weeks old anterior infarction with Q waves in V2-V4 and persisting ST elevation, a sign of left ventricular aneurysm formation.
-
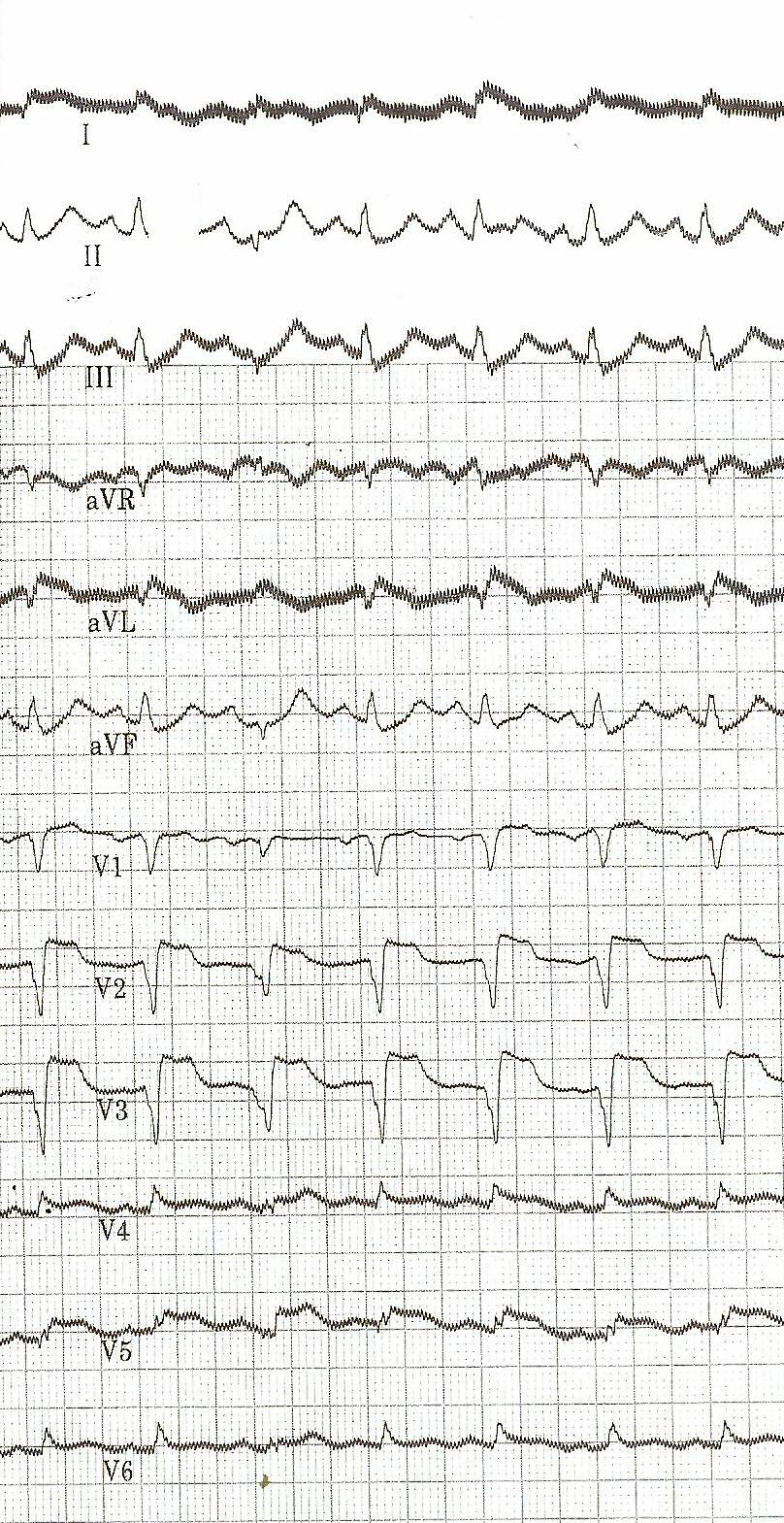
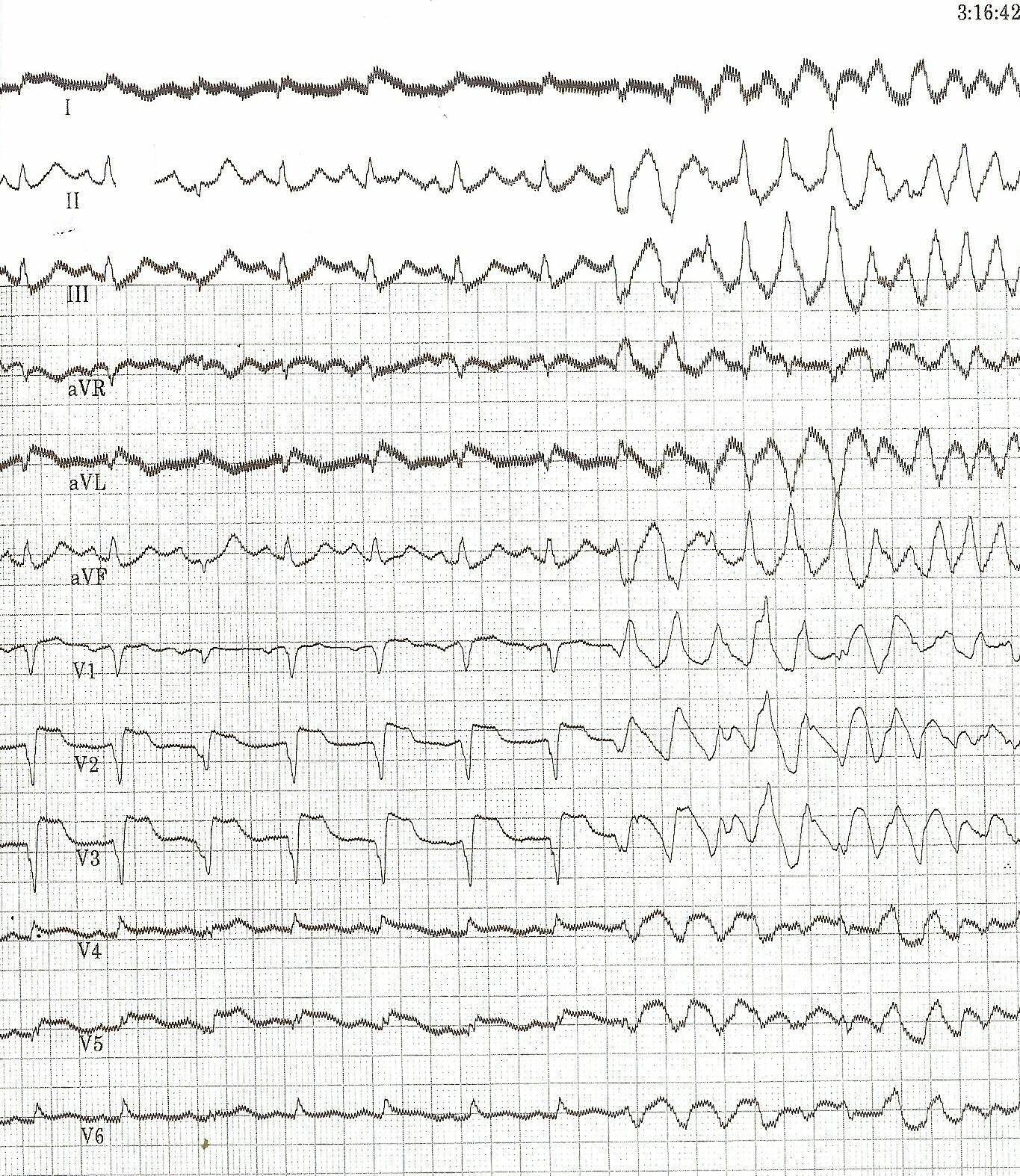
The heart rate increases and there are two extra systoles short after each other. Then, a chaotic rhythm develops: ventricular fibrillation.
-
Atrial fibrillation and inferior-posterior myocardial infarction.
-
Same patient's 2. EKG; This EKG shows clear ST elevation in the right precordial leads. A coronary angiography revealed a proximal right coronary artery occlusion.
-
Inferior-posterior-lateral myocardial infarction with a nodal escape rhythm
-
The same patient before acute MI developed. Horizontal axis.
-
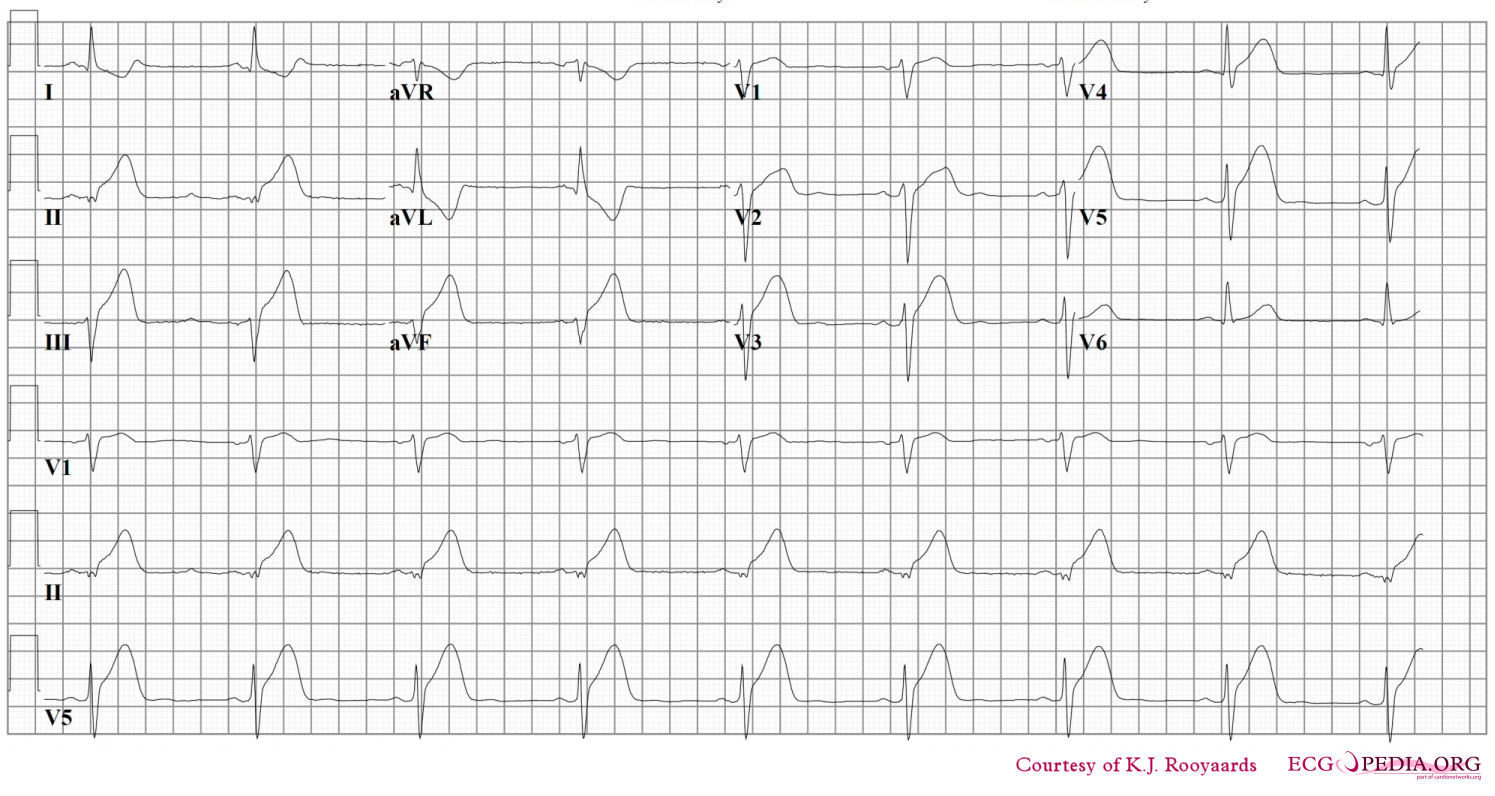
Acute myocardial infarction in in a patient with a pacemaker and LBBB. Concordant ST elevation in V5-V6 are clearly visible. There is discordant ST segment elevation > 5 mm in lead V3.
-
Atrial fibrillation with inferior-posterior-lateral myocardial infarction and incomplete right bundle branch block. Lead I shows ST depression, suggestive of right coronary artery involvement.
| Wall Affected | Leads Showing ST Segment Elevation | Leads Showing Reciprocal ST Segment Depression | Suspected Culprit Artery |
|---|---|---|---|
| Septal | V1, V2 | None | Left Anterior Descending (LAD) |
| Anterior | V3, V4 | None | Left Anterior Descending (LAD) |
| Anteroseptal | V1, V2, V3, V4 | None | Left Anterior Descending (LAD) |
| Anterolateral | V3, V4, V5, V6, I, aVL | II, III, aVF | Left Anterior Descending (LAD), Circumflex (LCX), or Obtuse Marginal |
| Extensive anterior (Sometimes called Anteroseptal with Lateral extension) | V1,V2,V3, V4, V5, V6, I, aVL | II, III, aVF | Left main coronary artery (LCA) |
| Inferior | II, III, aVF | I, aVL | Right Coronary Artery (RCA) or Circumflex (LCX) |
| Lateral | I, aVL, V5, V6 | II, III, aVF | Circumflex (LCX) or Obtuse Marginal |
| Posterior (Usually associated with Inferior or Lateral but can be isolated) | V7, V8, V9 | V1,V2,V3, V4 | Posterior Descending (PDA) (branch of the RCA or Circumflex (LCX)) |
| Right ventricular (Usually associated with Inferior) | II, III, aVF, V1, V4R | I, aVL | Right Coronary Artery (RCA) |
References
- ↑ 1.0 1.1 "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 8: Stabilization of the Patient With Acute Coronary Syndromes." Circulation 2005; 112: IV-89 - IV-110.
- ↑ Somers MP, Brady WJ, Perron AD, Mattu A. "The prominent T wave: electrocardiographic differential diagnosis." Am J Emerg Med 2002; 20(3): 243-51. PMID 11992348
- ↑ Smith SW, Whitwam W. "Acute Coronary Syndromes." Emerg Med Clin N Am 2006; 24(1): 53-89. PMID 16308113
- ↑ "The clinical value of the ECG in noncardiac conditions." Chest 2004; 125(4): 1561-76. PMID 15078775
- ↑ Brady WJ, Perron AD, Martin ML, Beagle C, Aufderheide TP. "Cause of ST segment abnormality in ED chest pain patients." Am J Emerg Med 2001; 19(1): 25-8. PMID 11146012
- ↑ 6.0 6.1 Wang K, Asinger RW, Marriott HJ. "ST-segment elevation in conditions other than acute myocardial infarction." New Engl J Med 2003; 349(22): 2128-35. PMID 14645641
- ↑ Brady WJ, Chan TC, Pollack M. "Electrocardiographic manifestations: patterns that confound the EKG diagnosis of acute myocardial infarction-left bundle branch block, ventricular paced rhythm, and left ventricular hypertrophy." J Emerg Med 2000; 18(1): 71-8. PMID 10645842
- ↑ "Electrocardiographic ST-segment elevation: correct identification of acute myocardial infarction (AMI) and non-AMI syndromes by emergency physicians." Acad Emerg Med 2001; 8(4): 349-60. PMID 11282670
- ↑ Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS. "Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle branch block." N Engl J Med 1996; 334 (8): 481-7. PMID 8559200
- ↑ "Electrocardiographic ST-segment elevation: the diagnosis of acute myocardial infarction by morphologic analysis of the ST segment." Acad Emerg Med 2001; 8(10): 961-7. PMID 11581081
- ↑ Wang K, Asinger RW, Marriott HJ. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003 Nov 27; 349 (22): 2128-35. Review. PMID 14645641
- ↑ Ako J, Honda Y, Fitzgerald PJ. Conditions associated with ST-segment elevation. N Engl J Med. 2004 Mar 11; 350 (11): 1152-5; (author reply to PMID 14645641) 1152-5. PMID 15014192
- ↑ Lipovetsky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Heavy meals as a trigger for a first event of the acute coronary syndrome:a case-crossover study. Isr Med Assoc J. 2004;6:728 –731.
- ↑ Lipovetsky N, Hod H, Roth A, Kishon Y, Sclarovsky S, Green MS. Heavy meals as a trigger for a first event of the acute coronary syndrome:a case-crossover study. Isr Med Assoc J. 2004;6:728 –731.
- ↑ Hiroaki Kawano, Yuji Koide, Genji Toda and Katsusuke Yano. ST-segment Elevation of Electrocardiogram in a Patient with Shoshin Beriberi. Internal Medicine. Vol. 44 (2005) , No. 6 pp.578-585.
- ↑ Hundley JM, Ashburn LL, Sebrell WH. The electrocardiogram in chronic thiamine deficiency in rats. Am J Physiol 144: 404–414, 1954.
- ↑ Read DH, Harrington DD. Experimentally induced thiamine deficiency in beagle dogs: clinical observations. Am J Vet Res 42: 984–991, 1981.
- ↑ Selker HP, Zalenski RJ, Antman EM, et al. "An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: executive summary of a National Heart Attack Alert Program Working Group Report." Ann Emerg Med 1997; 29(1): 25-28. PMID 8998085
- ↑ Masoudi FA, Magid DJ, Vinson DR et al."Implications of the Failure to Identify High-Risk Electrocardiogram Findings for the Quality of Care of Patients With Acute Myocardial Infarction." Circulation 2006; 114: 1565-1571.
- ↑ Morris F, Brady W (2002). "ABC of clinical electrocardiography: Acute myocardial infarction-Part I.". BMJ. 324 (7341): 831–4. PMID 1934778.Full text
- ↑ Novotný T, Sisáková M, Floriánová A, Toman O, Dohnalová I, Poloczek M, Kala P, Kyselová I, Dostálová L, Vít P, Spinar J. [QT dynamicity in risk stratification in patients after myocardial infarction]. Vnitr Lek 2007 Sep; 53(9) 964-7. PMID 18019666
- ↑ Jensen BT, Abildstrom SZ, Larroude CE, Agner E, Torp-Pedersen C, Nyvad O, Ottesen M, Wachtell K, and Kanters JK. QT dynamics in risk stratification after myocardial infarction. Heart Rhythm 2005 Apr; 2(4) 357-64. doi:10.1016/j.hrthm. 2004.12.028 PMID 15851335
- ↑ Chevalier P, Burri H, Adeleine P, Kirkorian G, Lopez M, Leizorovicz A, André-Fouët X, Chapon P, Rubel P, Touboul P; QT dynamicity and sudden death after myocardial infarction: results of a long-term follow-up study. J Cardiovasc Electrophysiol 2003 Mar; 14(3) 227-33. PMID 12716101
See Also
Additional Resources
- Tanel RE. ECGs in the ED. Pediatr Emerg Care. 2008 Jan; 24 (1): 62-3. PMID 18212616
External links
- The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research
- Clinical Trial Results: An up to date resource of Cardiovascular Research
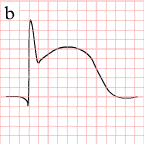

















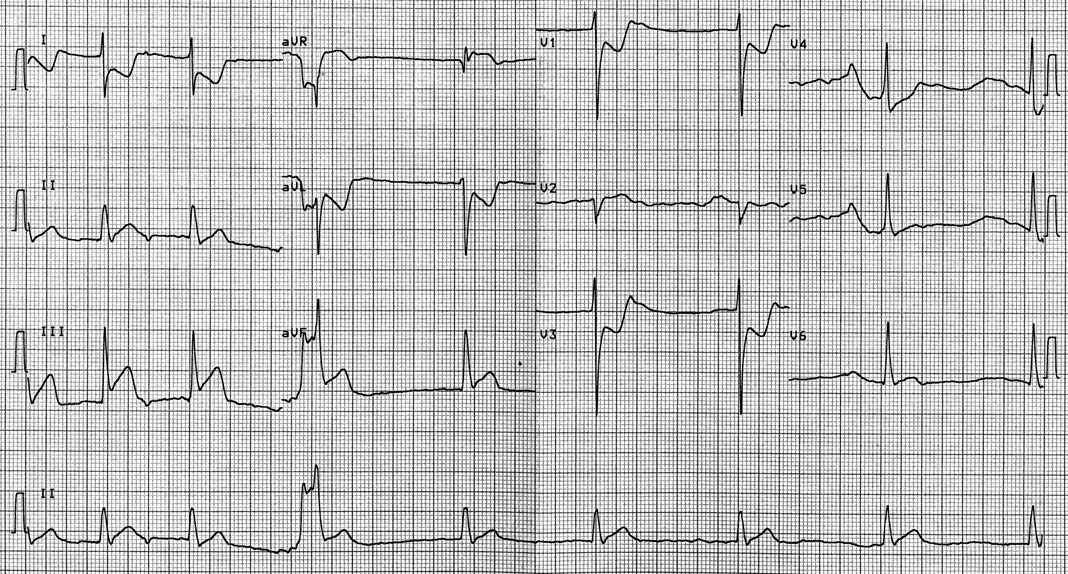






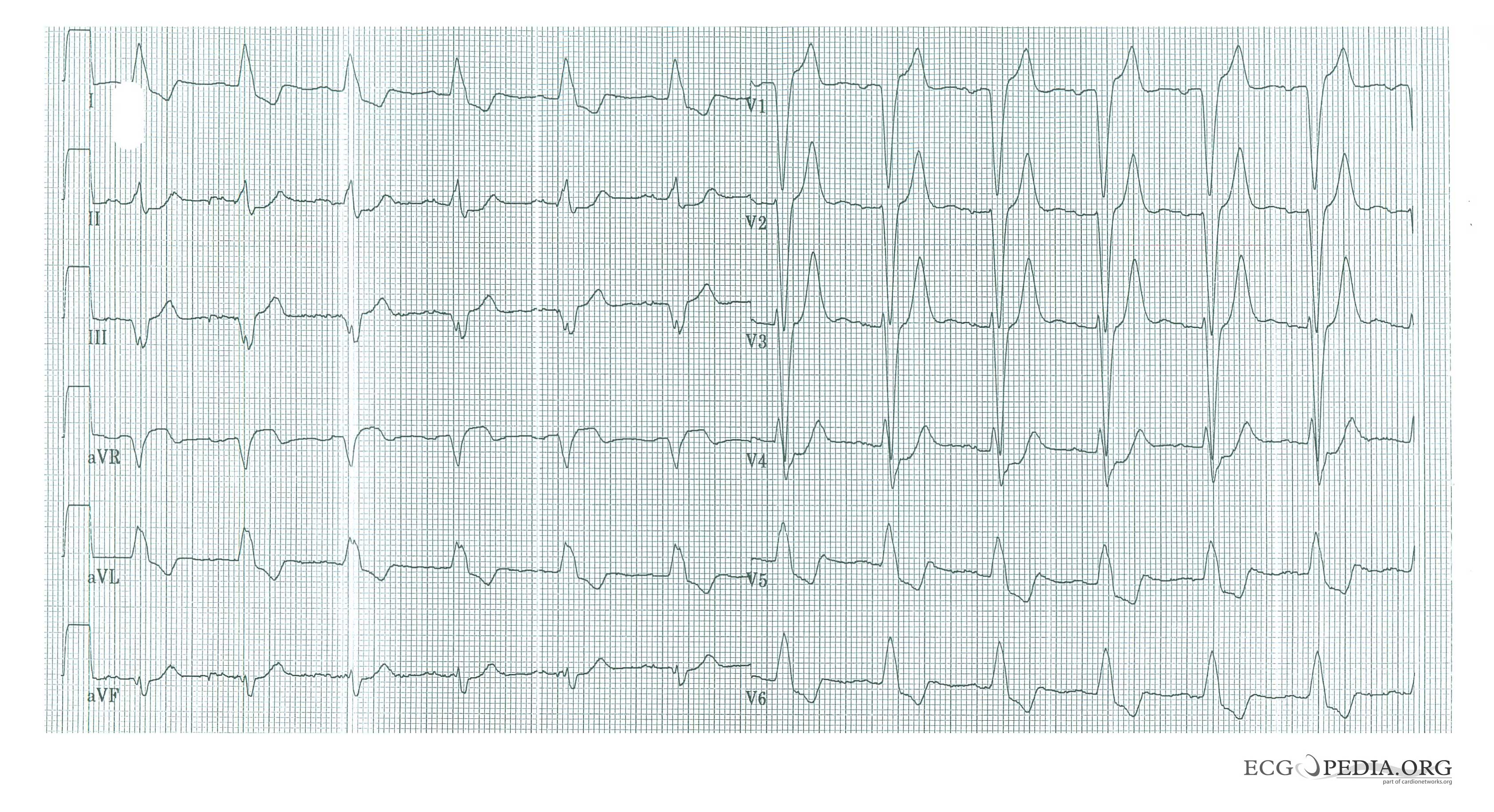

![Typical negative T waves post anterior myocardial infarction. This patient also shows QTc prolongation. Whether this has an effect on prognosis is debated. [21] [22] [23]](/images/1/17/STEMI_28.png)