|
|
| (45 intermediate revisions by 13 users not shown) |
| Line 1: |
Line 1: |
| | {| class="infobox" style="float:right;" |
| | |- |
| | | [[File:Siren.gif|link=Urinary tract infection resident survival guide|41x41px]]|| <br> || <br> |
| | | [[Urinary tract infection resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] |
| | |} |
| {{Infobox Disease | | | {{Infobox Disease | |
| Name = Prostatitis | | | Name = Prostatitis | |
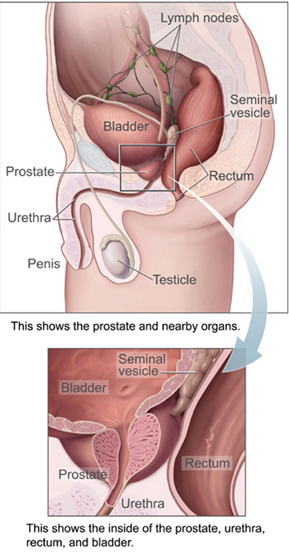
| ICD10 = {{ICD10|N|41| |n|40}} | | | Image = prostatelead.jpg | |
| ICD9 = {{ICD9|601}} |
| | Caption = Image via public domain<ref name="urlFile:Prostata.jpg - Wikimedia Commons">{{cite web |url=https://commons.wikimedia.org/w/index.php?curid=462958 |title=File:Prostata.jpg - Wikimedia Commons |format= |work= |accessdate=}}</ref> |
| Image = prostatelead.jpg |
| |
| Caption = | | |
| DiseasesDB = 10801 |
| |
| eMedicineSubj = |
| |
| eMedicineTopic = |
| |
| eMedicine_mult = |
| |
| MedlinePlus = 000524 |
| |
| MeshName = Prostatitis |
| |
| MeshNumber = D011472 |
| |
| }} | | }} |
| {{Search infobox}}
| | __NOTOC__ |
|
| |
|
| '''Editor(s)-in-Chief:''' [[C. Michael Gibson]], M.S.,M.D. [mailto:mgibson@perfuse.org] Phone:617-632-7753; [[Steven C. Campbell]], M.D., Ph.D., [mailto:campbes3@ccf.org], Phone:216-444-5595 | | {{Prostatitis}} |
| | '''For patient information page on Prostatitis click [[{{PAGENAME}} (patient information)|here]]''' |
|
| |
|
| ==Overview==
| | '''For patient information page on Chronic bacterial prostatitis click [[Chronic bacterial prostatitis (patient information)|here]]''' |
|
| |
|
| '''Prostatitis''' or '''prostitis''' is an [[inflammation]] of the [[prostate]]. Because women do not have a prostate gland, it is a condition found only in [[men]], although women do have microscopic paraurethral [[Skene's gland]]s connected to the distal third of the urethra in the prevaginal space that are homologous to the prostate, and may cause symptoms.<ref name="skene">{{cite journal | author=R F Gittes and R M Nakamura| title=Female urethral syndrome. A female prostatitis?| journal=West J Med.| year=1996| volume=164| issue=5| page=435-438| url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1303542}}</ref>
| | {{CMG}}{{AE}}{{USAMA}} |
|
| |
|
| A prostatitis diagnosis is assigned at 8% of all urologist and 1% of all primary care physician visits in the United States.<ref name="prev">{{cite journal | author=Collins MM et al| title=How common is prostatitis? A national survey of physician visits.| journal=J Urol.| year=1998| volume=159| issue=4| page=1224-1228| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=98167258&dopt=Citation}}</ref>
| | {{SK}} Prostitis; Acute bacterial prostatitis; Chronic bacterial prostatitis; Bacterial prostatitis; |
|
| |
|
| *Mumps is the main reason of increased risk of prostitis in childhood.
| | ==[[Prostatitis overview|Overview]]== |
|
| |
|
| *In adolescents and adults; prostitis is usually a secondary infection (e.g. IBS & Candida).
| | ==[[Prostatitis historical perspective|Historical Perspective]]== |
|
| |
|
| *In elderly, prostitis usually occurs secondary to the enlargement of the gland over a period of years.
| | ==[[Prostatitis classification|Classification]]== |
| | ==[[Prostatitis pathophysiology|Pathophysiology]]== |
|
| |
|
| ==Nomenclature== | | ==[[Prostatitis causes|Causes]]== |
| The term prostatitis refers in its strictest sense to [[histological]] (microscopic) inflammation of the tissue of the prostate gland, although historically the term has loosely been used as a rubric to describe a set of quite different conditions. To try to remedy this, the [[NIH]] devised a new classification system in 1999.
| |
|
| |
|
| ==Classification== | | ==[[Prostatitis differential diagnosis|Differentiating Prostatitis from other Diseases]]== |
| According to the 1999 National Institute of Health (NIH) Classification, there are four categories of prostatitis:
| |
|
| |
|
| * Category I: [[#Category_I:_Acute_prostatitis_.28bacterial.29|Acute prostatitis (bacterial)]]
| | ==[[Prostatitis epidemiology and demographics|Epidemiology and Demographics]]== |
| * Category II: [[#Category_II:_Chronic_bacterial_prostatitis|Chronic bacterial prostatitis]]
| |
| * Category III: [[#Category_III:_CP.2FCPPS |Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS)]]
| |
| :: <span style="font-size: 85%">Subdivisions of IIIa (inflammatory) and IIIb (non-inflammatory) exist based on levels of pus cells in expressed prostatic secretions, but these subcategories are of limited use clinically</span>
| |
| * Category IV: [[#Category_IV:_Asymptomatic_inflammatory_prostatitis|Asymptomatic inflammatory prostatitis]]
| |
|
| |
|
| ==Category I: Acute prostatitis (bacterial)== | | ==[[Prostatitis risk factors|Risk Factors]]== |
|
| |
|
| '''[[Acute (medical)|Acute]] [[prostatitis]]''' is any [[inflammation]] of the [[prostate gland]] that is caused by a sudden infection, usually by bacteria that get into the prostate by traveling up into the body through the [[urethra]]. Some of these bacteria are the normal germs that live on and inside your body. Other infections are transmitted through sexual contact.
| | == [[Prostatitis screening|Screening]] == |
|
| |
|
| Most men who will develop prostatitis have a normal prostate gland, although the infection may be more common in older men as the gland gets larger with age. There is no known link between prostatitis and prostate cancer.
| | ==[[Prostatitis natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| Prostatitis is more common in men with AIDS, but many men who develop this infection have a normal immune system. | | ==Diagnosis== |
| | [[Prostatitis diagnostic study of choice|Diagnostic study of choice]] | [[Prostatitis history and symptoms| History and Symptoms]] | [[Prostatitis physical examination | Physical Examination]] | [[Prostatitis laboratory findings|Laboratory Findings]] | [[Prostatitis electrocardiogram|Electrocardiogram]] | [[Prostatitis x ray|X-Ray Findings]] | [[Prostatitis echocardiorgaphy and ultrasound|Echocardiography and Ultrasound]] | [[Prostatitis CT scan|CT-Scan Findings]] | [[Prostatitis MRI|MRI Findings]] | [[Prostatitis other imaging findings|Other Imaging Findings]] | [[Prostatitis other diagnostic studies|Other Diagnostic Studies]] |
|
| |
|
| ===Signs and symptoms=== | | ==Treatment== |
| *Pain between the scrotum & rectum.
| | [[Prostatitis medical therapy|Medical Therapy]] | [[Prostatitis surgery|Surgery]] | [[Prostatitis primary prevention|Primary Prevention]] | [[Prostatitis secondary prevention|Secondary Prevention]] | [[Prostatitis future or investigational therapies|Future or Investigational Therapies]] |
| *Frequent but low amount of urination (pollakiuria).
| |
| *The sensation of burning or pain during urination (dysuria), dribbling with urination
| |
| *Difficulty starting the urine stream or total inability to pass urine,
| |
| *Blood or pus in the urine.
| |
| *Sometimes accompanied by fever and chills and/or IBS symptoms, nausea and vomiting, muscle aches and fatigue or flu-like symptoms.
| |
| *The desire to urinate more at night.
| |
| *There may be discharge from the penis.
| |
| *Demonstrable infection of the urinary tract, as evidenced by white blood cells and bacteria in the urine.
| |
|
| |
|
| ===Diagnosis=== | | ==Case Studies== |
| Acute prostatitis is relatively easy to diagnose due to its symptoms that suggest infection. Common bacteria are ''[[Escherichia coli]], [[Klebsiella]], [[Proteus]], [[Pseudomonas]], [[Enterobacter]], [[Enterococcus]], [[Serratia]],'' and ''[[Staphylococcus aureus]].'' This can be a medical emergency in some patients and hospitalization with intravenous antibiotics may be required. A [[full blood count]] reveals increased white blood cells. [[Sepsis]] from prostatitis is very rare, but may occur in [[immunocompromised]] patients; high [[fever]] and malaise generally prompt [[blood culture]]s, which are often positive in sepsis. A prostate massage should never be done in a patient with suspected acute prostatitis, since it may induce sepsis. Since bacteria causing the prostatitis is easily recoverable from the urine, prostate massage is not required to make the diagnosis.
| | [[Prostatitis case study one|Case #1]] |
| | |
| ===Treatment of Acute Bacterial Prostatitis===
| |
| | |
| [[Antibiotics]] are the first line of treatment in acute prostatitis (Cat. I). Antibiotics usually resolve acute prostatitis infections in a very short time. Appropriate [[antibiotics]] should be used, based on the microbe causing the infection. Some antibiotics have very poor penetration of the prostatic capsule, others, such as [[Ciprofloxacin]], Co-trimoxazole and tetracyclines penetrate well. In acute prostatitis, penetration of the prostate is not as important as for category II because the intense inflammation disrupts the prostate-blood barrier. It is more important to choose a bacteriocidal antibiotic (kills bacteria, eg quinolone) rather than a bacteriostatic antibiotic (slows bacterial growth, eg. tetracycline) for acute potentially life threatening infections.<ref name="pmid15049589">{{cite journal |author=Hua VN, Schaeffer AJ |title=Acute and chronic prostatitis |journal=Med. Clin. North Am. |volume=88 |issue=2 |pages=483-94 |year=2004 |pmid=15049589 |doi=10.1016/S0025-7125(03)00169-X}}</ref> Severely ill patients may need hospitalization, while nontoxic patients can be treated at home with bed rest, analgesics, stool softeners, and hydration. Patients in urinary retention are best managed with a suprapubic catheter or intermittent catheterization. Lack of clinical response to antibiotics should raise the suspicion of an [[abscess]] and prompt an imaging study such as a transrectal ultrasound (TRUS).<ref name="pmid15380852">{{cite journal |author=Göğüş C, Ozden E, Karaboğa R, Yağci C |title=The value of transrectal ultrasound guided needle aspiration in treatment of prostatic abscess |journal=European journal of radiology |volume=52 |issue=1 |pages=94-8 |year=2004 |pmid=15380852 |doi=10.1016/S0720-048X(03)00231-6}}</ref>
| |
| | |
| ===Prognosis===
| |
| | |
| Full recovery without [[sequela]]e is usual.
| |
| | |
| ==Category II: Chronic bacterial prostatitis==
| |
| | |
| ===Signs and symptoms===
| |
| Chronic bacterial prostatitis is a relatively rare condition (<5% of patients with prostate-related non-BPH LUTS) that usually presents with an intermittent UTI-type picture and that is defined as recurrent urinary tract infections in men originating from a chronic infection in the prostate. Dr. Weidner, Professor of Medicine, Department of Urology, University of Giessen, has stated: "In studies of 656 men, we seldom found chronic bacterial prostatitis. It is truly a rare disease. Most of those were E-coli."<ref name="rare">{{cite journal | author=Schneider, H., Ludwig, M., Hossain, H. M., Diemer, T. & Weidner, W.| title=The 2001 Giessen Cohort Study on patients with prostatitis syndrome – an evaluation of inflammatory status and search for microorganisms 10 years after a first analysis| journal=Andrologia| year=2003| volume=35| issue=5| page=258-262| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=14535851&itool=pubmed_docsum}}</ref> Symptoms may be completely absent until there is also bladder infection, and the most troublesome problem is usually recurrent cystitis.<ref name="haber">{{cite journal | author=Habermacher GM, Chason JT, Schaeffer AJ.| title=Prostatitis/chronic pelvic pain syndrome| journal=Annu Rev Med.| year=2006| volume=57| page=195-206| url=http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=retrieve&db=pubmed&list_uids=16409145&dopt=citation}}</ref>
| |
| | |
| Main symptoms of chronic prostitis;
| |
| | |
| *Frequent urination with an accompanied burning sensation (dysuria).
| |
| *Blood or pus in the urine.
| |
| *Lower back pain.
| |
| *Premature ejaculation or loss of potency.
| |
| *The desire to urinate more at night (nocturia).
| |
| | |
| ===Diagnosis===
| |
| In chronic bacterial prostatitis there are bacteria in the prostate but usually no symptoms. The prostate infection is diagnosed by culturing urine as well as prostate fluid (expressed prostatic secretions or EPS) which are obtained by the doctor doing a rectal exam and putting pressure on the prostate. If no fluid is recovered after this prostatic massage, a post massage urine should also contain any prostatic bacteria. [[Prostate specific antigen]] levels may be elevated, although there is no malignancy.
| |
| | |
| ===Treatment of Chronic Bacterial Prostatitis===
| |
| | |
| Treatment requires prolonged courses (4-8 weeks) of antibiotics that penetrate the prostate well ([[beta-lactam|β-lactam]]s and [[nitrofurantoin]] are ineffective). These include [[quinolone]]s (ciprofloxacin, [[levofloxacin]]), [[Sulfonamide (medicine)|sulfas]] ([[trimethoprim-sulfamethoxazole|Bactrim, Septra]]) and [[macrolide]]s ([[erythromycin]], [[clarithromycin]]). Persistent infections may be helped in 80% of patients by the use of [[alpha blocker]]s ([[tamsulosin]] (Flomax), [[alfuzosin]]), or long term low dose antibiotic therapy.<ref>{{cite journal |author=Shoskes D, Hakim L, Ghoniem G, Jackson C |title=Long-term results of multimodal therapy for chronic prostatitis/chronic pelvic pain syndrome |journal=J Urol |volume=169 |issue=4 |pages=1406-10 |year=2003 |id=PMID 12629373}}</ref> Recurrent infections may be caused by inefficient urination (benign prostatic hypertrophy, neurogenic bladder), prostatic stones or a structural abnormality that acts as a reservoir for infection.
| |
| | |
| The addition of [[prostate massage]] to courses of antibiotics was previously proposed as being beneficial.<ref>{{cite journal |author=Nickel J, Downey J, Feliciano A, Hennenfent B |title=Repetitive prostatic massage therapy for chronic refractory prostatitis: the Philippine experience |journal=Tech Urol |volume=5 |issue=3 |pages=146-51 |year=1999 |id=PMID 10527258}}</ref><ref>{{cite journal |author= |title=Use of prostatic massage in combination with antibiotics in the treatment of chronic prostatitis |journal=Prostate Cancer Prostatic Dis |volume=2 |issue=3 |pages=159-162 |year=1999 |id=PMID 12496826}}</ref>
| |
| It is though not without some risk,<ref name="massage9">{{cite journal | author=Buse S, Warzinek T, Hobi C, Ackerman D.| title=Prostate massage with unwanted consequences. Case report| journal=Urologe A. | year=2003| volume=42| issue=1| page=78-79| url=http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=retrieve&db=pubmed&list_uids=14655640&dopt=citation}}</ref><ref>{{cite journal |author=Sengoku A, Yamashita M, Umezu K |title=[A case of Fournier's gangrene: was it triggered by prostatic massage?] |journal=Hinyokika Kiyo |volume=36 |issue=9 |pages=1097-100 |year=1990 |id=PMID 2239620}}</ref> and, in more recent trials, was not shown to improve outcome compared to antibiotics alone.<ref>{{cite journal |author=Ateya A, Fayez A, Hani R, Zohdy W, Gabbar M, Shamloul R |title=Evaluation of prostatic massage in treatment of chronic prostatitis |journal=Urology |volume=67 |issue=4 |pages=674-8 |year=2006 |id=PMID 16566972}}</ref>
| |
| | |
| ===Prognosis===
| |
| Over time, the relapse rate is high, exceeding 50%. A 2007 study showed that repeated courses of combination antibiotics may eradicate infection in 83.9% of patents with clinical remission extending throughout a follow-up period of 30 months for 94% of these patients.<ref name="ital">{{cite journal | author=Magri V et al| title=Efficacy of repeated cycles of combination therapy for the eradication of infecting organisms in chronic bacterial prostatitis.| journal=Int J Antimicrob Agents| year=2007 May| volume=29| issue=5| page=549-556| url=http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=retrieve&db=pubmed&list_uids=17336504 &dopt=citation}}</ref>
| |
| | |
| ==Category III: CP/CPPS==
| |
| | |
| ===Signs and symptoms===
| |
| | |
| In chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) there is pelvic pain of unknown cause, lasting longer than 3 months,<ref name="luzzi">{{cite journal | author=Luzzi, GA.| title=Chronic prostatitis and chronic pelvic pain in men: aetiology, diagnosis and management.| journal=J Eur Acad Dermatol Venereol.| year=2002| volume=16| issue=3| page=253-256| url=http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=retrieve&db=pubmed&list_uids=12195565&dopt=citation}}</ref> as the key symptom. Symptoms may wax and wane. Pain can range from mild discomfort to debilitating. Pain may radiate to back and rectum, making sitting difficult. [[Dysuria]], [[arthralgia]], [[myalgia]], unexplained [[fatigue (medical)|fatigue]], abdominal pain, constant burning pain in the penis, and frequency may all be present. Frequent urination and increased urgency may suggest [[Interstitial cystitis|interstitial cystitis]] (inflammation centred in bladder rather than prostate). [[Ejaculation]] may be painful, as the prostate contracts during emission of semen, although nerve- and muscle-mediated post-ejaculatory pain is more common, and a classic sign of [[CP/CPPS]]. Some patients report low libido, [[Sexual dysfunction|sexual dysfunction]] and [[Impotence|erectile difficulties]]. Pain after [[ejaculation]] is a very specific complaint that distinguishes CP/CPPS from men with [[Benign prostatic hyperplasia|BPH]] or normal men.
| |
| | |
| ===Theories of etiology===
| |
| | |
| Theories behind the disease include [[autoimmunity]], for which there is scant evidence, [[neurogenic inflammation]] and [[Myofascial_Pain_Syndrome|myofascial pain syndrome]]. In the latter two categories, dysregulation of the local nervous system due to past trauma, infection or an anxious disposition and chronic albeit unconscious pelvic tensing lead to inflammation that is mediated by substances released by nerve cells (such as [[substance P]]). The prostate (and other areas of the genitourinary tract: bladder, urethra, testicles) can become inflamed by the action of the chronically activated pelvic nerves on the mast cells at the end of the nerve pathways. Similar stress-induced genitourinary inflammation has been shown experimentally in other mammals.<ref name=TC>{{cite journal |author=Alexacos N, Pang X, Boucher W, Cochrane DE, Sant GR, Theoharides TC |title=Neurotensin mediates rat bladder mast cell degranulation triggered by acute psychological stress |journal=Urology |volume=53 |issue=5 |pages=1035–40 |year=1999 |pmid=10223502 |doi=}}</ref> However, there is no correlation between inflammation on histological examination of the prostate and the [[National Institutes of Health]] Chronic Prostatitis Symptom Index.<ref name="pmid17632164">{{cite journal |author=Nickel JC, Roehrborn CG, O'leary MP, Bostwick DG, Somerville MC, Rittmaster RS |title=Examination of the relationship between symptoms of prostatitis and histological inflammation: baseline data from the REDUCE chemoprevention trial |journal=J. Urol. |volume=178 |issue=3 Pt 1 |pages=896–900; discussion 900–1 |year=2007 |pmid=17632164 |doi=10.1016/j.juro.2007.05.041}}</ref>
| |
| | |
| The bacterial infection theory that for so long had held sway in this field was shown to be unimportant in a 2003 study from the [[University of Washington]] team led by Dr Lee and Professor Richard Berger. The study found that one third of both normal men and patients had equal counts of similar bacteria colonizing their prostates.<ref name=BG>{{cite journal |author=Lee JC, Muller CH, Rothman I, ''et al'' |title=Prostate biopsy culture findings of men with chronic pelvic pain syndrome do not differ from those of healthy controls |journal=J. Urol. |volume=169 |issue=2 |pages=584–7; discussion 587–8 |year=2003 |pmid=12544312 |doi=10.1097/01.ju.0000045673.02542.7a}}</ref> This view was endorsed by Dr Anthony Schaeffer, Professor and Chairman of the Department of Urology at [[Feinberg School of Medicine]], in a 2003 editorial of ''The Journal of Urology'', in which he stated that ''"...these data suggest that bacteria do not have a significant role in the development of the chronic pelvic pain syndrome"'',<ref name="comment">{{cite journal | author=Schaeffer AJ| title=Editorial: Emerging concepts in the management of prostatitis/chronic pelvic pain syndrome.| journal=J Urol.| year=2003| volume=169| issue=2| page=597-598| pmid=12544315}}</ref> and a year later with his colleagues he published studies showing that antibiotics are essentially useless for CP/CPPS.<ref name=BC1>{{cite journal |author=Alexander RB, Propert KJ, Schaeffer AJ, ''et al'' |title=Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial |journal=Ann. Intern. Med. |volume=141 |issue=8 |pages=581–9 |year=2004 |pmid=15492337 |doi=}}</ref><ref name=BC2>{{cite journal |author=Nickel JC, Downey J, Clark J, ''et al'' |title=Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial |journal=Urology |volume=62 |issue=4 |pages=614–7 |year=2003 |pmid=14550427 |doi=}}</ref> Since the publication of these studies, the focus has shifted from infection to neuromuscular and psychological etiologies for chronic prostatitis (CP/CPPS); a 2005 study showed that [[Stress (medicine)|stress]] is correlated to Cat III prostatitis.<ref name="pmid16173907">{{cite journal |author=Ullrich PM, Turner JA, Ciol M, Berger R |title=Stress is associated with subsequent pain and disability among men with nonbacterial prostatitis/pelvic pain |journal=Annals of behavioral medicine : a publication of the Society of Behavioral Medicine |volume=30 |issue=2 |pages=112–8 |year=2005 |pmid=16173907 |doi=10.1207/s15324796abm3002_3}}</ref>
| |
| | |
| Additional theories and observations include:
| |
| | |
| ====Possible role of unculturable bacteria in CPPS====
| |
| | |
| A 2007 Croatian study, without controls, suggested that "prostatitis syndrome"[''sic''] patients may be infected with a wide variety of microbes. The study used McCoy culture and [[Lugol's_iodine|Lugol stain]] or by [[Immunofluorescence|immunofluorescent]] typing with monoclonal antibodies to come to these findings.<ref name="PMID17868538">{{cite journal |author=Skerk V, Krhen I, Cajić V, Markovinović L, Puntarić A, Roglić S, Zekan S, Ljubin-Sternak S, Zidovec Lepej S, Vince A. |title=The Role of Chlamydia trachomatis in Prostatitis Syndrome - Our Experience in Diagnosis and Treatment. |journal=Acta Dermatovenerol Croat. |volume=3 |pages=135-140; |year=2007 |pmid=17868538}}</ref> If this study refers to men with Chronic Pelvic Pain Syndrome, it is not in line with major studies from other centres.<ref name=BG /><ref name=JC />
| |
| | |
| ====CPPS as a form of interstitial cystitis====
| |
| | |
| Some researchers have suggested that CPPS is a form of [[interstitial cystitis]]. A large multicenter prospective randomized controlled study showed that Elmiron was slightly better than placebo in treating the symptoms of CPPS, however the primary endpoint did not reach statistical significance.<ref name="elmiron">{{cite journal |author=Nickel JC, Forrest JB, Tomera K, ''et al'' |title=Pentosan polysulfate sodium therapy for men with chronic pelvic pain syndrome: a multicenter, randomized, placebo controlled study |journal=J. Urol. |volume=173 |issue=4 |pages=1252–5 |year=2005 |pmid=15758763 |doi=10.1097/01.ju.0000159198.83103.01}}</ref> Other therapies shown more effective than Elmiron in treating interstitial cystitis, such as [[quercetin]] and Elavil ([[amitriptyline]]), can help with chronic prostatitis.
| |
| | |
| ====Effect of cold exposure====
| |
| | |
| Studies in 2007 showed that CPPS is associated with cold weather and exposure to cold.<ref name="pmid17853027">{{cite journal |author=Hedelin H, Jonsson K |title=Chronic prostatitis/chronic pelvic pain syndrome: Symptoms are aggravated by cold and become less distressing with age and time |journal= |volume= |issue= |pages=1–5 |year=2007 |pmid=17853027 |doi=10.1080/00365590701428517}}</ref><ref name="pmid17853032">{{cite journal |author=Hedelin H, Jonsson K |title=Chronic abacterial prostatitis and cold exposure |journal= |volume= |issue= |pages=1–6 |year=2007 |pmid=17853032 |doi=10.1080/00365590701365123}}</ref>
| |
| | |
| ===Diagnosis===
| |
| | |
| There are no definitive diagnostic tests for CP/CPPS. This is a poorly understood disorder, even though it accounts for 90%-95% of prostatitis diagnoses.<ref name="t1">{{cite journal | author=Habermacher GM, Chason JT, Schaeffer AJ.| title=Prostatitis/chronic pelvic pain syndrome.| journal=Annu Rev Med.| year=2006| volume=57| page=195-206| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=16409145&itool=pubmed_docsum}}</ref> It is found in men of any age, with the peak onset in the early 30s. CP/CPPS may be inflammatory (category IIIa) or non-inflammatory (category IIIb). In the inflammatory form, urine, semen, and other fluids from the prostate contain pus cells (dead white blood cells or WBCs), whereas in the non-inflammatory form no pus cells are present. Recent studies have questioned the distinction between categories IIIa and IIIb, since both categories show evidence of inflammation if pus cells are ignored and other more subtle signs of inflammation, like [[cytokines]], are measured. In 2006, Chinese researchers found that men with categories IIIa and IIIb both had significantly and similarly raised levels of anti-inflammatory cytokine TGFß1 and pro-inflammatory cytokine [[interferon-gamma|IFN-γ]] in their expressed prostatic secretions when compared with controls; therefore measurement of these cytokines could be used to diagnose category III prostatitis.<ref name="tgf">{{cite journal | author=Ding XG, Li SW, Zheng XM, Hu LQ.| title=[IFN-gamma and TGF-beta1, levels in the expressed prostatic secretions of patients with chronic abacterial prostatitis]| journal=Zhonghua Nan Ke Xue.| year=2006| volume=12| issue=11| page=982-984| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=17146921&itool=pubmed_docsum}}</ref>
| |
| | |
| Normal men have slightly more bacteria in their semen than men with CPPS.<ref name=JC>[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=12913707&itool=pubmed_docsum Leukocytes and bacteria in men with chronic prostatitis/chronic pelvic pain syndrome compared to asymptomatic controls] ''J Urol. 2003 Sep;170(3):818-22'' (Nickel JC, Alexander RB, Schaeffer AJ)</ref> The traditional Stamey 4-glass test is invalid for diagnosis of this disorder, and inflammation cannot be localized to any particular area of the lower GU tract.<ref name=JC />
| |
| | |
| Men with CP/CPPS are more likely than the general population to suffer from [[Chronic Fatigue Syndrome]] (CFS),<ref name="cfs">{{cite journal | author=Leslie A Aaron et al| title=Comorbid Clinical Conditions in Chronic Fatigue, A Co-Twin Control Study| journal=J Gen Intern Med.| year=2001| volume=16| issue=1| page=24-31| url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&rendertype=abstract&artid=1495162}}</ref> and [[Irritable bowel syndrome|Irritable Bowel Syndrome]] (IBS). [[Prostate specific antigen]] levels may be elevated, although there is no malignancy.
| |
| | |
| Experimental tests that could be useful in the future include tests to measure semen and prostate fluid cytokine levels. Various studies have shown increases in markers for inflammation such as elevated levels of cytokines, myeloperoxidase, and chemokines.
| |
| | |
| ===Treatment of Chronic Prostatitis / Chronic Pelvic Pain Syndrome===
| |
| | |
| A 2007 review article by Drs Potts and Payne in the ''[[Cleveland Clinic]] Journal of Medicine'' states:<ref name="potts2007">{{cite journal | author=Potts J, Payne RE| title=Prostatitis: Infection, neuromuscular disorder, or pain syndrome? Proper patient classification is key.| journal=Cleve Clin J Med| year=2007 May| volume=74| issue=Suppl 3| page=S63-71| url=http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=retrieve&db=pubmed&list_uids=17549825&dopt=citation}}</ref><blockquote>''"Indeed, chronic abacterial prostatitis (also known as chronic pelvic pain syndrome) is both the most prevalent form and also the least understood and the most challenging to evaluate and treat. This form of prostatitis may respond to non-prostate-centered treatment strategies such as physical therapy, myofascial trigger point release, and relaxation techniques."''</blockquote>
| |
| ====Physical and psychological therapy====
| |
| For chronic nonbacterial prostatitis (Cat III), also known as [[CP/CPPS]], which makes up the majority of men diagnosed with "prostatitis", a treatment called the '''Stanford Protocol''',<ref name="spcpcom">{{Cite web|url=http://www.chronicprostatitis.com/spasmtx.html|title=The Stanford Protocol|accessdate=2006-12-09|year=2005|format=html}}</ref> developed by [[Stanford University School of Medicine]] Professor of Urology Rodney Anderson and psychologist David Wise in 1996, has recently been published. This is a combination of medication (using tricyclic [[antidepressant]]s and [[benzodiazepine]]s), psychological therapy (paradoxical relaxation, an advancement and adaptation, specifically for pelvic pain, of a type of progressive relaxation technique developed by [[Edmund Jacobson]] during the early 20th century), and physical therapy ([[Trigger point|trigger point]] release therapy on [[pelvic floor]] and abdominal muscles, and also yoga-type exercises with the aim of relaxing pelvic floor and abdominal muscles). <ref name=SP>[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=15947608&itool=pubmed_docsum Trigger Points and Relaxation in the Treatment of Prostatitis] ''J Urol. 2005 Jul;174(1):155-60'' (Anderson RU, Wise D, Sawyer T, Chan C.)</ref> <ref name=SP1>[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=16952676&itool=pubmed_docsum Sexual Dysfunction in Men With Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Improvement After Trigger Point Release and Paradoxical Relaxation Training] ''J Urol. 2006 Oct;176(4 Pt 1):1534-8; discussion 1538-9'' (Anderson RU, Wise D, Sawyer T, Chan C.)</ref> While these studies are encouraging, definitive proof of efficacy would require a randomized, sham controlled, blinded study, which is not as easy to do with physical therapy as with drug therapy.
| |
| | |
| Cat. III prostatitis may have no initial trigger other than anxiety, often with an element of [[Obsessive Compulsive Disorder]] or other anxiety-spectrum problem. This is theorized to leave the pelvic area in a sensitized condition resulting in a loop of muscle tension and heightened neurological feedback (neural wind-up). Current protocols largely focus on stretches to release overtensed muscles in the pelvic or anal area (commonly referred to as [[trigger points]]), physical therapy to the area, and progressive relaxation therapy to reduce causative stress. [[Biofeedback]] physical therapy to relearn how to control pelvic floor muscles may be useful.<ref name="biofeed">{{cite journal | author=Cornel EB et al| title=The effect of biofeedback physical therapy in men with Chronic Pelvic Pain Syndrome Type III.| journal=Eur Urol.| year=2005| volume=47| issue=5| page=607-11| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=15826751&itool=pubmed_docsum}}</ref>
| |
| | |
| Aerobic exercise can help those sufferers who are not also suffering from [[Chronic fatigue syndrome|Chronic Fatigue Syndrome (CFS)]] or whose symptoms are not exacerbated by exercise.<ref name="exerc">{{cite journal | author=Giubilei G, Mondaini N, Minervini A, Saieva C, Lapini A, Serni S, Bartoletti R, Carini M.| title=Physical Activity of Men With Chronic Prostatitis/Chronic Pelvic Pain Syndrome Not Satisfied With Conventional Treatments-Could it Represent a Valid Option? The Physical Activity and Male Pelvic Pain Trial: A Double-Blind, Randomized Study.| journal=J Urol.| year=2007| volume=177| issue=1| page=159-65| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=17162029&itool=pubmed_docsum}}</ref>
| |
| | |
| ====Food allergies====
| |
| Anecdotal evidence suggests that food allergies and intolerances may have a role in exacerbating [[CP/CPPS]], perhaps through mast cell mediated mechanisms. Specifically patients with [[gluten]] intolerance or [[celiac disease]] report severe symptom flares after sustained gluten ingestion. Patients may therefore find an exclusion diet helpful in lessening symptoms by identifying problem foods. Studies are lacking in this area.
| |
| | |
| ====Pharmacological treatment====
| |
| There is a substantial list of medications used to treat this disorder.<ref name="cpcom">{{Cite web|url=http://www.chronicprostatitis.com/meds.html|title=Pharmacological treatment options for prostatitis/chronic pelvic pain syndrome|accessdate=2006-12-11|year=2006|format=html}}</ref>
| |
| | |
| * Alpha blockers ([[tamsulosin]], [[alfuzosin]]) are moderately helpful for many men with CPPS;<ref name="alpha">"...tamsulosin did not substantially reduce symptoms in men with long-standing CP/CPPS who had at least moderate symptoms." {{cite journal | author=Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O'Leary MP, Pontari MA, McNaughton-Collins M, Shoskes DA, Comiter CV, Datta NS, Fowler JE Jr, Nadler RB, Zeitlin SI, Knauss JS, Wang Y, Kusek JW, Nyberg LM Jr, Litwin MS; Chronic Prostatitis Collaborative Research Network.| title=Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial.| journal=Ann Intern Med.| year=2004| volume=141| issue=8| page=581-9| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?itool=abstractplus&db=pubmed&cmd=Retrieve&dopt=abstractplus&list_uids=15492337}}</ref> duration of therapy needs to be at least 3 months.<ref name="alpha3">"...treatment duration should be long enough (more than 3 months)"{{cite journal | author=Yang G et al| title=The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials.| journal=J Androl.| year=2006| volume=27| issue=6| page=847-52| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=16870951&itool=pubmed_docsum}}</ref>
| |
| * [[Quercetin]] has shown effective in a randomized, placebo-controlled trial in chronic prostatitis using 500 mg twice a day for 4 weeks.<ref name="shoskes">{{cite journal | author=Shoskes, DA et al| title=Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial.| journal=Urology.| year=1999| volume=54| issue=6| page=960-3| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=10604689&itool=pubmed_docsum}}</ref> Subsequent studies showed that quercetin, a mast cell inhibitor, reduces inflammation and oxidative stress in the prostate.
| |
| * Pollen extract (Cernilton) has also been shown effective in randomized placebo controlled trials.<ref name="bee">{{cite journal | author=Suzuki T, et al| title=[Clinical effect of Cernilton in chronic prostatitis]| journal=Hinyokika Kiyo.| year=1992| volume=38| issue=4| page=489-94| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=1529825&opt=Abstract}}</ref><ref name="bee2">{{cite journal | author=Yan, H et al| title=[Efficacy of Prostat in the treatment of NIH category IIIA prostatitis]| journal= Zhonghua Nan Ke Xue. | year=2004| volume=10| issue=12| page=930-1| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=15638027&itool=pubmed_docsum}}</ref><ref name="bee3">{{cite journal | author=Elist J| title=Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study.| journal=Urology| year=2006| volume=67| issue=1| page=60-3| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=16413333&itool=pubmed_docsum}}</ref>
| |
| * Commonly used therapies that have not been properly evaluated in clinical trials are dietary modification, gabapentin, and amitriptyline.
| |
| * Therapies shown to be ''ineffective'' by randomized placebo/sham controlled trials: [[levaquin]] ([[antibiotics]]), alpha blockers for 6 weeks or less, transurethral needle ablation of the prostate ([[TUNA]]).
| |
| * At least one study suggests that multi-modal therapy (aimed at different pathways such as inflammation and neuromuscular dysfunction simultaneously) is better long term than monotherapy.<ref name="potts">{{cite journal | author=Potts JM| title=Therapeutic options for chronic prostatitis/chronic pelvic pain syndrome.| journal=Curr Urol Rep.| year=2005| volume=6| issue=4| page=313-7| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=15978236&itool=pubmed_docsum}}</ref>
| |
| | |
| ===Prognosis===
| |
| In recent years the prognosis for CP/CPPS has improved greatly with the advent of multimodal treatment, phytotherapy and protocols aimed at quieting the pelvic nerves through myofascial trigger point release and anxiety control.
| |
| | |
| ==Category IV: Asymptomatic inflammatory prostatitis==
| |
| | |
| ===Signs and symptoms===
| |
| These patients have no history of genitourinary pain complaints, but [[Leucocyte|leukocytosis]] or bacteria have been noted during evaluation for other conditions.
| |
| | |
| ===Diagnosis===
| |
| Diagnosis is through tests of semen, EPS or prostate tissue that reveal inflammation in the absence of symptoms.<ref name="pmid16280832">{{cite journal |author=Clemens JQ, Meenan RT, O'Keeffe Rosetti MC, Gao SY, Calhoun EA |title=Incidence and clinical characteristics of National Institutes of Health type III prostatitis in the community |journal=J. Urol. |volume=174 |issue=6 |pages=2319-22 |year=2005 |pmid=16280832 |doi=10.1097/01.ju.0000182152.28519.e7}}</ref>
| |
| | |
| ===Treatment of Asymptomatic Inflammatory Prostatitis===
| |
| | |
| No treatment required. It is standard practice for men with infertility and category IV prostatitis to be given a trial of antibiotics and/or anti-inflammatories however evidence for efficacy are weak.<ref name="weidner">"Several inflammatory and reactive alterations of sperm quality seem to be proven; nevertheless, the impact of these findings on male fertility remains in many cases unclear."{{cite journal | author=Weidner W, et al| title=Relevance of male accessory gland infection for subsequent fertility with special focus on prostatitis.| journal=Hum Reprod Update.| year=1999| volume=5| issue=5| page=421-32| url=http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=pubmed&cmd=Retrieve&dopt=AbstractPlus&list_uids=10582781&itool=pubmed_docsum}}</ref> Since signs of asymptomatic prostatic inflammation may sometimes be associated with [[prostate cancer]], this can be addressed by tests that assess the ratio of free-to-total PSA. The results of these tests were significantly different in prostate cancer and category IV prostatitis in one study.<ref>"The ratio of free-to-total PSA is significantly different in PCa and NIH category IV prostatitis." [http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=15548444&dopt=Abstract Effect of NIH-IV prostatitis on free and free-to-total PSA] '' Eur Urol. 2004 Dec;46(6):760-4.'' (Stancik I et al)</ref>
| |
|
| |
|
| ==References== | | ==References== |
| {{Reflist|2}} | | {{reflist}} |
|
| |
|
| ==See also==
| | [[Category:Medicine]] |
| | | [[Category:Infectious disease]] |
| *[[Quercetin]] — a [[flavonoid]] which has [[anti-inflammatory]] and [[mast cell]] protective properties
| | [[Category:Nephrology]] |
| *[[Trigger_point|Trigger Points]]
| |
| *[[Interstitial cystitis]] — men with IC may have prostatitis, and vice versa.
| |
| | |
| == External links ==
| |
| | |
| * [http://www.mayoclinic.com/health/prostatitis/DS00341 Mayo Clinic] - prostatitis at the Mayo Clinic.
| |
| | |
| {{Diseases of the pelvis, genitals and breasts}}
| |
| | |
| [[Category:Inflammations]] | |
| [[Category:Urology]] | | [[Category:Urology]] |
| [[Category:Andrology]] | | [[Category:Up-To-Date]] |
| [[Category:Infectious disease]] | | [[Category:Emergency medicine]] |
| [[Category:Disease state]]
| |
| [[Category:Needs patient information]]
| |
| | |
| {{SIB}}
| |
| | |
| [[de:Prostatitis]]
| |
| [[es:Prostatitis]]
| |
| [[fr:Prostatite]]
| |
| [[it:Prostatite]]
| |
| [[nl:Prostatitis]]
| |
| [[pt:Prostatite]]
| |
| [[ru:Простатит]]
| |
| [[fi:Eturauhasen tulehdus]]
| |
| [[zh:前列腺炎]]
| |
| | |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |