ST elevation myocardial infarction coronary artery bypass grafting: Difference between revisions
No edit summary |
|||
| Line 14: | Line 14: | ||
MeshID = | | MeshID = | | ||
}} | }} | ||
'''For patient information click [[Heart attack (patient information)|here]]''' | |||
{{CMG}} | {{CMG}} | ||
Revision as of 13:48, 1 July 2010
| Myocardial infarction | |
 | |
|---|---|
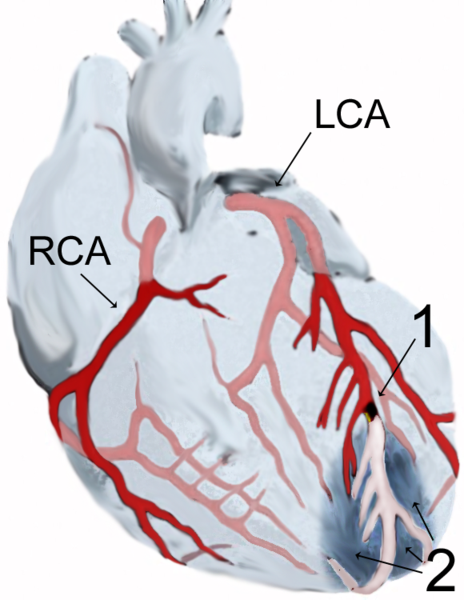
| Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
| Cardiology Network |
 Discuss ST elevation myocardial infarction coronary artery bypass grafting further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Coronary Artery Bypass Surgery

Despite the guidelines, emergency bypass surgery for the treatment of an acute myocardial infarction (MI) is less common then PCI or medical management. In an analysis of patients in the U.S. National Registry of Myocardial Infarction (NRMI) from January 1995 to May 2004, the percentage of patients with cardiogenic shock treated with primary PCI rose from 27.4% to 54.4%, while the increase in CABG treatment was only from 2.1% to 3.2%.[1]
Emergency coronary artery bypass graft surgery (CABG) is usually undertaken to simultaneously treat a mechanical complication, such as a ruptured papillary muscle, or a ventricular septal defect, with ensueing cardiogenic shock.[2] In uncomplicated MI, the mortality rate can be high when the surgery is performed immediately following the infarction.[3] If this option is entertained, the patient should be stabilized prior to surgery, with supportive interventions such as the use of an intra-aortic balloon pump.[4] In patients developing cardiogenic shock after a myocardial infarction, both PCI and CABG are satisfactory treatment options, with similar survival rates.[5][6]
Coronary artery bypass surgery involves an artery or vein from the patient being implanted to bypass narrowings or occlusions on the coronary arteries. Several arteries and veins can be used, however internal mammary artery grafts have demonstrated significantly better long-term patency rates than great saphenous vein grafts.[7] In patients with two or more coronary arteries affected, bypass surgery is associated with higher long-term survival rates compared to percutaneous interventions.[8] In patients with single vessel disease, surgery is comparably safe and effective, and may be a treatment option in selected cases.[9] Bypass surgery has higher costs initially, but becomes cost-effective in the long term.[10] A surgical bypass graft is more invasive initially but bears less risk of recurrent procedures (but these may be again minimally invasive).
ACC / AHA Guidelines (DO NOT EDIT)[11]
| “ |
Class I1. Emergency or urgent CABG in patients with STEMI should be undertaken in the following circumstances:
Class IIa1. Emergency CABG can be useful as the primary reperfusion strategy in patients who have suitable anatomy and who are not candidates for fibrinolysis or PCI and who are in the early hours (6 to 12 hours) of an evolving STEMI, especially if severe multivessel or left main disease is present. (Level of Evidence: B) 2. Emergency CABG can be effective in selected patients 75 years or older with ST elevation, LBBB, or posterior MI who develop shock within 36 hours of STEMI, have severe triple-vessel or left main disease, and are suitable for revascularization that can be performed within 18 hours of shock. Patients with good prior functional status who are suitable for revascularization and agree to invasive care may be selected for such an invasive strategy. (Level of Evidence: B) Class III1. Emergency CABG should not be performed in patients with persistent angina and a small area of risk who are hemodynamically stable. (Level of Evidence: C) 2. Emergency CABG should not be performed in patients with successful epicardial reperfusion but unsuccessful microvascular reperfusion. (Level of Evidence: C) |
” |
See also
- acute coronary syndrome
- angina
- Cardiac arrest
- coronary thrombosis
- Hibernating myocardium
- Stunned myocardium
- Ventricular remodeling
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [12]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [11]
References
- ↑ Babaev A, Frederick PD, Pasta DJ, Every N, Sichrovsky T, Hochman JS (2005). "Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock". JAMA. 294 (4): 448–54. doi:10.1001/jama.294.4.448. PMID 16046651. Unknown parameter
|month=ignored (help) - ↑ Townsend, Courtney M. (2004). Sabiston Textbook of Surgery - The Biological Basis of Modern Surgical Practice. Philadelphia, Pennsylvania: Elsevier Saunders. p. 1871. ISBN 0-7216-0409-9. Unknown parameter
|coauthors=ignored (help) - ↑ Kaul TK, Fields BL, Riggins SL, Dacumos GC, Wyatt DA, Jones CR (1995). "Coronary artery bypass grafting within 30 days of an acute myocardial infarction". Ann. Thorac. Surg. 59 (5): 1169–76. PMID 7733715. Unknown parameter
|month=ignored (help) - ↑ Creswell LL, Moulton MJ, Cox JL, Rosenbloom M (1995). "Revascularization after acute myocardial infarction". Ann. Thorac. Surg. 60 (1): 19–26. PMID 7598589. Unknown parameter
|month=ignored (help) - ↑ White HD, Assmann SF, Sanborn TA; et al. (2005). "Comparison of percutaneous coronary intervention and coronary artery bypass grafting after acute myocardial infarction complicated by cardiogenic shock: results from the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial". Circulation. 112 (13): 1992–2001. doi:10.1161/CIRCULATIONAHA.105.540948. PMID 16186436. Unknown parameter
|month=ignored (help) - ↑ Hochman JS, Sleeper LA, Webb JG; et al. (2006). "Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction". JAMA. 295 (21): 2511–5. doi:10.1001/jama.295.21.2511. PMC 1782030. PMID 16757723. Unknown parameter
|month=ignored (help) - ↑ Raja SG, Haider Z, Ahmad M, Zaman H (2004). "Saphenous vein grafts: to use or not to use?". Heart Lung Circ. 13 (4): 403–9. doi:10.1016/j.hlc.2004.04.004. PMID 16352226. Unknown parameter
|month=ignored (help) - ↑ Hannan EL, Racz MJ, Walford G; et al. (2005). "Long-term outcomes of coronary-artery bypass grafting versus stent implantation". N. Engl. J. Med. 352 (21): 2174–83. doi:10.1056/NEJMoa040316. PMID 15917382. Unknown parameter
|month=ignored (help) - ↑ Bourassa MG (2000). "Clinical trials of coronary revascularization: coronary angioplasty vs. coronary bypass grafting". Curr. Opin. Cardiol. 15 (4): 281–6. PMID 11139092. Unknown parameter
|month=ignored (help) - ↑ Hlatky MA, Boothroyd DB, Melsop KA; et al. (2004). "Medical costs and quality of life 10 to 12 years after randomization to angioplasty or bypass surgery for multivessel coronary artery disease". Circulation. 110 (14): 1960–6. doi:10.1161/01.CIR.0000143379.26342.5C. PMID 15451795. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1 Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help)
External links
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American College of Cardiology (ACC) Door to Balloon (D2B) Initiative.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.