Radiation safety
|
WikiDoc Resources for Radiation safety |
|
Articles |
|---|
|
Most recent articles on Radiation safety Most cited articles on Radiation safety |
|
Media |
|
Powerpoint slides on Radiation safety |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Radiation safety at Clinical Trials.gov Trial results on Radiation safety Clinical Trials on Radiation safety at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Radiation safety NICE Guidance on Radiation safety
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Radiation safety Discussion groups on Radiation safety Patient Handouts on Radiation safety Directions to Hospitals Treating Radiation safety Risk calculators and risk factors for Radiation safety
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Radiation safety |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editors-In-Chief: Alexandra Almonacid M.D. and Jeffrey J. Popma M.D.
Radiation Safety Regulations
- The Massachusetts Department of Public Health regulates the use of fluoroscopy in hospitals – all non-radiologist personnel that use flouroscopy must have documented training (Code DPH 105 CMR 120.405)
- The FDA and Nuclear Regulatory Commissions have provided summary recommendations and equipment requirements but do not regulate flouroscopy at hospitals
- Recent FDA mandate that angiographic system manufactured after June 2006 must have cumulative time readouts, in addition to 5-minute time alerts
- Significant medicolegal and regulatory implications for noncompliance with the policy
- Additional DPH Training Requirements Effective October 2006
- All non-radiologist physician flouroscopic operators must be trained annually in flouroscopy and radiation safety. MDs must also be trained for the correct operation of the equipment that they use.
- Hospitals must provide a privileging program for properly-qualified non-radiology physicians to use flouroscopy
- Written policies and procedures covering these requirements must be prepared and maintained
- For each operating flouroscopy unit, each flouro exposure must be logged showing patient ID, procedure, operator, flouro times, spot films
- A procedure to identify cases where the skin entry dose exceeds 100 Rads
- Investigation must include fluoro time to dose conversions considering patient positioning, movement of the entrance beam, flouroparameters, such as pulsing, mag view, high dose recording fluoro, number and dose of spot films
- doses above 100 Rads to be entered into the patient record and reported to the RSC
- Additional Procedure Logging Requirements Effective October 2006
- Careful ongoing review of each case is required as it progresses to determine whether the 100 Rad dose is exceeded
- The combined effort of the procedure team at the end of the procedure to best estimate times associated with radiation exposure, including spot films, high dose rate imaging procedures, and patient positions, height, and wt
- Full documentation must be forwarded to a qualified person knowledgeable in the equipment used to obtain a best estimate of a maximum skin-entry patient dose for proper documentation and recording
- State regulations now require that a log book be kept with each flouroscopic unit and that each flouro examination is recorded with the flouro time and number of spot films
- The identity of the flouro operator and an appropriate identification number of the patient for each procedure must be included in the entry logs
- Flouroscopic logs must be maintained in auditable form for at least 5 years and must be available to State Radiation Inspection Program inspectors on demand
- Assessment of Liability in the Event of an Adverse Outcome
- Equipment manufacturer
- Operator must be provided with an indication of whether the “last image hold” image is a “freeze frame” fluoro image or a radiographic image
- New fluoro equipment must be equipped to provide a readout of the skin-entry dose rate for a patient properly positioned on the X-ray table
- A cumulative readout of skin-entry dose must be available as the case progresses
- Data displayed as Air-Kerma-Rate (AKR) and Cumulative Air-Kerma (CAK) must be distinguishable in the readouts
- The units displayed will be mGy/min (AKR) and mGy (CAK)
- Physician performing the procedure
- Medical Facility
- Equipment manufacturer
Radiation Safety Training
Principles and operation of fluoroscopy
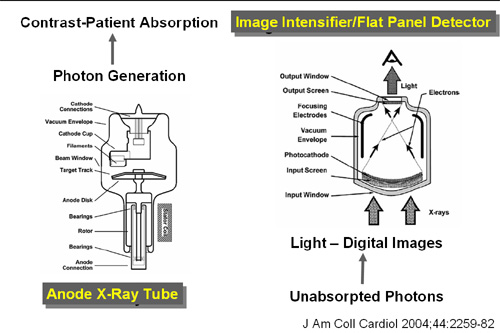
- Physics and Nature of X-Radiation (1)
- X-rays are described in photons, comprised of a discrete packet of electromagnetic radiation containing a defined amount of radiation (quantum)
- An X-ray photon contains 5,000 to 75,000 times as much energy as a visible light photon. **For example, there are 2 electron volts for green light and between 10,000-15,000 electron volts for X-ray
- The differences in the biologic effects of light and X-ray relates to the energy differences between the two modalities
- Parameters Affecting X-Ray Images (1)
- X-ray beam penetrating power: Increasing the kVp of the X-ray beam decrease its absorption, reducing patient exposure. However, increasing the kVP also decreases the differences in the relative absorption of the different tissues, reducing image contrast
- X-ray beam filtration: “Hardening the beam” with aluminum and copper filtration reduces skin injury
- Scatter radiation: increases with size of X-ray field and can be reduced with collimators
- Image noise: “quantum mottling”
- Moving the X-Ray Tube Closer to the Patient Has the Following Effects: Increases the patient skin exposure and results in blurring (unsharpness) in the image
- Positioning of the Image Intensifier Closer to the Patient Has the Following Effects: Reduces the patient skin exposure and enhances the image quality
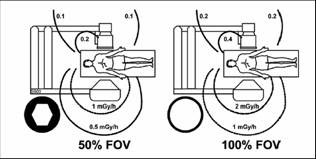
- Collimation: Collimate tightly to the area of interest.
- Reduces the patient’s total entrance skin exposure.
- Improves image contrast.
- Scatter radiation to the operator will also decrease.
- Collimators:
- Tighter collimation decreases the potential for scatter radiation production
- “Coning down” reduces patient risk since less tissue is being irradiated
- Operator exposure can be reduced when collimators are used effectively
- Scatter radiation increase image noise, thereby reducing image contrast
- Collimators:
Biologic effects of x-rays
- Commonly used radiation units: Roentgen (R), Rad, Gray (Gy), Rem, Sievert (Sv).
- Expected Radiation Exposure
- Average annual radiation dose for each person in the US due to natural background radiation is approximately 300 mrem
- The maximum allowable effective who body dose to a physician performing radiological procedures is 5000 mrem per year
- The As-Low-As-Reasonably Achievable (ALARA) goal is to limit annual occupational exposure to less than 10% of the maximum permissible or less than 500 mrem per year
- Factors Leading to More Skin Injury With Oblique Angiographic Projections
- X-ray beam traverses thicker portions of the patient
- Wider span of anatomy irridadiated on an individual plan causes skin surfaces to be closer to the X-ray tube than intended
- Rotating between oblique and perpendicular views can cause the x-ray tube to be closure than intended
- Underreportimg radiation skin deffects
- Skin damage is often located in regions not visible to the patient
- Due to latency, skin injury expression can be weeks to months after the procedure
- Physicians are relatively unaware of the possibility of this occurrence
- Radiation exposure reporting : In the event of a large fluoroscopic exposure, a significant skin reaction may be delayed. The following individuals should be notified of the excessive exposure: Radiation Safety Officer, the primary care physician, entry of an appropriate note in the patient’s medical record
Principles of Radiation Safety
- ALARA (As Low as Reasonably Achievable)
- There is no magnitude of radiation exposure that is completely safe
- The use of a mini-C arm requires the same radiation protection as other flouroscopic systems
- Operators are significantly affected by scatter radiation
- Time, distance, and shielding are primary issues
- MD needs to: Operate equipment in a manner that generates optimal image quality with minimal patient and personnel exposure; recognize circumstances in which risk of radiation injury is increased
- Protection of personnel
- Reducing Fluoroscopy Time
- Use of 5-minute notifications
- Always view the video image while performing fluoroscopy
- Judicious use of last image hold features
- Planning images before radiation to reduce unnecessary panning
- Use record mode only when a permanent record is required
- Use pulse flouroscopy v. continuous
- Distance
- Inverse square law: Halving the distance from the radiation source increases the radiation dose by a factor of 4; Exposure reduction is due to the divergent nature of radiation; Doubling the distance from the radiation source decreases the dose by a fourth; Tripling the distance from the radiation source decreases the dose rate by one ninth
- Double the distance
- One step back from tableside:cuts exposure by factor of 4
- Lateral fluoroscopy: 5x less dose on Image Int. side
- Move Image Int. close to patient:less patient skin exposure; less scatter (more dose interception by tower) sharper image
- Source to Skin Distance (SSD):38 cm for stationary fluoroscopes; 30 cm for mobile fluoroscopes
- Reducing radiation dose
- Limit use of magnification modes to situations where enhanced visualization is necessary
- Avoid opening collimators fully
- Avoid extremely oblique angulations when similar information can be obtained using perpendicular views
- Select the highest tube voltage possible that provides suitable contrast for the procedure
- Shielding
- Bagdes: Massachusetts regulations require that a personnel radiation monitor is worn and that it is placed at the neck (collar) level unshielded
- Aprons: 0.25 mm Pb equivalent. The most common 0.5 mm lead equivalent aprons attenuate about 95% of the scatter radiation to the physician torso. The light weight 0.25 mm lead aprons attenuate about 80% of the scatter radiation to the physician torso
- Thyroid collar, Pb glasses, Pb eye protection
- Ceiling mounted & rollaway shields
- Dosimeters
- Collar and waist badges
- Ring / wrist badges, eye clips
- Dosimeter storage, control badges
- Reducing Fluoroscopy Time
Fluoroscopic Outputs
- Effect of Angulated Views on Exposure
View ......................... Waist level scatter (mR/hr)
Anterior ......................... 34
RAO 30 ......................... 20
LAO 30 ......................... 103
Lateral ......................... 204
High level control options
- Portable C-Arm Systems
- A common error when using the portable C-arm is to place the x-ray tube too close to the patient’s skin when varying the distance is possible
- The image intensifier should be lowered to touch or come close to the skin in order to maximize the distance between the X-ray tube and the skin
- Closing the collimators down to radiate only the tissue of interest will reduce the area and volume of tissue irradiated, thus reducing the whole body effective dose
- Collimation improves image quality
Dose reduction techniques for x-ray systems
- Fluoroscopy Dose Management Issues
- X-ray beam collimation
- Last Image Hold
- Pulsed Fluoroscopy
- Virtual collimator and semitransparent diaphragm control
- X-ray stand position memory
- Acquisition dose management issues
- Digital image subtraction
- Correctable Dose Reduction Factors (1)
- Equipment designs and settings
- Movement capabilities of C-arm, X-Ray Sources, image intensifier
- Field-of-view size
- Collimator position
- Bean filtration
- Fluoroscopy pulse rate and acquisition frame rate
- Fluoroscopy and acquisition input dose rates
- Automatic dose-rate control bean energy management options
- X-ray photon energy spectra
- Software image filters
- Prevention maintenance and calibration
- Quality control
- Patient Factors
- Patient body weight and habitus
- Physician procedure conduct
- Positioning of image intensifier and X-ray source relative to the patient
- Bean orientation and movement
- Detector field-of-view size
- Collimation
- Acquisition and fluoroscopic technique factors on some units
- Fluoroscopy pulse rate
- Acquisition frame rate
- Use of variable bean filtration
- Total fluoroscopy time
- Total acquisition time
- Equipment designs and settings
2011 ACCF/AHA/SCAI Guidelines for Percutaneous Coronary Intervention (DO NOT EDIT)[1]
Radiation Safety (DO NOT EDIT)[1]
| Class I |
|
"1.Cardiac catheterization laboratories should routinely record relevant available patient procedural radiation dose data (eg, total air kerma at the international reference point [Ka,r], air kerma air product [PKA], fluoroscopy time, number of cine images), and should define thresholds with corresponding follow-up protocols for patients who receive a high procedural radiation dose. (Level of Evidence: C)" |
References
- ↑ 1.0 1.1 Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, Khot UN, Lange RA, Mauri L, Mehran R, Moussa ID, Mukherjee D, Nallamothu BK, Ting HH (2011). "2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: Executive Summary A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions" (PDF). Journal of the American College of Cardiology. 58 (24): 2550–83. doi:10.1016/j.jacc.2011.08.006. PMID 22070837. Retrieved 2011-12-08. Text "PDF" ignored (help); Unknown parameter
|month=ignored (help)