Renal tubular acidosis: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 18:32, 8 May 2012
| Renal tubular acidosis | |
 | |
|---|---|
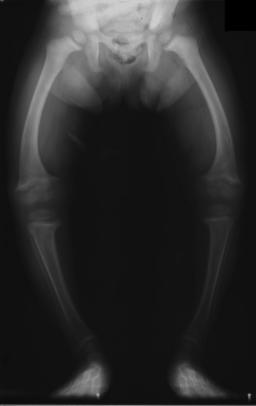
| Significant bilateral nephrocalcinosis (calcification of the kidneys) on a frontal X-ray (radiopacities (white) in the right upper and left upper quadrant of the image), as seen in distal renal tubular acidosis. | |
| ICD-10 | N25.8 |
| ICD-9 | 588.89 |
| OMIM | 179800 |
| DiseasesDB | 11687 Template:DiseasesDB2 Template:DiseasesDB2 |
| MeSH | D000141 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Renal tubular acidosis (RTA) is a medical condition that involves an accumulation of acid in the body due to a failure of the kidneys to appropriately acidify the urine.[1] When blood is filtered by the kidney, the filtrate passes through the tubules of the nephron, allowing for exchange of salts, acid equivalents, and other solutes before it drains into the bladder as urine. The metabolic acidosis that results from RTA may be caused either by failure to recover sufficient (alkaline) bicarbonate ions from the filtrate in the early portion of the nephron (proximal tubule) or by insufficient secretion of (acid) hydrogen ions into the latter portions of the nephron (distal tubule). Although a metabolic acidosis also occurs in those with renal insufficiency, the term RTA is reserved for individuals with poor urinary acidification in otherwise well-functioning kidneys. Several different types of RTA exist, which all have different syndromes and different causes.
The word acidosis refers to the tendency for RTA to lower the blood's pH. When the blood pH is below normal (7.35), this is called acidemia. The metabolic acidosis caused by RTA is a normal anion gap acidosis.
Type I-Distal RTA
Distal RTA (dRTA) is the most common and also the classical form of RTA, being the first described. It has a number of causes which cause a common underlying problem, which is a failure of acid secretion by the alpha intercalated cells of the cortical collecting duct of the distal nephron. This leads to a failure acidify the urine to a pH of less than 5.3 even if the blood is too acidic (ie there is systemic acidemia), and consequently there is a tendency towards acidemia. This leads to the clinical features of dRTA;[1]
- Variable metabolic acidosis/acidemia
- Hypokalemia (which may be severe)
- Urinary stone formation
- Nephrocalcinosis (deposition of calcium in the substance of the kidney)
- Bone demineralisation (causing rickets in children and osteomalacia in adults)
The acidosis is variable, and one may have dRTA with alpha intercalated cell failure without necessarily being acidemic, this is termed incomplete dRTA. The diagnosis of dRTA can be made by the observation of a urinary pH of greater than 5.3 in the face of a systemic acidemia (usually taken to be a serum bicarbonate of 20 mmol/l or less). In the case of an incomplete dRTA, failure to acidify the urine following an oral acid loading challenge is often used as a test. The test usually performed is the short ammonium chloride test,[2] in which ammonium chloride capsules are used as the acid load. More recently, an alternative test using furosemide and fludrocortisone has been described. [3]
The symptoms and sequelae of dRTA are variable and ranging from being completely asymptomatic, through loin pain and hematuria from kidney stones to failure to thrive and severe rickets in childhood forms as well as possible renal failure and even death.
Interestingly, dRTA has been proposed as a possible diagnosis for the unknown malady plaguing Tiny Tim in Charles Dickens' A Christmas Carol.[4][5]
Causes
- Autoimmune disease. Classically Sjögren's syndrome, but it is also associated with systemic lupus erythematosus, rheumatoid arthritis and even hypergammaglobulinemia. Hypokalaemia is often severe in these cases.[6]
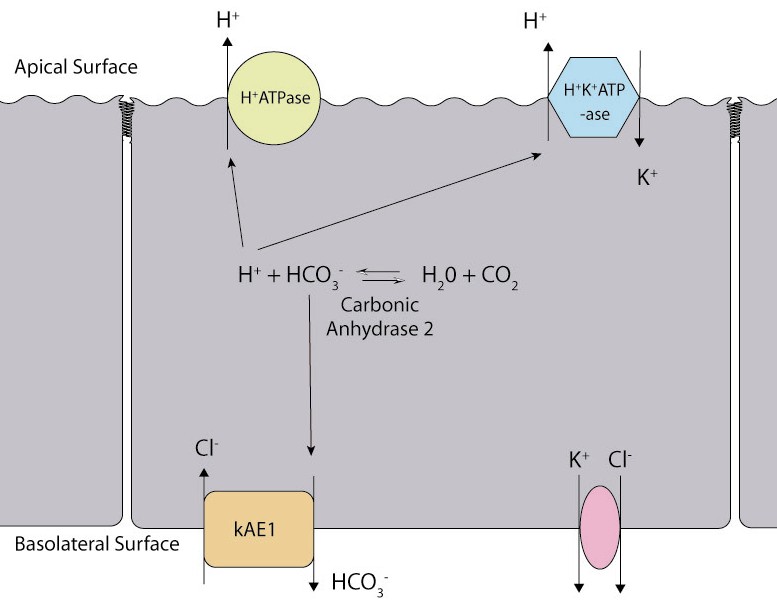
- Hereditary causes include mutations of Band 3[7] the basolateral bicarbonate transporter of the intercalated cell, which may transmit in an autosomal dominant fashion in western European cases, or in an autosomal recessive fashion in South East Asian cases. The South East Asian cases are associated with more severe hypokaemia.[8] Other Hereditary causes include mutations of subunits of the apical proton pump vH+-ATPase,[9] which transmit in an autosomal recessive fashion, and may be associated with sensorineural deafness.[10]
- Liver cirrhosis.
- Nephrocalcinosis. While it is a consequence of dRTA, it can also be a cause; related to calcium-induced damage of the cortical collecting duct.
- Renal transplantation.
- Sickle cell anemia.
- Toxins, including ifosfamide,[11] toluene,[12] lithium carbonate[13] and amphotericin B.[14]
- Chronic urinary tract obstruction.
Treatment
This is relatively straightforward. It involves correction of the acidemia with oral sodium bicarbonate or sodium citrate. This will correct the acidemia and reverse bone demineralisation. Hypokalemia and urinary stone formation and nephrocalcinosis can be treated with potassium citrate tablets which not only replace potassium but won't increase calcium excretion and thus exacerbate stone disease as sodium bicarbonate or citrate may do.[15]
Type 2-Proximal RTA
Proximal RTA (pRTA) is caused by a failure of the proximal tubular cells to reabsorb filtered bicarbonate from the urine, leading to urinary bicarbonate wasting and subsequent acidemia. The distal intercalated cells function normally, so the acidemia is less severe than dRTA and the urine can acidify to a pH of less than 5.3.[16] pRTA also has several causes, and may occasionally be present as a solitary defect, but is usually associated with a more generalised dysfunction of the proximal tubular cells called Fanconi's syndrome where there is also phosphaturia, glycosuria, aminoaciduria, uricosuria and tubular proteinuria. The principle feature of Fanconi's syndrome is bone demineralisation due to phosphate wasting.
Causes
Familial disorders
- Cystinosis[17]
- Galactosemia[18]
- Glycogen storage disease (type I)[19]
- Hereditary fructose intolerance[20]
- Lowe's syndrome[21]
- Tyrosinemia
- Wilson's disease[22]
Acquired disorders
- Amyloidosis[23]
- Multiple myeloma[24]
- Paroxysmal nocturnal hemoglobinuria[25]
- Toxins, such as HAART, ifosfamide,[26] lead, and cadmium
Treatment
Again this depends on oral bicarbonate supplementation. However, this will increase urinary bicarbonate wasting and may well promote a bicarbonate diuresis. The amount of bicarbonate given may have to be very large, to stay ahead of the urinary losses. Correction with oral bicarbonate may exacerbate urinary potassium losses and precipitate hypokalemia.[27]As with dRTA, reversal of the chronic acidosis should reverse bone demineralisation.[28]
Type 3 RTA
This was previously used to designate a rare and transient mixed dRTA and pRTA of uncertain aetiology. Now it is used to describe a genetic defect in type 2 carbonic anhydrase (CA2), which is found in both the proximal and distal tubular cells, as well in bone. As a result it causes;
- proximal renal tubular acidosis
- distal renal tubular acidosis
- osteopetrosis
- cerebral calcification and subsequent mental impairment;
It is very rare and cases from all over the world have been reported, of which about 70% are from the Magreb region of North Africa, possibly due to the high prevalence of consanguinity there.[29] The kidney problems are treated as described above. There is no treatment for the osteopetrosis or cerebral calcification.
Type 4 RTA (Hypoaldosteronism)
Type 4 RTA is not actually a tubular disorder at all, and nor does it have a clinical syndrome similar to the other types of RTA described above. It was included in the classification of renal tubular acidoses as it is associated with a mild (normal anion gap) metabolic acidosis due to a physiological reduction in distal tubular ammonium excretion, which is secondary to hypoaldosteronism. Its cardinal feature is hyperkalemia, and measured urinary acidification is normal.

Causes
- Aldosterone deficiency-Primary (rare)
- Primary adrenal insufficiency
- Congenital adrenal hyperplasia
- Aldosterone synthase deficiency
- Potassium sparing diuretics
- Hyporeninemic hypoaldosteronism (due to decreased angiotensin 2 production as well as intra-adrenal dysfunction)[30]
- Renal dysfunction-most commonly diabetic nephropathy
- HIV infection
- ACE inhibitors
- NSAIDs
- Ciclosporin
- Aldosterone resistance
Treatment
- Aldosterone deficiency should be treated with a mineralocorticoid (such as fludrocortisone), as well as possibly a glucocorticoid for cortisol deficiency, if present.
- Hyporeninemic hypoaldosteronism is ammenable to fludrocortisone treatment,[30] but the accompanying hypertension and edema can prove a problem in these patients, so often a diuretic (such as the thiazide diuretic, bendrofluazide,or a loop diuretic, such as furosemide) is used to control the hyperkalemia.[31]
Related Chapetsr
References
- ↑ 1.0 1.1 Laing, C M (2005). "Renal tubular acidosis: developments in our understanding of the molecular basis". Int J Biochem Cell Biol. 37 (6): 1151–61. Unknown parameter
|month=ignored (help) - ↑ Wrong, O (1959). "The Excretion of Acid in Renal Disease". QJM. 28: 259–313. Unknown parameter
|coauthors=ignored (help) - ↑ Walsh, S B (2007). "Urinary acidification assessed by simultaneous furosemide and fludrocortisone treatment: an alternative to ammonium chloride". Kidney International. Unknown parameter
|month=ignored (help) - ↑ Lewis D (1992). "What was wrong with Tiny Tim?". Am J Dis Child. 146 (12): 1403–7. PMID 1340779.
- ↑ http://www.time.com/time/magazine/article/0,9171,977391,00.html
- ↑ Wrong, OM (1993). "Immune-related potassium-losing interstitial nephritis: a comparison with distal renal tubular acidosis". QJM. 86 (8): 513–542.
- ↑ Bruce, L J (1997). "Familial distal renal tubular acidosis is associated with mutations in the red cell anion exchanger (Band 3, AE1) gene". J Clin Invest. 100: 1693–1707.
- ↑ Bruce, L J (2000). "Band 3 mutations, renal tubular acidosis and South-East Asian ovalocytosis in Malaysia and Papua New Guinea: loss of up to 95% band 3 transport in red cells". Biochem J. 350: 41–51.
- ↑ Wagner, CA (2004). "Renal Vacuolar H+-ATPase". Physiological Reviews. 84 (4): 1263–314. Unknown parameter
|month=ignored (help) - ↑ Karet, F E (1999). "Mutations in the gene encoding B1 subunit of H+-ATPase cause renal tubular acidosis with sensorineural deafness". Nature Genetics. 21: 81–90.
- ↑ Skinner, R (1996). "Risk factors for ifosfamide nephrotoxicity in children". Lancet. 348(9027): 578–80. Unknown parameter
|month=ignored (help) - ↑ Battle, DC (1988). "On the mechanism of toluene-induced renal tubular acidosis". Nephron. 49 (3): 210–8.
- ↑ Boton, R (1987). "Prevalence, pathogenesis, and treatment of renal dysfunction associated with chronic lithium therapy". Am J Kidney Dis. 10 (5): 329–45. Unknown parameter
|month=ignored (help) - ↑ McCurdy, DK (1968). "Renal tubular acidosis due to amphotericin B". NEJM. 278 (3): 124–30. Unknown parameter
|month=ignored (help) - ↑ Morris, R C (2002). "Alkali Therapy In Renal Tubular Acidosis: Who Needs It?" (PDF). J Am Soc Nephrol. 13: 2186–2188.
- ↑ Rodriguez, Soriano J (1967). "Proximal renal tubular acidosis. A defect in bicarbonate reabsorption with normal urinary acidification". Paedatr Res. 1 (2): 81–98. Unknown parameter
|month=ignored (help) - ↑ Gahl, William (2002). "Cystinosis". NEJM. 347: 111–121. Unknown parameter
|month=ignored (help) - ↑ Golberg, L (1956). "A clinical and biochemical study of galactosaemia; a possible explanation of the nature of the biochemical lesion". Arch Dis Child. 31 (158): 254–64. Unknown parameter
|month=ignored (help) - ↑ Matsuo, N (1986). "Proximal renal tubular acidosis in a child with type 1 glycogen storage disease". Acta Paediatr Scand. 75 (2): 332–5. Unknown parameter
|month=ignored (help) - ↑ Morris, Curtis (1968). "An experimental renal acidification defect in patients with hereditary fructose intolerance". J Clin Invest. 47 (6): 1389–1398. Unknown parameter
|month=ignored (help) - ↑ Hodgson, SV (1986). "A balanced de novo X/autosome translocation in a girl with manifestations of Lowe syndrome". Am J Med Genet. 23 (3): 837–47. Unknown parameter
|month=ignored (help) - ↑ Weibers, DO (1979). "Renal stones in Wilson's disease". Am J Med. 67 (2): 249–54. Unknown parameter
|month=ignored (help) - ↑ Rochman, J (1980). "Adult Fanconi's syndrome with renal tubular acidosis in association with renal amyloidosis: occurrence in a patient with chronic lymphocytic leukemia". Arch Int Med. 140 (10). Unknown parameter
|month=ignored (help) - ↑ Messiaen, Thierry (2000). "Adult Fanconi Syndrome Secondary to Light Chain Gammopathy: Clinicopathologic Heterogeneity and Unusual Features in 11 Patients". Medicine. 79 (3): 135–154. Unknown parameter
|month=ignored (help) - ↑ Riley, AL (1977). "Renal proximal tubular dysfunction and paroxysmal nocturnal hemoglobinuria". Am J Med. 62 (1): 125–9. Unknown parameter
|month=ignored (help) - ↑ Skinner, R (2003). "Chronic ifosfamide nephrotoxicity in children". Medical and Pediatric Oncology. 41 (3): 190–197. Unknown parameter
|month=ignored (help) - ↑ Rodriguez, Soriano J (2002). "Renal tubular acidosis: the clinical entity" (PDF). J Am Soc Nephrol. 13 (8): 2160–70. Unknown parameter
|month=ignored (help) - ↑ McSherry, E (1981). "Renal tubular acidosis in childhood". Kidney International. 20: 799.
- ↑ Fathallah, D. M. (1997). "Carbonic anhydrase II (CA II) deficiency in Maghrebian patients: evidence for founder effect and genomic recombination at the CA II locus" (PDF). Human Genetics (99): 634–637. 10.1007/s004390050419.
- ↑ 30.0 30.1 DeFronzo, RA (1980). "Hyperkalemia in hyporeninemic hypoaldosteronism". Kidney International (17): 118.
- ↑ Sebastian, A (1984). "Amelioration of hyperchloremic acidosis with furosemide therapy in patients with chronic renal insufficiency and type 4 renal tubular acidosis". Am J Nephrol. 4 (5): 287–300.