ST elevation myocardial infarction electrocardiogram: Difference between revisions
No edit summary |
No edit summary |
||
| Line 21: | Line 21: | ||
[[Image:Coronary arteries related myocardial area.png|thumb|none|450px|Coronary arteries related myocardial area]] | [[Image:Coronary arteries related myocardial area.png|thumb|none|450px|Coronary arteries related myocardial area]] | ||
{| | {| style="width:80%; height:100px" border="1" | ||
! Wall Affected | ! Wall Affected | ||
! Leads Showing ST Segment Elevation | ! Leads Showing ST Segment Elevation | ||
| Line 102: | Line 102: | ||
|- | |- | ||
|} | |} | ||
===Measurement of the Magnitude of ST Elevation: 60 Milliseconds after the J point=== | ===Measurement of the Magnitude of ST Elevation: 60 Milliseconds after the J point=== | ||
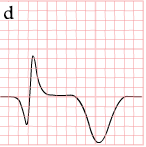
The optimal time after the J point to measure ST elevation is debated. This example shows the technique of measuring the magnitude of ST elevation 60 milliseconds or 1.5 small boxes after the J point. | The optimal time after the J point to measure ST elevation is debated. This example shows the technique of measuring the magnitude of ST elevation 60 milliseconds or 1.5 small boxes after the J point. | ||
| Line 108: | Line 109: | ||
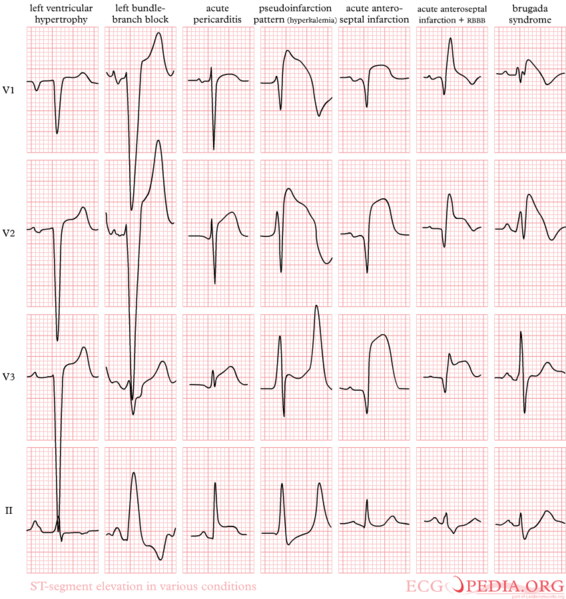
Early repolarization is an electrocardiographic pattern that can mimic the changes of ST elevation myocardial infarction. It is often seen in younger males. As the example below shows, there is often a notch (shown in red) where the QRS and ST segments join. | Early repolarization is an electrocardiographic pattern that can mimic the changes of ST elevation myocardial infarction. It is often seen in younger males. As the example below shows, there is often a notch (shown in red) where the QRS and ST segments join. | ||
[[Image:Normal_ST_elevation.png | [[Image:Normal_ST_elevation.png|none|500px|'''Examples of Early Repolarization and Normal Variant of ST Elevation''']] | ||
==EKG Examples== | ==EKG Examples== | ||
Revision as of 20:34, 30 May 2012
|
ST Elevation Myocardial Infarction Microchapters |
|
Differentiating ST elevation myocardial infarction from other Diseases |
|
Diagnosis |
|
Treatment |
|
|
Case Studies |
|
ST elevation myocardial infarction electrocardiogram On the Web |
|
ST elevation myocardial infarction electrocardiogram in the news |
|
Blogs on ST elevation myocardial infarction electrocardiogram |
|
Directions to Hospitals Treating ST elevation myocardial infarction |
|
Risk calculators and risk factors for ST elevation myocardial infarction electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
A primary purpose of the electrocardiogram is to detect ischemia or acute coronary injury in broad, symptomatic emergency department populations. The 12 lead ECG is used to classify patients into one of three groups:
- Those with ST segment elevation or new bundle branch block (suspicious for acute injury and a possible candidate for acute reperfusion therapy with thrombolytics or primary PCI),
- Those with ST segment depression or T wave inversion (suspicious for ischemia), and
- Those with a so-called non-diagnostic or normal ECG.[1]
A normal ECG does not rule out the presence of acute myocardial infarction. Sometimes the earliest presentation of acute myocardial infarction is instead the presence of a hyperacute T wave.[2] In clinical practice, hyperacute T waves are rarely seen, because they exists for only 2-30 minutes after the onset of infarction.[3] Hyperacute T waves need to be distinguished from the peaked T waves associated with hyperkalemia.[4]
Definition of ST Elevation
The electrocardiographic definition of ST elevation MI requires the following: at least 1 mm (0.1 mV) of ST segment elevation in 2 or more anatomically contiguous leads.[1] While these criteria are sensitive, they are not specific as thromboctic coronary occlusion is not the most common cause of ST segment elevation in chest pain patients.[5]
Limitations of the 12 lead ECG
While clinicians are widely familar with the 12 lead ECG, there are limitations to its sensitivity and specificity in detecting myocardial injury due to thrombotic vessel occlusion. A single static ECG represents a brief sample in time. In STEMI, the culprit artery is often opening and closing or "winking and blinking" due to cyclic flow variations with the clot dissolving and reforming again. Furthermore, patients with acute coronary syndromes often have rapidly changing supply versus demand characteristics. As a clinical example, one of the authors (CM Gibson) once saw a patient with 6 hours of chest pain who had non-specific ECG changes. 15 minutes later the patient complained of worsening chest pain, and at that time the ECG showed ST elevation. Had the second ECG with ST elevation been instead the first ECG that was reviewed, it would have been concluded that the patient was infarcting for over 6 hours, when instead, the artery was occluded for 15 minutes at most during the recent episode of chest pain. Because a single ECG may not accurately represent evolving myocardial injury, it is standard practice to obtain serial 12 lead ECGs, particularly if the first ECG is obtained during a pain-free episode. Alternatively, many emergency departments and chest pain centers use computers capable of continuous ST segment monitoring.[6] While the standard 12 lead ECG is well designed to detect anterior ischemia, by virtue of the fact that it samples only electrical vectors from the front left chest wall, the 12 lead ECG may miss right ventricular and posterior infarctions. In particular, acute myocardial infarction in the distribution of the circumflex artery is likely to produce a nondiagnostic ECG or ST segment depression in the anterior precordial leads. The use of non-standard ECG leads like right-sided lead V4R and posterior leads V7, V8, and V9 may improve sensitivity for right ventricular and posterior myocardial infarction. Newer technologies such as the 80 lead ECG have demonstrated greater sensitivity in detecting RV and posterior infarcts compared with the 12 lead ECG. The failure to identify patients with ST elevation MI delays care and has a negative effect on the quality of patient care.[7]
Localization of the Culprit Artery Based Upon the 12 lead ECG
While the ECG leads that are involved with ST elevation and depression are often used to predict the potential location of the culprit artery, teh sensitivity and specificity of these techniques are often poor. New technologies such as 80 lead ECGs may prove to be more useful in this regard. Identification of the potential culprit artery can be important in guiding patient management. In particular, the ECG should be used to identify patients with a right ventricular infarct where nitrate administration is contraindicated. The 12 lead ECG can also be used to identify the most appropriate artery to perform angiography on first when performing primary angioplasty.

| Wall Affected | Leads Showing ST Segment Elevation | Leads Showing Reciprocal ST Segment Depression | Suspected Culprit Artery |
|---|---|---|---|
| Septal | V1, V2 | None | Left Anterior Descending (LAD) |
| Anterior | V3, V4 | None | Left Anterior Descending (LAD) |
| Anteroseptal | V1, V2, V3, V4 | None | Left Anterior Descending (LAD) |
| Anterolateral | V3, V4, V5, V6, I, aVL | II, III, aVF | Left Anterior Descending (LAD), Circumflex (LCX), or Obtuse Marginal |
| Extensive anterior (Sometimes called Anteroseptal with Lateral extension) | V1,V2,V3, V4, V5, V6, I, aVL | II, III, aVF | Left main coronary artery (LCA) |
| Inferior | II, III, aVF | I, aVL | Right Coronary Artery (RCA) or Circumflex (LCX) |
| Lateral | I, aVL, V5, V6 | II, III, aVF | Circumflex (LCX) or Obtuse Marginal |
| Posterior (Usually associated with Inferior or Lateral but can be isolated) | V7, V8, V9 | V1,V2,V3, V4 | Posterior Descending (PDA) (branch of the RCA or Circumflex (LCX)) |
| Right ventricular (Usually associated with Inferior) | II, III, aVF, V1, V4R | I, aVL | Right Coronary Artery (RCA) |
Evolution of ST Segment Elevation
As the myocardial infarction evolves, there may be loss of R wave height and development of pathological Q waves. T wave inversion may persist for months or even permanently following acute myocardial infarction.[8] Typically, however, the T wave recovers, leaving a pathological Q wave as the only remaining evidence that an acute myocardial infarction has occurred. Understanding the typical time course of ST changes in acute MI is critical in distinguishing STEMI from pericarditis and other conditions.
| Figure | change | |
|---|---|---|
| minutes | 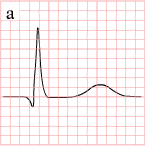
|
hyperacute T waves (peaked T waves)
ST-elevation |
| hours | 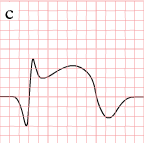
|
ST-elevation, with terminal negative T wave
negative T wave (these can last for months) |
| days | 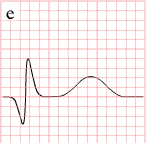
|
Pathologic Q Waves |
Measurement of the Magnitude of ST Elevation: 60 Milliseconds after the J point
The optimal time after the J point to measure ST elevation is debated. This example shows the technique of measuring the magnitude of ST elevation 60 milliseconds or 1.5 small boxes after the J point.
Distinguishing Early Repolarization and Other Normal Variants from Pathologic ST Elevation
Early repolarization is an electrocardiographic pattern that can mimic the changes of ST elevation myocardial infarction. It is often seen in younger males. As the example below shows, there is often a notch (shown in red) where the QRS and ST segments join.

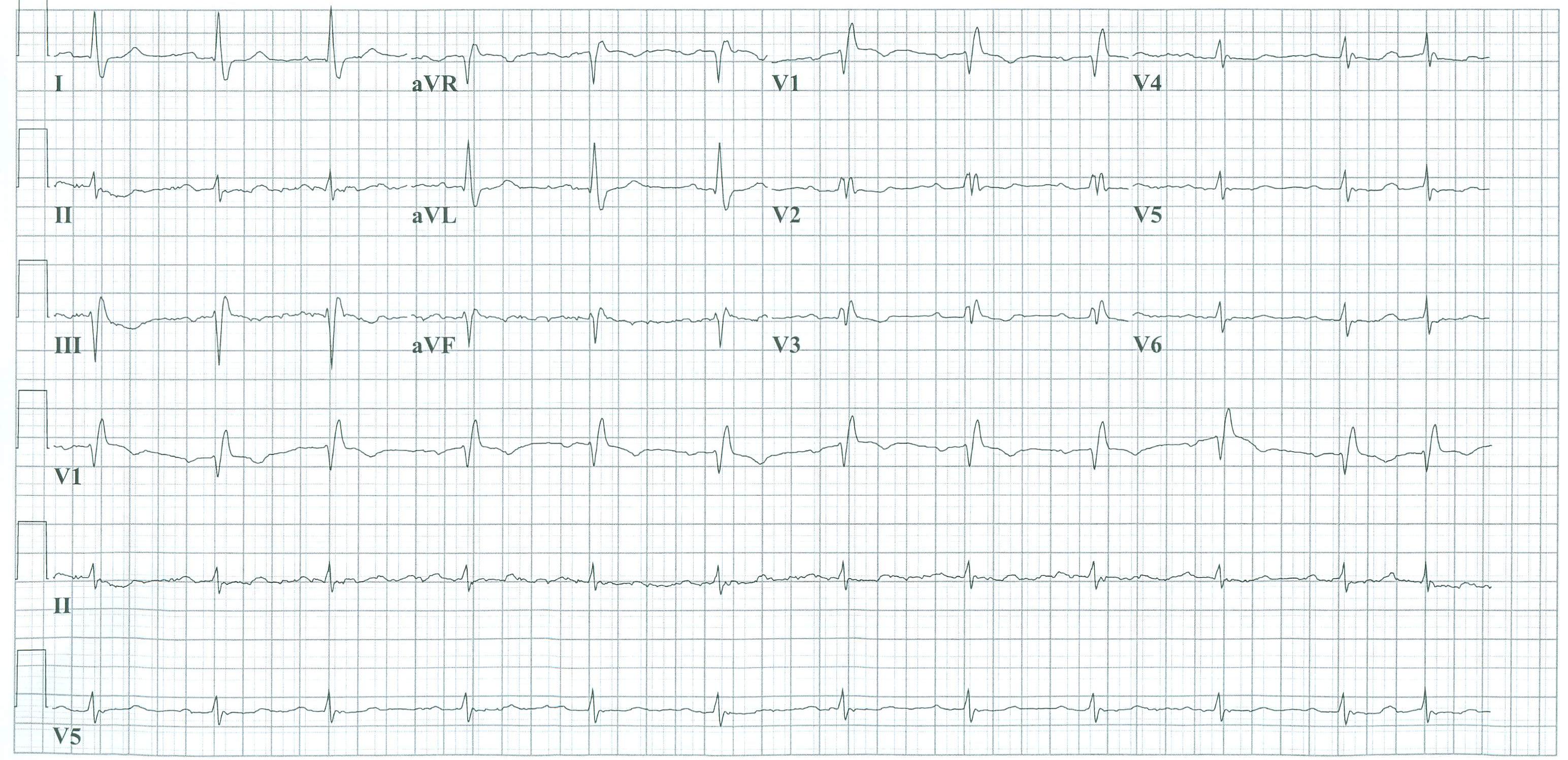
EKG Examples
-
The evolution of an infarct on the ECG. ST elevation, Q wave formation, T wave inversion, normalization with a persistent Q wave
-
Pathologic ST elevation
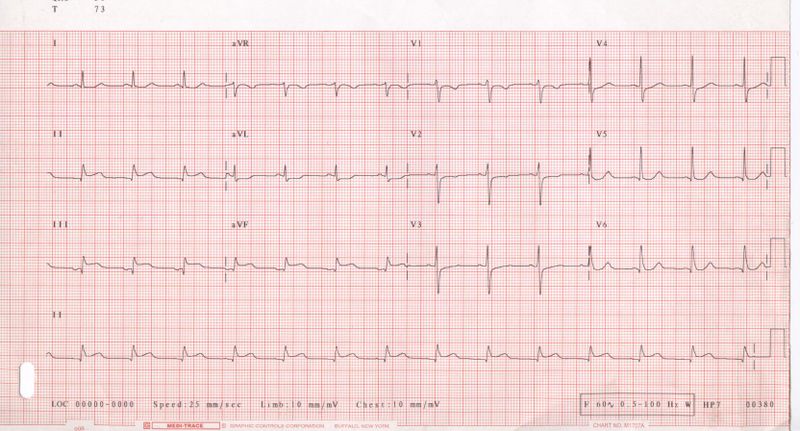
-
12-lead electrocardiogram (ECG) showing acute inferior ST segment elevation MI (STEMI). Note the ST segment elevation in leads II, III, and aVF along with reciprocal ST segment depression in leads I and aVL.
-
Acute inferior myocardial infarction with RV involvement.
-
Acute inferoposterior MI: ST elevation in II, III, AVF (in III > II). ST depression in I, AVL, V2. Tall R in V2, otherwise normal QRS morphology.
-
Acute inferior MI
-
Acute posterolateral MI
-
Acute inferolateral MI: ST depression in V1, V4, tall R in V2. ST elevation in II, III, AVF, V5 and V6.
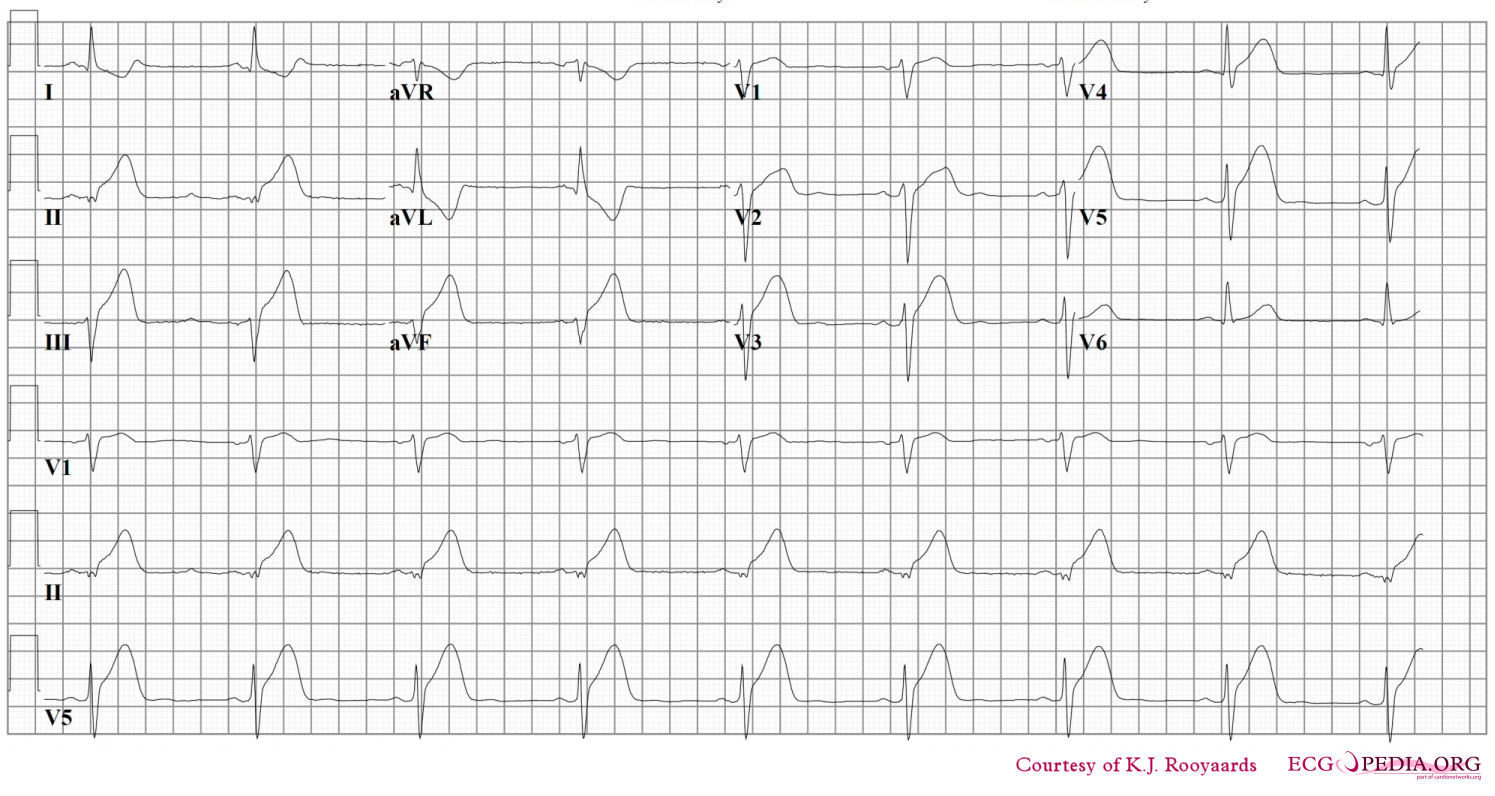
-
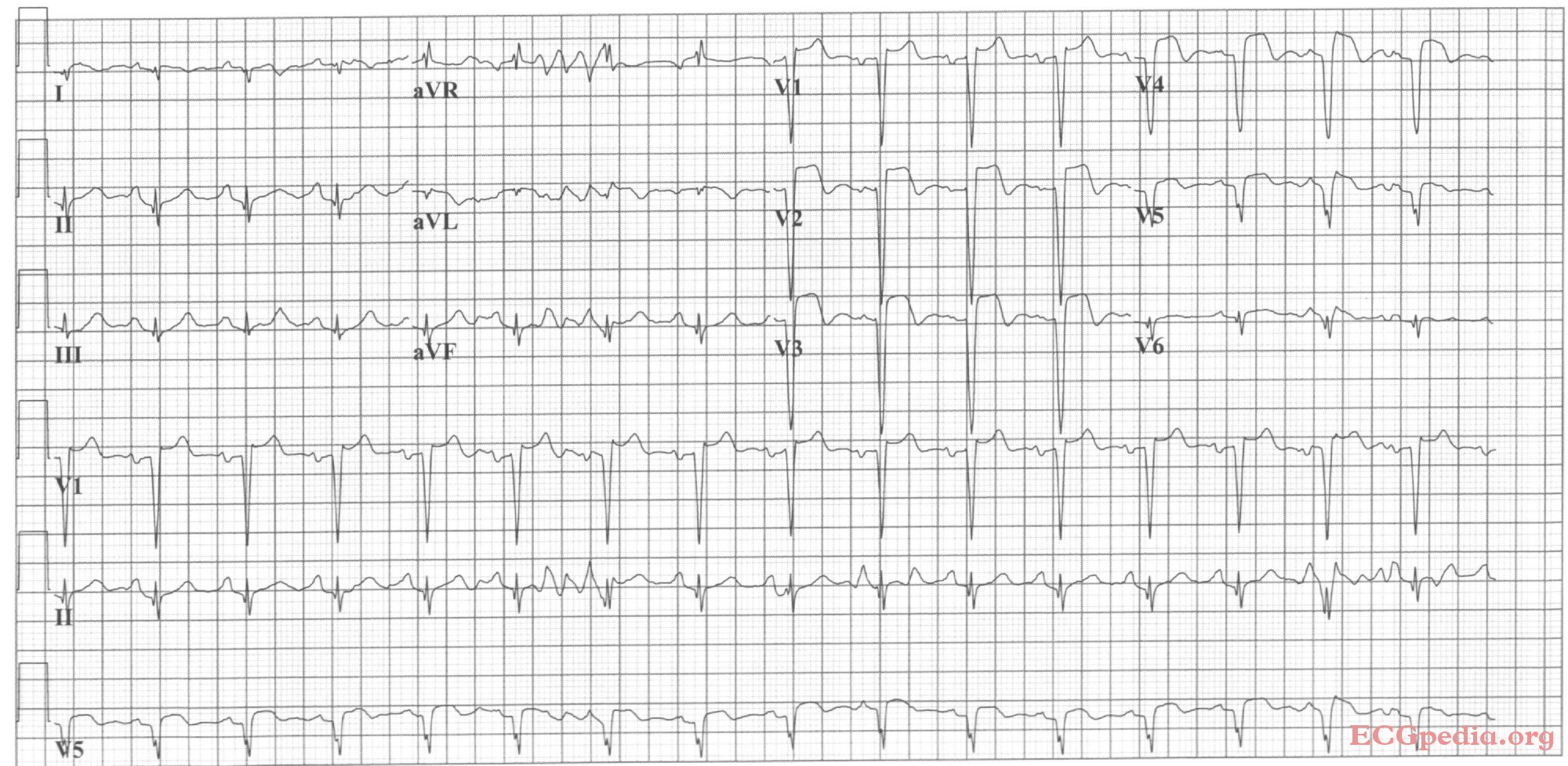
Acute anterior MI. Loss of R waves throughout the anterior wall (V1-V6). QS complexes in V3-V5. ST elevation in V1-V5 with terminal negative T waves.
-
Sinus bradycardia with first degree AV block and inferior-posterior-lateral myocardial infarction.
-
Sinus bradycardia with inferior-lateral myocardial infarction.
-
Acute anterior MI. LAD artery occlusion
-
Sinus rhythm with anteroseptal myocardial infarction.
-
Sinus rhythm with left bundle branch block, comparison with an old EKG is mandatory to evaluate whether the LBBB is new (a sign of myocardial infarction) or old.
-
Inferior-posterior myocardial infarction with complete AV block and ventricular excape rhythm with RBBB pattern and left axis, followed by sinus rhythm.
-
Acute anterior myocardial infarction and left anterior hemiblock. Image courtesy of Dr Jose Ganseman
-
Old anterior myocardial infarction and bifascicular block (RBBB and LAHB) Image courtesy of Dr Jose Ganseman
-
Acute MI with proximal LAD occlusion
-
A 2 days old anterior infarction with Q waves in V1-V4 with persisting ST elevation, a sign of left ventricular aneurysm formation.
-
A 2 weeks old anterior infarction with Q waves in V2-V4 and persisting ST elevation, a sign of left ventricular aneurysm formation.
-
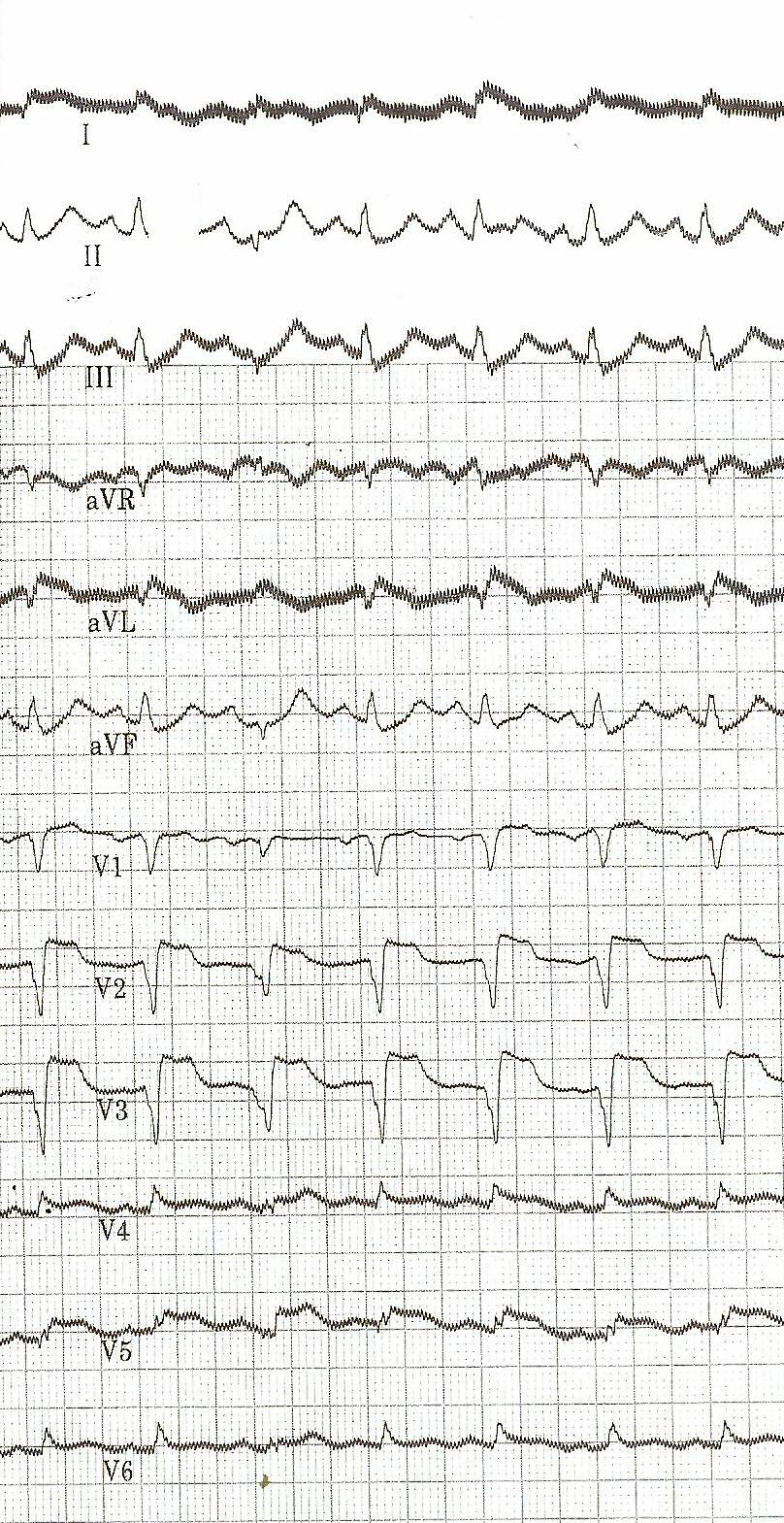
The heart rate increases and there are two extra systoles short after each other. Then, a chaotic rhythm develops: ventricular fibrillation.
-
Atrial fibrillation and inferior-posterior myocardial infarction.
-
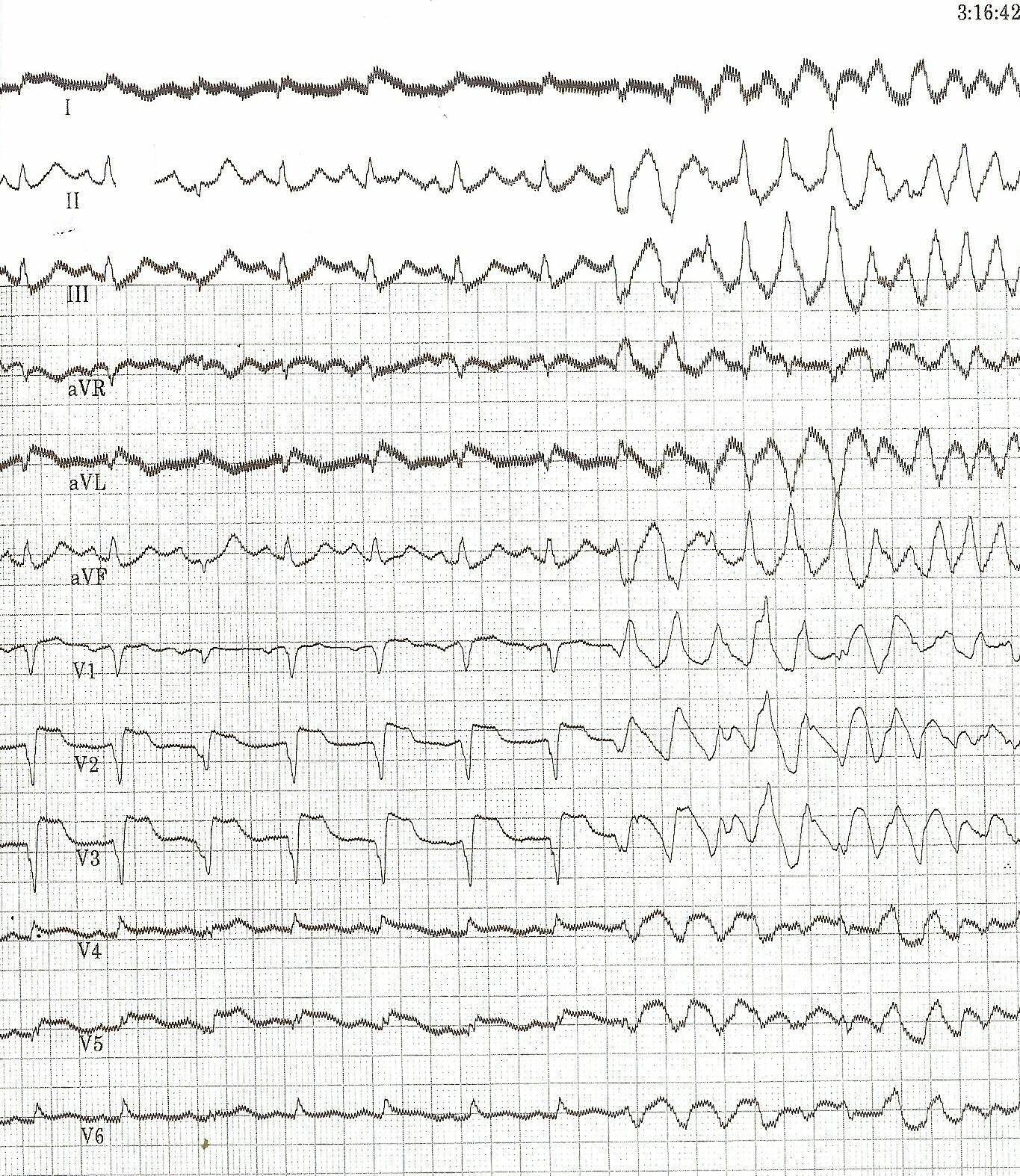
Same patient's 2. EKG; This EKG shows clear ST elevation in the right precordial leads. A coronary angiography revealed a proximal right coronary artery occlusion.
-
Inferior-posterior-lateral myocardial infarction with a nodal escape rhythm
-
The same patient before acute MI developed. Horizontal axis.
-
Acute myocardial infarction in in a patient with a pacemaker and LBBB. Concordant ST elevation in V5-V6 are clearly visible. There is discordant ST segment elevation > 5 mm in lead V3.
-
Atrial fibrillation with inferior-posterior-lateral myocardial infarction and incomplete right bundle branch block. Lead I shows ST depression, suggestive of right coronary artery involvement.
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [12]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [13]
References
- ↑ 1.0 1.1 "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 8: Stabilization of the Patient With Acute Coronary Syndromes." Circulation 2005; 112: IV-89 - IV-110.
- ↑ Somers MP, Brady WJ, Perron AD, Mattu A (2002). "The prominant T wave: electrocardiographic differential diagnosis". Am J Emerg Med. 20 (3): 243–51. PMID 11992348. Unknown parameter
|month=ignored (help) - ↑ Smith SW, Whitwam W. "Acute Coronary Syndromes." Emerg Med Clin N Am 2006; 24(1): 53-89. PMID 16308113
- ↑ "The clinical value of the ECG in noncardiac conditions." Chest 2004; 125(4): 1561-76. PMID 15078775
- ↑ Smith SW, Whitwam W (2006). "Acute coronary syndromes". Emerg. Med. Clin. North Am. 24 (1): 53–89, vi. doi:10.1016/j.emc.2005.08.008. PMID 16308113. Unknown parameter
|month=ignored (help) - ↑ Selker HP, Zalenski RJ, Antman EM; et al. (1997). "An evaluation of technologies for identifying acute cardiac ischemia in the emergency department: executive summary of a National Heart Attack Alert Program Working Group Report". Ann Emerg Med. 29 (1): 1–12. PMID 8998085. Unknown parameter
|month=ignored (help) - ↑ Masoudi FA, Magid DJ, Vinson DR; et al. (2006). "Implications of the failure to identify high-risk electrocardiogram findings for the quality of care of patients with acute myocardial infarction: results of the Emergency Department Quality in Myocardial Infarction (EDQMI) study". Circulation. 114 (15): 1565–71. doi:10.1161/CIRCULATIONAHA.106.623652. PMID 17015790. Unknown parameter
|month=ignored (help) - ↑ Namba Y, Bando M, Takeda K, Iwata M, Mannen T (1991). "[Marchiafava-Bignami disease with symptoms of the motor impersistence and unilateral hemispatial neglect]". Rinsho Shinkeigaku (in Japanese). 31 (6): 632–5. PMID 1934778. Unknown parameter
|month=ignored (help) - ↑ Novotný T, Sisáková M, Floriánová A; et al. (2007). "[QT dynamicity in risk stratification in patients after myocardial infarction]". Vnitr Lek (in Czech). 53 (9): 964–7. PMID 18019666. Unknown parameter
|month=ignored (help) - ↑ Jensen BT, Abildstrom SZ, Larroude CE; et al. (2005). "QT dynamics in risk stratification after myocardial infarction". Heart Rhythm. 2 (4): 357–64. doi:10.1016/j.hrthm.2004.12.028. PMID 15851335. Unknown parameter
|month=ignored (help) - ↑ Chevalier P, Burri H, Adeleine P; et al. (2003). "QT dynamicity and sudden death after myocardial infarction: results of a long-term follow-up study". J. Cardiovasc. Electrophysiol. 14 (3): 227–33. PMID 12716101. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)
Related Chapters
- Pages with citations using unsupported parameters
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- CS1 maint: Unrecognized language
- Cardiology
- Ischemic diseases
- Electrophysiology
- Emergency medicine
- Laboratory studies
- Mature chapter
- Microchapter candidate
- Up-To-Date
- Up-To-Date cardiology
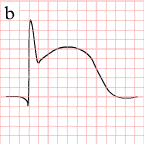

















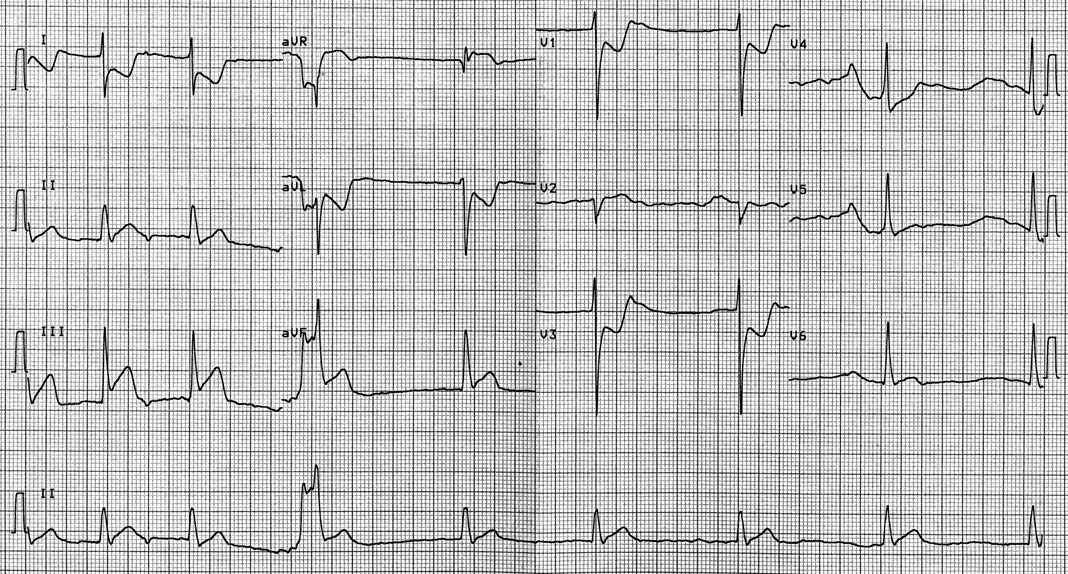






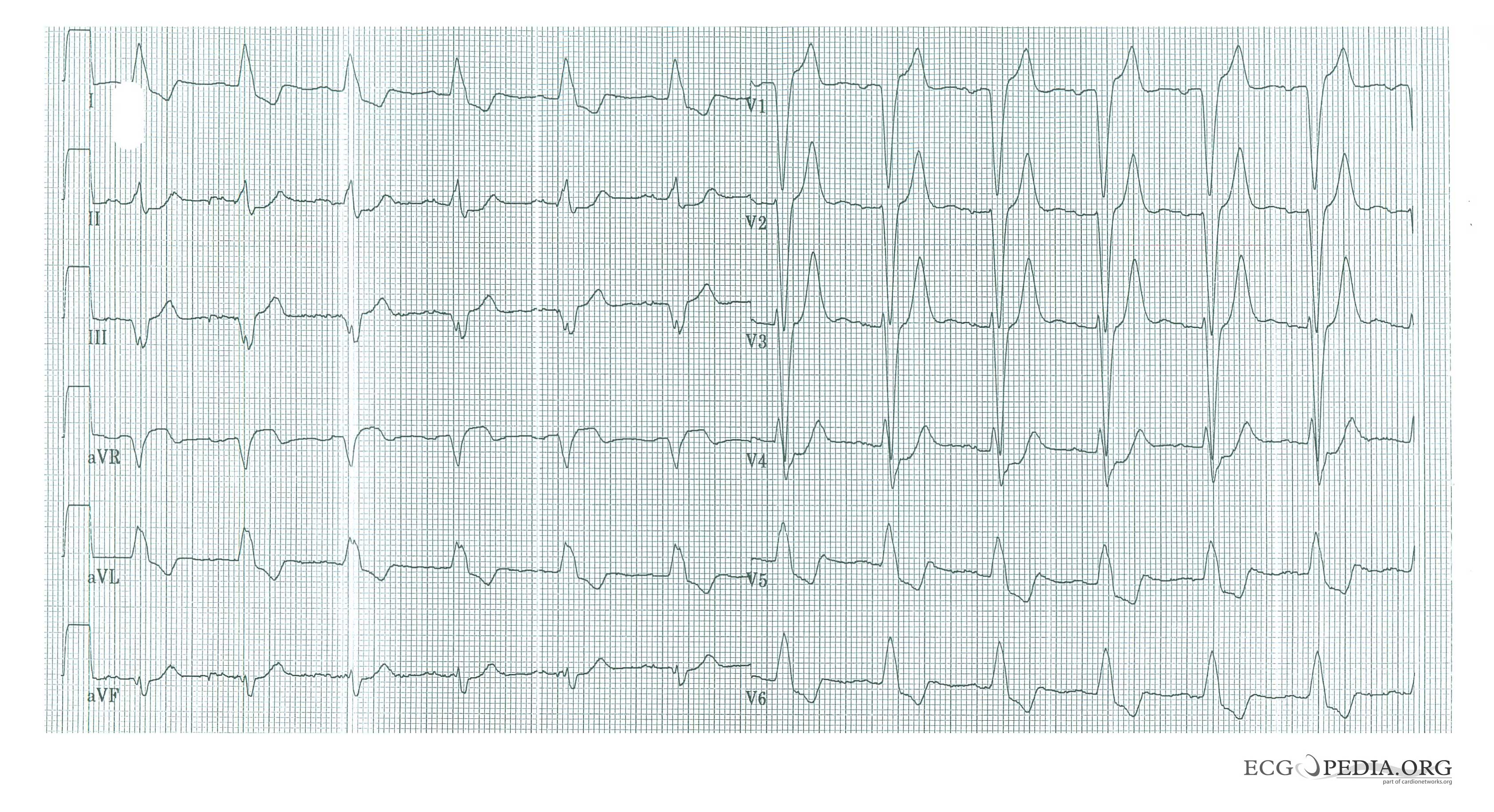

![Typical negative T waves post anterior myocardial infarction. This patient also shows QTc prolongation. Whether this has an effect on prognosis is debated. [9][10][11]](/images/1/17/STEMI_28.png)