Relapsing fever: Difference between revisions
| Line 42: | Line 42: | ||
==Treatment== | ==Treatment== | ||
[[Relapsing fever medical therapy|Medical therapy]] | [[Relapsing fever surgery|Surgical options]] | [[Relapsing fever primary prevention|Primary prevention]] | [[Relapsing fever secondary prevention|Secondary prevention]] | [[Relapsing fever cost-effectiveness of therapy|Financial costs]] | [[Relapsing fever future or investigational therapies|Future therapies]] | [[Relapsing fever medical therapy|Medical therapy]] | [[Relapsing fever surgery|Surgical options]] | [[Relapsing fever primary prevention|Primary prevention]] | [[Relapsing fever secondary prevention|Secondary prevention]] | [[Relapsing fever cost-effectiveness of therapy|Financial costs]] | [[Relapsing fever future or investigational therapies|Future therapies]] | ||
== Diagnosis == | == Diagnosis == | ||
Revision as of 17:04, 7 February 2012
For patient information click here
| Relapsing fever | |
| ICD-10 | A68 |
|---|---|
| ICD-9 | 087 |
| DiseasesDB | 1547 |
| eMedicine | emerg/590 med/1999 |
| MeSH | D012061 |
|
Relapsing fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Relapsing fever On the Web |
|
American Roentgen Ray Society Images of Relapsing fever |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Historical Perspective
Pathophysiology
Epidemiology & Demographics
Risk Factors
Screening
Causes
Differentiating Relapsing fever
Complications & Prognosis
Diagnosis
History and Symptoms | Physical Examination | Laboratory tests | Electrocardiogram | X Rays | CT | MRI Echocardiography or Ultrasound | Other images | Alternative diagnostics
Treatment
Medical therapy | Surgical options | Primary prevention | Secondary prevention | Financial costs | Future therapies
Diagnosis
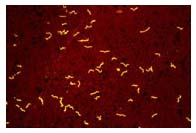

- The definitive diagnosis of TBRF is based on the observation of Borrelia spirochetes in smears of peripheral blood, bone marrow, or cerebrospinal fluid in a symptomatic person. Although best visualized by dark field microscopy, the organisms can also be detected by Wright-Giemsa or acridine orange-stained preparations.
- The organisms are best detected in blood obtained while a person is febrile. With subsequent febrile episodes, the number of circulating spirochetes decreases, making it harder to detect spirochetes on a peripheral blood smear. Even during the initial episode spirochetes will only be seen 70% of the time.
Blood samples obtained before antibiotic treatment can be cultured using BSK medium or by inoculating immature mice. The spirochete will usually be evident within 24 hours if the blood was drawn during a febrile episode.
Although not valuable for making an immediate diagnosis, serologic testing is available through public health laboratories and some private laboratories. Acute serum should be taken within 7 days of symptom onset and convalescent serum should be taken at least 21 days after symptoms start. Early antibiotic treatment may blunt the antibody response and the antibody levels may wane quickly during the months after exposure. To confirm the diagnosis of TBRF, Borrelia specific antibody titers should be increased between acute and convalescent serum samples and convalescent serum antibody levels should be at least two standard deviations above pooled negative controls. Serologic testing for TBRF is not standardized and results may vary by lab. Patients with TBRF may have false-positive tests for Lyme disease because of the similarity of proteins between the two organisms.
Incidental laboratory findings include normal to increased white blood cell count with a left shift towards immature cells, a mildly increased serum bilirubin level, mild to moderate thrombocytopenia (low platelet count), elevated ESR and slightly prolonged coagulation tests, PT and APTT.
Differential Diagnosis
The following infectious disease should be consider in someone with recurrent episodes of a febrile illness:
Colorado tick fever, Infectious mononucleosis, Ascending (intermittent) cholangitis, Yellow fever, African hemorrhagic fevers, Lymphocytic choriomengitis, Dengue fever, Leptospirosis, Infections with echovirus 9, Malaria, Chronic meningococcemia, Infections with Bartonella species, Brucellosis, Rat bite fever.[1]
Treatment
Pharmacotherapy
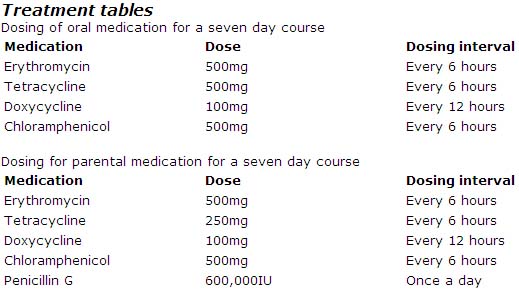
Erythromycin, tetracyclines, chloramphenicol, or penicillins have all been shown to be effective for treating TBRF. Although duration of therapy has not been well studied for TBRF, the current recommendation is seven days of antibiotic therapy. In contrast, LBRF caused by B. recurrentis can be treated with a single dose of antibiotics.
For young children and pregnant women either erythromycin and/or penicillin are recommended for treatment of TBRF.
When initiating antibiotic therapy, a patient should be watched closely for a Jarisch-Herxheimer reaction for the first 4 hours after the antibiotic is given (Negussie, Remick et al. 1992). The reaction may be difficult to distinguish from a febrile crisis, with rigors and decreased blood pressure. Cooling blankets and appropriate use of antipyrectic agents may be indicated. The Jarisch-Herxheimer reaction produces apprehension, diaphoresis, fever, tachycardia, and tachypnea with an initial pressor response followed rapidly by hypotension. Recent studies have shown that tumor necrosis factor-alpha (TNF-alpha) may be partly responsible for the reaction.
Acute Pharmacotherapies
The CDC has not developed specific treatment guidelines for TBRF. Below are the treatment recommendations as outlined in Harrisons Principles of Internal Medicine. 16th edition. 2004. p 994.
Prevention
In order to prevent relapsing fever, one should:
- Avoid sleeping in rodent infested buildings.
- Limit tick bites by using insect repellent containing DEET (on skin or clothing) or permethrin (applied to clothing or equipment).
- Rodent-proof buildings in areas where the disease is known to occur.
- Identify and remove any rodent nesting material from walls, ceilings and floors.
- In combination with removing the rodent material, fumigate the building with preparations containing pyrethrins and permethrins. More than one treatment is often needed to effectively rid the building of the vectors, the soft-ticks. Always folllow product product instructions, and consider consulting a liscensed pest control specialist.[3]
See also
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson M.S., M.D.
List of contributors:
Pilar Almonacid