Pulmonary nodule CT: Difference between revisions
No edit summary |
|||
| (22 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Solitary pulmonary nodule}} | {{Solitary pulmonary nodule}} | ||
{{CMG}} | {{CMG}}{{AE}}{{MV}} {{JE}} | ||
== | ==Overview== | ||
=== | Computed tomography is the method of choice for the diagnosis of solitary pulmonary nodule. On CT, characteristic findings of solitary pulmonary nodules, include: ground-glass opacity, rounded mass, and less than 30mm.<ref name="pmid8190965">{{cite journal |vauthors=Rosado-de-Christenson ML, Templeton PA, Moran CA |title=Bronchogenic carcinoma: radiologic-pathologic correlation |journal=Radiographics |volume=14 |issue=2 |pages=429–46; quiz 447–8 |year=1994 |pmid=8190965 |doi=10.1148/radiographics.14.2.8190965 |url=}}</ref><ref name="pmid19234288">{{cite journal |vauthors=Parker MS, Chasen MH, Paul N |title=Radiologic signs in thoracic imaging: case-based review and self-assessment module |journal=AJR Am J Roentgenol |volume=192 |issue=3 Suppl |pages=S34–48 |year=2009 |pmid=19234288 |doi=10.2214/AJR.07.7081 |url=}}</ref> The evaluation of solitary pulmonary nodule will depend on 7 characteristics: calcification patterns, size, location, size, growth, shape, margins, attenuation, and contrast enhancement.<ref name="pmid19234288">{{cite journal |vauthors=Parker MS, Chasen MH, Paul N |title=Radiologic signs in thoracic imaging: case-based review and self-assessment module |journal=AJR Am J Roentgenol |volume=192 |issue=3 Suppl |pages=S34–48 |year=2009 |pmid=19234288 |doi=10.2214/AJR.07.7081 |url=}}</ref> | ||
==== | |||
==CT== | |||
* If less than 8 mm, use guidelines | *Computed tomography is the method of choice for the diagnosis of solitary pulmonary nodule | ||
*On CT, characteristic findings of solitary pulmonary nodules, include: | |||
:*Single to multiple intraparenchymal lesion | |||
:*Less than 3 cm in size | |||
:*Rounded or spiculated lesion | |||
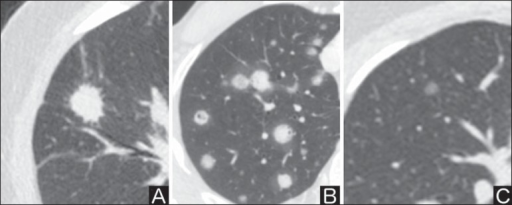
[[File: Solitary pul nodule.png|400px|left|thumb| CT scan showing solitary pulmonary nodules (Picture courtesy: [https://openi.nlm.nih.gov/detailedresult?img=PMC4770395_rb-49-01-0035-g05&query=solitary%20pulmonary%20nodules&it=xg&req=4&npos=15 National Library of Medicine])]] | |||
<br style="clear:left"> | |||
The evaluation of solitary pulmonary nodule will depend on the following characteristics: | |||
'''Calcification''' | |||
*Calcification patterns are commonly seen in granulomatous disease and hamartomas | |||
*Calcification patterns are normally a sign of benignancy | |||
*Characteristic benign calcification patterns of pulmonary nodule, include: | |||
:*Diffuse | |||
:*Central | |||
:*Laminated | |||
:*Popcorn | |||
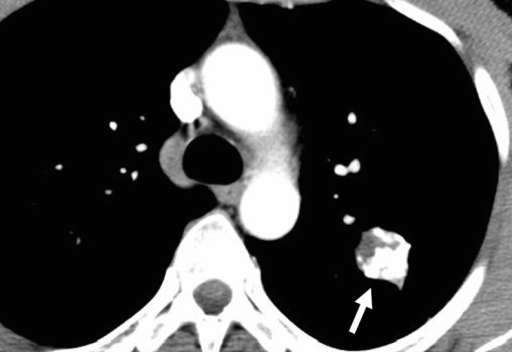
[[File: Calcified lung nodule white arrow.png|400px|left|thumb| CT scan showing a calcified solitary pulmonary nodules (white arrow) (Picture courtesy: [https://openi.nlm.nih.gov/detailedresult?img=PMC3259307_13244_2010_39_Fig6_HTML&query=Calcified%20solitary%20pulmonary%20nodules&it=xg&req=4&npos=2 National Library of Medicine])]] | |||
<br style="clear:left"> | |||
'''Size''' | |||
*Different types of size ranges for pulmonary nodule, include: | |||
:* Nodules less than 4mm | |||
:* Nodules between 4mm and 7mm | |||
:* Nodules between 8mm and 20mm | |||
:* Nodules more than 20mm | |||
'''Location''' | |||
*Locations of pulmonary nodule, include: | |||
:*Perilymphatic | |||
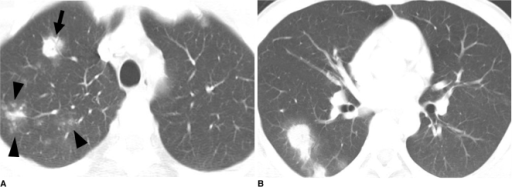
[[File: Perilymphatic solitary pulmonary nodules.jpg |400px|left|thumb| CT scan showing a Perilymphatic solitary pulmonary nodules of [[sarcoidosis]] (Picture courtesy: [https://radiopaedia.org/cases/pulmonary-sarcoidosis?lang=gb Radiopaedia])]] | |||
<br style="clear:left"> | |||
:*Perifissural | |||
[[File: Perifissural solitary pulmonary nodules.png|400px|left|thumb| CT scan showing a Perifissural solitary pulmonary nodule (white circle) (Picture courtesy: [https://en.wikipedia.org/wiki/Lung_nodule#/media/File:CT_of_perifissural_nodule.png Wikipedia])]] | |||
<br style="clear:left"> | |||
:*Centrilobular | |||
[[File: Centrilobular_solitary_pulmonary_nodule.png |400px|left|thumb| CT scan showing a Centrilobular solitary pulmonary nodule (black arrowheads) (Picture courtesy: [https://openi.nlm.nih.gov/detailedresult?img=PMC2893311_kjr-11-407-g003&query=Centrilobular%20solitary%20pulmonary%20nodule&it=xg&req=4&npos=4 National Library of Medicine])]] | |||
<br style="clear:left"> | |||
'''Growth''' | |||
*The growth pattern of the pulmonary nodule plays an important role in the management strategy.<ref name="pmid22156993">{{cite journal |vauthors=Ko JP, Berman EJ, Kaur M, Babb JS, Bomsztyk E, Greenberg AK, Naidich DP, Rusinek H |title=Pulmonary Nodules: growth rate assessment in patients by using serial CT and three-dimensional volumetry |journal=Radiology |volume=262 |issue=2 |pages=662–71 |year=2012 |pmid=22156993 |pmc=3267080 |doi=10.1148/radiol.11100878 |url=}}</ref> | |||
*Nodule growth should be evaluated on a individual basis and based on the risk assessment score | |||
* A 4x growth is associated with a 50% risk of malignancy<ref name="pmid22156993">{{cite journal |vauthors=Ko JP, Berman EJ, Kaur M, Babb JS, Bomsztyk E, Greenberg AK, Naidich DP, Rusinek H |title=Pulmonary Nodules: growth rate assessment in patients by using serial CT and three-dimensional volumetry |journal=Radiology |volume=262 |issue=2 |pages=662–71 |year=2012 |pmid=22156993 |pmc=3267080 |doi=10.1148/radiol.11100878 |url=}}</ref> | |||
'''Shape''' | |||
*Different types of shape for pulmonary nodule, include: | |||
:*Polygonal | |||
:*Spherical | |||
'''Margins''' | |||
*Different types of margins for pulmonary nodule, include: | |||
:*Lobulated or scalloped margins | |||
::*Intermediate malignancy probability | |||
:*Smooth margins | |||
:*:Associated with nodule benignancy | |||
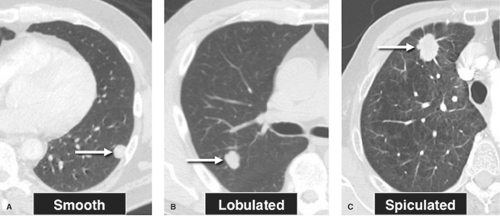
[[File: Pul nodule borders.png|400px|left|thumb| CT scan showing types of solitary pulmonary nodule margins (Picture courtesy: [https://radiologykey.com/pulmonary-neoplasms-4/ Radiologykey])]] | |||
<br style="clear:left"> | |||
'''Attenuation''' | |||
*Different types of attenuation for pulmonary nodule, include: | |||
*Solid pulmonary nodules | |||
:*Malignancy rate of only 7% | |||
*Calcified pulmonary nodules | |||
*Partly solid pulmonary nodules | |||
:*Malignancy rate of 63% | |||
*Ground glass pulmonary nodules | |||
:*Malignancy rate of 18% | |||
'''Contrast enhancement''' | |||
* Contrast enhancement of pulmonary nodules may be useful to determine benign or malignant features | |||
* Benign pulmonary nodules usually have a contrast enhancement less than 15 HU | |||
On CT, radiological signs of pulmonary nodule, include: | |||
*'''Corona radiata sign''': highly associated with malignancy | |||
*'''Air bronchogram sign''': airway surrounded by collection in alveolar spaces, non-specific sign | |||
*'''Halo sign''': zone of ground-glass attenuation surrounding a pulmonary nodule or mass on CT images | |||
*'''Tree-in-bud sign''': CT appearance of multiple areas of centrilobular nodules with a linear branching pattern | |||
*'''Cheerio sign''': pulmonary nodules with a central lucent cavity as seen on CT. It is due to proliferation of (malignant or non-malignant) cells around an airway | |||
==CT Surveillance== | |||
According to the [[American College of Chest Physicians]] (ACCP) for the CT surveillance of pulmonary nodules, recommends the following:<ref name="pmid23649456">{{cite journal| author=Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP et al.| title=Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. | journal=Chest | year= 2013 | volume= 143 | issue= 5 Suppl | pages= e93S-120S | pmid=23649456 | doi=10.1378/chest.12-2351 | pmc=PMC3749714 | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23649456 }} </ref> | |||
* If less than 8 mm, use guidelines by the Fleischner society (see table below). | |||
* For nodules greater than 8 mm in diameter, assess the patients risk of complications from thoracic surgery: | * For nodules greater than 8 mm in diameter, assess the patients risk of complications from thoracic surgery: | ||
** If low to moderate risk for complications of surgery, assess probability of cancer by a validated calculation. The model developed at the Mayo Clinic has been the most extensively validated<ref name="pmid9129544">{{cite journal| author=Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES| title=The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. | journal=Arch Intern Med | year= 1997 | volume= 157 | issue= 8 | pages= 849-55 | pmid=9129544 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9129544 }} </ref> | ** If low to moderate risk for complications of surgery, assess probability of cancer by a validated calculation. The model developed at the Mayo Clinic has been the most extensively validated. An open-source version is [https://openrules.ocpu.io/home/www/pulmnodule.html available online]. | ||
** If high risk for complications of surgery, assess probability of cancer by a validated calculation. If low to moderate risk of cancer follow up with CT scan surveillance. If moderate to high risk of cancer obtain non-surgical biopsy.<ref name="pmid9129544">{{cite journal| author=Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES| title=The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. | journal=Arch Intern Med | year= 1997 | volume= 157 | issue= 8 | pages= 849-55 | pmid=9129544 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9129544 }} </ref> | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ Fleischner | |+ Fleischner Society guidelines for follow-up and management of nodules <8 mm <br>Detected incidentally at non-screening CT<ref name="pmid16244247">{{cite journal| author=MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP et al.| title=Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. | journal=Radiology | year= 2005 | volume= 237 | issue= 2 | pages= 395-400 | pmid=16244247 | doi=10.1148/radiol.2372041887 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16244247 }} </ref> | ||
! Nodule Size (mm) | ! Nodule Size (mm) | ||
! | ! Low risk patients† | ||
! | ! High risk patients‡ | ||
|- | |- | ||
| <= 4 | | <= 4 | ||
| No follow-up needed | | No follow-up needed | ||
| Follow-up at 12 months. If no change, no further imaging needed | | Follow-up at 12 months.<br> If no change, no further imaging needed | ||
|- | |- | ||
| >4 - 6 | | > 4 - 6 | ||
| Follow-up at 12 months. If no change, no further imaging needed | | Follow-up at 12 months.<br>If no change, no further imaging needed | ||
| Initial follow-up CT at 6 -12 months | | Initial follow-up CT at 6 -12 months <br>If no change follow-up CT at 18 - 24 months | ||
|- | |- | ||
| >6 - 8 | | > 6 - 8 | ||
| Initial follow-up CT at 6 -12 months | | Initial follow-up CT at 6 -12 months<br>If no change follow-up CT at 18 - 24 months | ||
| Initial follow-up CT at 3 - 6 months | | Initial follow-up CT at 3 - 6 months<br> >If no change follow-up CT at 9 -12 and 24 months | ||
|- | |- | ||
| >8 | | > 8 | ||
| Follow-up | | Follow-up CT at around 3, 9, and 24 months<br>Dynamic contrast enhanced CT, PET, and/or biopsy | ||
| Same at for low risk patients | | Same at for low risk patients | ||
|- | |- | ||
| colspan="3" |† Low risk patients: Minimal or absent history of smoking and of other known risk factors.<br />‡ High risk patients: History of smoking or of other known risk factors | | colspan="3" |† Low risk patients: Minimal or absent history of smoking and of other known risk factors.<br />‡ High risk patients: History of smoking or of other known risk factors | ||
|} | |} | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{WH}} | {{WH}} | ||
{{WS}} | {{WS}} | ||
| Line 86: | Line 130: | ||
[[Category:Disease]] | [[Category:Disease]] | ||
[[Category:Pulmonology]] | [[Category:Pulmonology]] | ||
Latest revision as of 17:56, 22 July 2020
|
Pulmonary Nodule Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Pulmonary nodule CT On the Web |
|
American Roentgen Ray Society Images of Pulmonary nodule CT |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2] Joanna Ekabua, M.D. [3]
Overview
Computed tomography is the method of choice for the diagnosis of solitary pulmonary nodule. On CT, characteristic findings of solitary pulmonary nodules, include: ground-glass opacity, rounded mass, and less than 30mm.[1][2] The evaluation of solitary pulmonary nodule will depend on 7 characteristics: calcification patterns, size, location, size, growth, shape, margins, attenuation, and contrast enhancement.[2]
CT
- Computed tomography is the method of choice for the diagnosis of solitary pulmonary nodule
- On CT, characteristic findings of solitary pulmonary nodules, include:
- Single to multiple intraparenchymal lesion
- Less than 3 cm in size
- Rounded or spiculated lesion
The evaluation of solitary pulmonary nodule will depend on the following characteristics:
Calcification
- Calcification patterns are commonly seen in granulomatous disease and hamartomas
- Calcification patterns are normally a sign of benignancy
- Characteristic benign calcification patterns of pulmonary nodule, include:
- Diffuse
- Central
- Laminated
- Popcorn
Size
- Different types of size ranges for pulmonary nodule, include:
- Nodules less than 4mm
- Nodules between 4mm and 7mm
- Nodules between 8mm and 20mm
- Nodules more than 20mm
Location
- Locations of pulmonary nodule, include:
- Perilymphatic

- Perifissural

- Centrilobular
Growth
- The growth pattern of the pulmonary nodule plays an important role in the management strategy.[3]
- Nodule growth should be evaluated on a individual basis and based on the risk assessment score
- A 4x growth is associated with a 50% risk of malignancy[3]
Shape
- Different types of shape for pulmonary nodule, include:
- Polygonal
- Spherical
Margins
- Different types of margins for pulmonary nodule, include:
- Lobulated or scalloped margins
- Intermediate malignancy probability
- Smooth margins
- Associated with nodule benignancy
Attenuation
- Different types of attenuation for pulmonary nodule, include:
- Solid pulmonary nodules
- Malignancy rate of only 7%
- Calcified pulmonary nodules
- Partly solid pulmonary nodules
- Malignancy rate of 63%
- Ground glass pulmonary nodules
- Malignancy rate of 18%
Contrast enhancement
- Contrast enhancement of pulmonary nodules may be useful to determine benign or malignant features
- Benign pulmonary nodules usually have a contrast enhancement less than 15 HU
On CT, radiological signs of pulmonary nodule, include:
- Corona radiata sign: highly associated with malignancy
- Air bronchogram sign: airway surrounded by collection in alveolar spaces, non-specific sign
- Halo sign: zone of ground-glass attenuation surrounding a pulmonary nodule or mass on CT images
- Tree-in-bud sign: CT appearance of multiple areas of centrilobular nodules with a linear branching pattern
- Cheerio sign: pulmonary nodules with a central lucent cavity as seen on CT. It is due to proliferation of (malignant or non-malignant) cells around an airway
CT Surveillance
According to the American College of Chest Physicians (ACCP) for the CT surveillance of pulmonary nodules, recommends the following:[4]
- If less than 8 mm, use guidelines by the Fleischner society (see table below).
- For nodules greater than 8 mm in diameter, assess the patients risk of complications from thoracic surgery:
- If low to moderate risk for complications of surgery, assess probability of cancer by a validated calculation. The model developed at the Mayo Clinic has been the most extensively validated. An open-source version is available online.
- If high risk for complications of surgery, assess probability of cancer by a validated calculation. If low to moderate risk of cancer follow up with CT scan surveillance. If moderate to high risk of cancer obtain non-surgical biopsy.[5]
| Nodule Size (mm) | Low risk patients† | High risk patients‡ |
|---|---|---|
| <= 4 | No follow-up needed | Follow-up at 12 months. If no change, no further imaging needed |
| > 4 - 6 | Follow-up at 12 months. If no change, no further imaging needed |
Initial follow-up CT at 6 -12 months If no change follow-up CT at 18 - 24 months |
| > 6 - 8 | Initial follow-up CT at 6 -12 months If no change follow-up CT at 18 - 24 months |
Initial follow-up CT at 3 - 6 months >If no change follow-up CT at 9 -12 and 24 months |
| > 8 | Follow-up CT at around 3, 9, and 24 months Dynamic contrast enhanced CT, PET, and/or biopsy |
Same at for low risk patients |
| † Low risk patients: Minimal or absent history of smoking and of other known risk factors. ‡ High risk patients: History of smoking or of other known risk factors | ||
References
- ↑ Rosado-de-Christenson ML, Templeton PA, Moran CA (1994). "Bronchogenic carcinoma: radiologic-pathologic correlation". Radiographics. 14 (2): 429–46, quiz 447–8. doi:10.1148/radiographics.14.2.8190965. PMID 8190965.
- ↑ 2.0 2.1 Parker MS, Chasen MH, Paul N (2009). "Radiologic signs in thoracic imaging: case-based review and self-assessment module". AJR Am J Roentgenol. 192 (3 Suppl): S34–48. doi:10.2214/AJR.07.7081. PMID 19234288.
- ↑ 3.0 3.1 Ko JP, Berman EJ, Kaur M, Babb JS, Bomsztyk E, Greenberg AK, Naidich DP, Rusinek H (2012). "Pulmonary Nodules: growth rate assessment in patients by using serial CT and three-dimensional volumetry". Radiology. 262 (2): 662–71. doi:10.1148/radiol.11100878. PMC 3267080. PMID 22156993.
- ↑ Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP; et al. (2013). "Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines". Chest. 143 (5 Suppl): e93S–120S. doi:10.1378/chest.12-2351. PMC 3749714. PMID 23649456.
- ↑ Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES (1997). "The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules". Arch Intern Med. 157 (8): 849–55. PMID 9129544.
- ↑ MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP; et al. (2005). "Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society". Radiology. 237 (2): 395–400. doi:10.1148/radiol.2372041887. PMID 16244247.