Pulmonary atresia
For patient information click here
| Pulmonary atresia | ||
 | ||
|---|---|---|
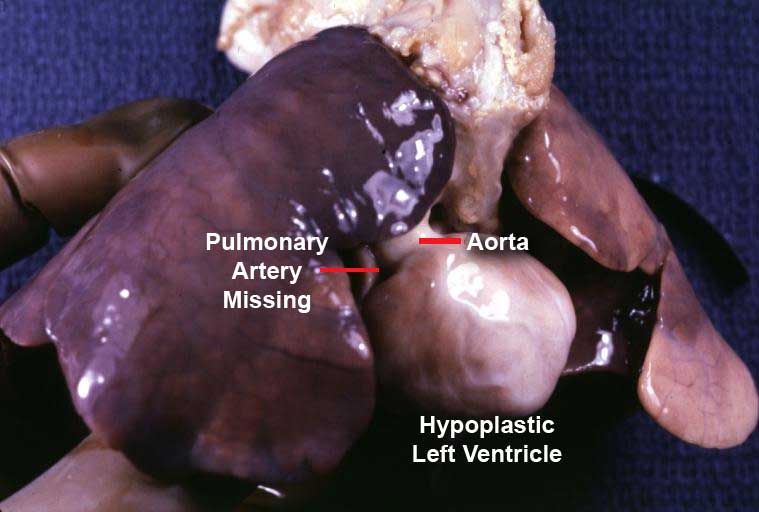
| Only an aorta can be seen originating from this pathology specimen. No pulmonary artery is present. | ||
| ICD-10 | Q25.5 | |
| ICD-9 | 747.3 | |
| MedlinePlus | 001091 | |
| MeSH | C14.240.670 | |
|
WikiDoc Resources for Pulmonary atresia |
|
Articles |
|---|
|
Most recent articles on Pulmonary atresia Most cited articles on Pulmonary atresia |
|
Media |
|
Powerpoint slides on Pulmonary atresia |
|
Evidence Based Medicine |
|
Cochrane Collaboration on Pulmonary atresia |
|
Clinical Trials |
|
Ongoing Trials on Pulmonary atresia at Clinical Trials.gov Trial results on Pulmonary atresia Clinical Trials on Pulmonary atresia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pulmonary atresia NICE Guidance on Pulmonary atresia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pulmonary atresia Discussion groups on Pulmonary atresia Patient Handouts on Pulmonary atresia Directions to Hospitals Treating Pulmonary atresia Risk calculators and risk factors for Pulmonary atresia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pulmonary atresia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Pulmonary atresia is a congenital malformation of the pulmonary valve in which the valve orifice fails to develop. Atresia means "no opening". The valve is completely closed thereby obstructing the outflow of blood from the heart to the lungs.
Oxygen-poor blood travels directly from the right atrium to the left side of the heart through a shunt (patent foramen ovale or any other type of atrial septal defect). This oxygen-poor blood is then pumped through the aorta to the rest of the body, making fingers, toes, and lips appear blue or cyanotic.
Babies with this type of cyanotic congenital heart disease survive only for the first few days of life while the normal fetal shunts (patent ductus arteriousus, patent foramen ovale) between left and right circulations remain patent. Without an operation in that period to open the pulmonary valve or to make a shunt between the aorta and the pulmonary arteries, the condition is fatal.
The type of surgery recommended depends on the size of the right ventricle and the pulmonary artery. If they are normal in size and the right ventricle is able to pump blood, open heart surgery can be performed to make blood flow through the heart in a normal pattern. If the right ventricle is small and unable to act as a pump, doctors may perform an operation called the Fontan procedure. In this procedure, the right atrium is connected directly to the pulmonary artery. Many children with Pulmonary Atresia will go on to lead 'normal' lives.
Pathophysiology
The pulmonary valve is located on the right side of the heart between the right ventricle and pulmonary artery. In a normal functioning heart, the opening to the pulmonary valve has three flaps that open and close like one way doors. As these flaps open and close they force blood to flow forward into the pulmonary artery and backward into the right ventricle then forward again to the lungs where the blood becomes oxygenated. With the disease pulmonary atresia, the flap-like openings are completely covered by a layer of tissue, thus preventing the ability of blood flow to the lungs to become oxygenated. The body requires oxygenated blood for survival. Pulmonary atresia is not threatening to a developing fetus however, because the mother's placenta provides the needed oxygen since the baby's lungs are not yet functional. Once the baby is born its lungs must now provide the oxygen needed for survival, but with Pulmonary atresia there is no opening on the pulmonary valve for blood to get to the lungs and become oxygenated. Due to this, the newborn baby is blue in color and pulmonary atresia can usually be diagnosed within hours or minutes after birth.
Classification
There are two forms of pulmonary atresia.
Pulmonary atresia with intact ventricular septum (PA-IVS)
PA-IVS is a rare congenital lesion. This lesion can be diagnosed during the fetal stage of life by using fetal echocardiography, which is a test that uses sound waves to look at the structure of an unborn baby's heart. PA-IVS involves complete blockage of the pulmonary valve located on the right side of the heart. This blockage thus prevents the flow of blood to the lungs. Because of this lack of blood flowing through the right side of the heart, the structures on that side, such as the pulmonary valve and the tricuspid valve, are abnormally small. The genetic cause of PA-IVS is unknown. It is rare, occurring in around 7.1-8.1 per every 100,000 live births.
With intact ventricular septum: complex cardiac lesion characterized by one of two patterns of pathophysiology.
Type I disease
In this particular type, there is a combination of pulmonary valvular atresia, competent tricuspid valve, and an intact ventricular septum. As a consequence a right ventricular hypertrophy and chamber obliteration with suprasystemic pressures is developed, which force blood through the myocardial sinusoids that feed the right ventricle into the coronary circulation.
Type II disease
This type consist of proximal pulmonary arterial atresia , an intact ventricular septum, but the tricuspid valve is incompetence allowing retrograde flow of blood into the right atrium and across an atrial septal defect. TTherefore, the right ventricle is either normal or dilated.
Survival has improved due to a combination of the early treatment with Prostaglandin PGE1 (to prevent the PDA from closing) and advances in cardiac surgery (creating shunts between the aorta and the pulmonary artery that may help increase blood flow to the lungs). A more complete repair will depends on the size of the pulmonary artery and right ventricle.
Pulmonary atresia with ventricular septal defect or VSD
PA-VSD is identified by underdevelopment of the right ventricle. It is a second opening in the ventricular wall. This opening provides a way out for blood in the right ventricle. When this second opening (VSD) does not exist, very little blood goes to the right ventricle, which is what causes it to be underdeveloped. This defect can also be determined before birth. Out of all congenital cardiac malformations, it is estimated that PA-VSD occurs in 2.5-3.4% of the cases. The genetic cause of PA-VSD is not known; it is found however, that children whose parents have PA-VSD are at a higher risk for congenital heart lesions.
Images shown below is courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
Clinical Symptoms
Symptoms are noted shortly after birth. The most common presentation is a newborn who becomes cyanotic (blue) in the transitional first day of life when the placenta (maternal source of oxygen) is removed. Cyanosis is related to the presence of other defects that allow blood to mix, such as a patent ductus arteriosus, patent foramen ovale, etc. Other symptoms may include rapid breathing, lethargy, irritability, etc.
Treatment
At first, the child will need to be admitted to the intensive care unit and possibly placed on oxygen and a ventilator that will help the child breathe. Also, IV medications that assist the heart and lung function may be given. An IV medication called prostaglandin E1 is used for treatment of pulmonary atresia. This medication helps the blood circulate through the body, but it is extremely dangerous because it causes apnea. Another example of preliminary treatment is heart catheterization to evaluate the defect or defects of the heart; this procedure is much more invasive. Ultimately, however, the patient will need to have a series of surgeries to improve the blood flow permanently. The first surgery will likely be performed shortly after birth. A shunt can be created between the aorta and the pulmonary artery to help increase blood flow to the lungs. As the child grows, so does the heart and the shunt may need revised in order to meet the body's requirements. Children with pulmonary atresia will need to be seen regularly throughout their lifetime by a cardiologist to be sure that their heart is functioning properly. Due to their increased risk of endocarditis, children diagnosed with pulmonary atresia should have amoxicillin before any type of dental work or other types of surgeries to help prevent this infection from occurring.
The type of surgery recommended depends on the size of the right ventricle and the pulmonary artery. If they are normal in size and the right ventricle is able to pump blood, open heart surgery can be performed to make blood flow through the heart in a normal pattern. If the right ventricle is small and unable to act as a pump, doctors may perform another type of operation called the Fontan procedure. In this two-stage procedure, the right atrium is disconnected from the pulmonary circulation. The systemic venous return goes directly to the lungs, by-passing the heart.
Prognosis
The outcome varies for every child. If the condition is left uncorrected it is fatal, but the prognosis has greatly improved over the years for babies with pulmonary atresia. Some factors that affect how well the child does include how well the heart is beating, the condition of the blood vessels that supply the heart, and how leaky the other heart valves are. Most cases of pulmonary atresia can be helped with surgery. If the patient's right ventricle is exceptionally small, many surgeries will be needed in order to help stimulate normal circulation of blood to the heart.
If uncorrected, babies with this type of congenital heart disease will only survive for the first few days of life while the fetal shunts between left and right circulations remain patent.
Many children with Pulmonary Atresia will go on to lead 'normal' lives.
Doctors are unsure of the cause of congenital heart defects, but there are some medical conditions that have been found to increase the risk of having a baby with a heart defect such as congenital heart disease in the mother, father, brother, or sister of the baby, a diabetic mother, use of drugs or alcohol or over the counter prescriptions during pregnancy. These conditions do not mean that the baby will definitely be born with a heart defect, but that it runs a higher chance. Sometimes babies are born without any of these conditions; the cause is unknown. All pregnant women should do all that they can to ensure and maintain the health of their unborn child.
General Management
Patient should be treated in the intensive care unit (ICU) or special care nursery once symptoms are noted. The patient will need oxygen, and possibly even a ventilator, to assist his/her breathing. Intravenous (IV) medications may be given to help the heart and lungs function more efficiently.
A cardiac catheterization procedure can be used as a diagnostic procedure, as well as initial treatment procedure as balloon atrial septostomy to improve mixing oxygenated blood and unoxygenated blood between the right and left atria.
Atrial Septostomy: a special catheter with a balloon in the tip is used to create an opening in the atrial septum. The catheter is guided through the foramen ovale to the left atrium (LA). Once the ballon is in the LA is inflated and then pulled back opening a bigger hole between the right atrium and the LA to mix blood.
If the hospital does not have a catheterization lab with skill physician to perform the ballon atrial septostomy, an intravenous medication called prostaglandin is administered to keep the ductus arteriousus from closing.
Those intervention will only allow time to stabilize the baby, because surgery is the definitive treatment to improve blood flow to the lungs
