Postpartum hemorrhage
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Adnan Ezici, M.D[2]
Synonyms and keywords:
Overview
Postpartum hemorrhage is classified according to the duration between the delivery and hemorrhage into 2 groups: primary (within the first 24 hours after birth) and secondary (between 24 hours and 12 weeks after birth). The pathophysiology of postpartum hemorrhage depends on the underlying etiology. It is important to differentiate the underlying etiology of postpartum hemorrhage for deciding the treatment. The most common cause of postpartum hemorrhage is uterine atony. Less common causes of postpartum hemorrhage include obstetrical lacerations, retained placental tissue, and maternal coagulation disorders. The incidence of postpartum hemorrhage (the leading cause of maternal deaths) is approximately 4,000-6,000 per 100,000 individuals with a case-fatality rate of 7.5%. Common risk factors in the development of postpartum hemorrhage include the prolonged third stage of labor, preeclampsia, Asian race, and previous postpartum hemorrhage. Risk factors in the development of postpartum hemorrhage further differentiate depending on the cause. The diagnosis of postpartum hemorrhage is based on the amount of blood loss and clinical presentation of the patient, which include either blood loss ≥1000 mL (regardless of the form of the delivery) or the presence of tachycardia and hypotension in a patient with blood loss. Postpartum hemorrhage is traditionally described as blood loss > 500 mL after a vaginal delivery or blood loss > 1000 mL after a cesarean delivery. Physical examination may provide the underlying etiology of postpartum hemorrhage such as the presence of a soft, large and boggy uterus which indicates uterine atony. Laboratory values that should be obtained on admission to delivery include complete blood count, basic metabolic panel, blood type/screening, fibrinogen, PT, and aPTT. Ultrasound may be helpful in the diagnosis of the underlying etiology of postpartum hemorrhage. IV catheter placement, foley catheter placement, bimanual uterine massage, manual exploration of the uterine cavity with the evacuation of retained placental tissue or blood clots, and intravenous fluid therapy are recommended among all patients who develop postpartum hemorrhage. If present, genital tract lacerations should immediately be repaired with absorbable sutures. Pharmacologic medical therapies for postpartum hemorrhage include either oxytocin (first-line), methylergonovine, carboprost, or misoprostol. Placement of an arterial catheter, placement of a central venous catheter, placement of a uterine balloon tamponade, tranexamic acid administration, and blood transfusion should additionally be considered in patients with estimated blood loss ≥1500-3000 mL. Embolization of the uterine artery should be considered among hemodynamically stable patients resistant to medical treatment. Surgery is not the first-line treatment option for patients with postpartum hemorrhage. Surgery is usually reserved for patients either with bleeding resistant to the less invasive measures, estimated blood loss ≥ 3000 mL, or hemodynamic instability. As a method of primary prevention, the active management of the third stage of labor (AMTSL) compared to the physiological (expectant) management reduces the risk of postpartum hemorrhage.
Historical Perspective
- In 1953, du Vigneaud et al. and Tuppy were the first to discover the aminoacid sequence of oxytocin and its biochemical synthesis.[1]
- In 1962, the use of prophylactic uterotonic agent, early cord clamping, and controlled cord traction were defined by Spencer for the active management of the third stage of labor (AMTSL).[2]
- The reduction of postpartum hemorrhage by the active management of the third stage of labor (AMTSL) compared to the physiological (expectant) management was established by Prendiville et al. in 1988 following a randomized controlled trial.[3]
- In 1997, the B-Lynch surgical technique was developed by B-Lynch et al. to treat postpartum hemorrhage.[4]
- In 2005, first placebo-controlled study of misoprostol was conducted by Derman et al. for the prevention of postpartum hemorrhage.[5]
- In 2007, the use of misoprostol in the absence of oxytocin was recommended by World Health Organization (WHO) for the prevention of postpartum hemorrhage.[1]
Classification
Postpartum hemorrhage is classified according to the duration between the delivery and hemorrhage into 2 groups: primary and secondary.[6]
- If the postpartum hemorrhage begins within the first 24 hours after birth, it is classified as primary postpartum hemorrhage.
- If the postpartum hemorrhage occurs between 24 hours and 12 weeks after birth, it is classified as secondary postpartum hemorrhage.
Pathophysiology
The pathophysiology of postpartum hemorrhage depends on the underlying etiology:
- Inadequate contractions following the delivery (uterine atony)[7]
- Trauma in either vulva, vagina, or cervix during the delivery (obstetrical lacerations)[8]
- Placenta accreta, increta, percreta, or incomplete delivery of placenta (retained placental tissue)[6]
- Massive activation of the coagulation system and subsequent consumption of the coagulation factors (disseminated intravascular coagulation), platelet disorders (thrombocytopenia caused by preeclampsia, HELLP syndrome, ITP, TTP, acute fatty liver of pregnancy and HUS, and also qualitative platelet disorders), von Willebrand disease (vWD), hemophilia A, and hemophilia B (maternal coagulation disorders) [9]
Causes
The most common cause of postpartum hemorrhage is uterine atony. Less common causes of postpartum hemorrhage include obstetrical lacerations, retained placental tissue, and maternal coagulation disorders.[6]
- The 4 T's (tone, trauma, tissue, and thrombin) can be used for summarizing the causes of postpartum hemorrhage.
Differential Diagnosis
It is important to differentiate the underlying etiology of postpartum hemorrhage for deciding the treatment.
- A detailed physical examination is crucial to detect the anatomical source (uterine, cervical, vaginal, perineal, etc.) of the bleeding.[10]
- The duration between the delivery and hemorrhage should be considered to decide whether the postpartum hemorrhage is primary or secondary.[10]
- Primary postpartum hemorrhage may be caused by uterine atony, obstetrical lacerations, retained placental tissue, placenta accreta spectrum (lacenta accreta, increta, and percreta), uterine inversion, inherited coagulation defects, and disseminated intravascular coagulation (DIC)
- Secondary postpartum hemorrhage may be caused by infection, retained products of conception (RPOC), subinvolution of placental sites (SPSs), and inherited coagulation defects (e.g., von Willebrand disease).
Epidemiology and Demographics
- The incidence of postpartum hemorrhage is approximately 4,000-6,000 per 100,000 individuals with a case-fatality rate of 7.5%.[11][12]
- Individuals living in rural areas are more likely to face postpartum hemorrhage than individuals living in urban areas.[11]
- Postpartum hemorrhage commonly affects individuals 15-54 years of age.[13]
- Approximately 25% of maternal deaths are due to postpartum hemorrhage, which is the leading cause of maternal deaths.[14]
- Postpartum hemorrhage usually results in death in individuals of the non-Hispanic black race. Non-Hispanic white individuals are less likely to die due to postpartum hemorrhage.[13]
Risk Factors
Common risk factors in the development of postpartum hemorrhage include the prolonged third stage of labor, preeclampsia, Asian race, and previous postpartum hemorrhage. Risk factors in the development of postpartum hemorrhage further differentiate depending on the cause.[11]
- Common risk factors in the development of uterine atony include uterine overdistention (e.g., polyhydramnios, multiple pregnancy, fetal macrosomia), prolonged labor, prolonged use of oxytocin, chorioamnionitis, and the application of inhaled anesthetic agents.
- Common risk factors in the development of obstetrical lacerations include episiotomy, cesarean delivery, assisted delivery, genital tract lacerations, and uterine rupture.
- Common risk factors in the development of disseminated intravascular coagulation include placental abruption, amniotic fluid embolism, intrauterine fetal demise, and sepsis.
Screening
There is insufficient evidence to recommend routine screening for postpartum hemorrhage.
Natural History, Complications, and Prognosis
- Common early complications of postpartum hemorrhage include hypovolemic shock, disseminated intravascular coagulation (DIC), hepatic failure, acute renal failure, transfusion-related acute lung injury (TRALI), transfusion-associated volume overload, acute respiratory distress syndrome (ARDS), and death.[6]
- Common late complications of postpartum hemorrhage include Sheehan syndrome and infertility.
Diagnosis
Diagnostic Study of Choice
The diagnosis of postpartum hemorrhage is based on the amount of blood loss and clinical presentation of the patient, which include either blood loss ≥1000 mL (regardless of the form of the delivery) or the presence of tachycardia and hypotension in a patient with blood loss.[6]
- Blood loss could be measured by two different methods include visual and quantitative.
- Although quantitative method is better for the accuracy of the blood loss, there is no significant difference between these methods for the clinical outcomes.
- Postpartum hemorrhage is traditionally described as blood loss > 500 mL after a vaginal delivery or blood loss > 1000 mL after a cesarean delivery.
- Obstetric shock index (heart rate divided by systolic blood pressure) might be helpful to establish the severity of bleeding and the requirement of blood transfusion. [15][16]
- In a patient with obstetric shock index > 1, blood transfusion and further resuscitation attempts should be considered.
History and Symptoms
The hallmark of postpartum hemorrhage is hypovolemia. Common symptoms of postpartum hemorrhage include:[17]
These symptoms indicate the loss of approximately 25% of the total blood volume, therefore, it is important to detect the blood loss before these symptoms of hypovolemia appear.[10]
Physical Examination
Physical examination may provide the underlying etiology of postpartum hemorrhage.[10]
- The presence of a soft, large and boggy uterus on physical examination is highly suggestive of uterine atony.[18]
- Inspection of the lower genital tract is crucial for the identification of cervical, vaginal, perineal, or rectovaginal lacerations.[6]
- Following the delivery of the placenta, an inspection of the placenta should be carefully done. An incomplete placenta on inspection is highly suggestive of retained placental tissue. However, a complete placenta on inspection does not exclude the retained placental tissue due to the probability of retained succenturiate lobe of the placenta within the uterine cavity.[10]
Laboratory Findings
Laboratory values that should be obtained on admission to delivery include complete blood count, basic metabolic panel, blood type/cross-matching, fibrinogen, PT, and aPTT.[6]
- Laboratory findings consistent with the diagnosis of postpartum hemorrhage include a decreased concentration of hemoglobin and hematocrit. However, it may not be useful in clinical settings because of the relatively late reflection of rapid blood loss. Thus, the management of postpartum hemorrhage should be started without waiting for the decreased concentration of hemoglobin and hematocrit.[19]
Electrocardiogram
An ECG may be helpful in the detection of myocardial infarction, which might occur during severe postpartum hemorrhage. Findings on an ECG suggestive of myocardial infarction include T wave inversion, ST-segment elevation, and Q waves.[20]
X-ray
There are no x-ray findings associated with postpartum hemorrhage.
Ultrasound
Ultrasound may be helpful in the diagnosis of the underlying etiology of postpartum hemorrhage.[21]
- Findings on ultrasound suggestive of retained placenta include echogenic mass in the uterine cavity, the diameter of the uterine cavity >90 percentile, and endometrial vascularity (on Doppler sonography).
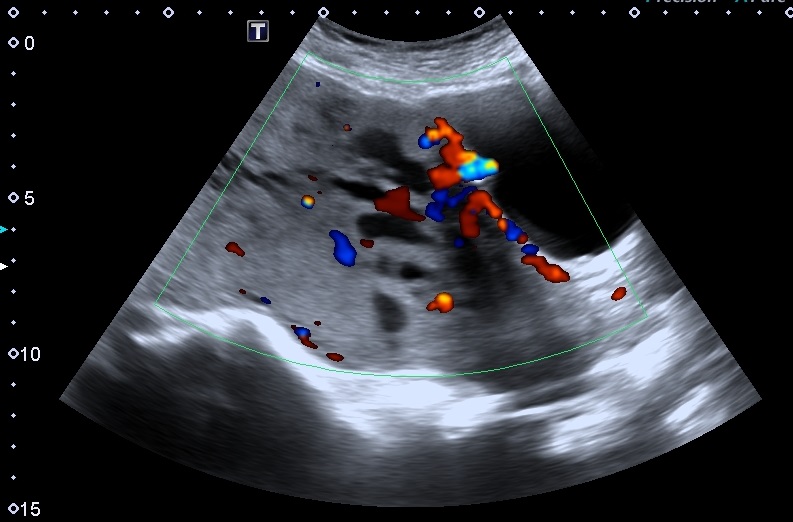
- Findings on ultrasound during pregnancy suggestive of morbidly adherent placenta include nonvisible retro-placental clear zone and persistent blood flow from the myometrium into the placenta (on Doppler sonography).
- Findings on ultrasound suggestive of uterine rupture include pelvic echo-free space which suggests free fluid within the pelvis.
- Findings on ultrasound suggestive of uterine inversion include the collapse of the fundus into the uterine cavity and an inverted fundus (hyperechoic) surrounded by the uterine wall (hypoechoic) on the axial view (target sign).
CT scan
Multidetector CT scan may be helpful in the diagnosis of the underlying etiology of severe postpartum hemorrhage.[23]
- Findings on CT scan suggestive of incomplete uterine rupture include hemoperitoneum and myometrial disruption.
- Unsuccessful uterine artery embolization or ligation of internal iliac arteries may be detected by CT scan with the finding of collateral vessels.
- CT scan may be helpful in the detection of extrauterine sources of bleeding such as rectus sheath hematomas and vascular injuries.
- CT scan may also be helpful for the preprocedural vascular mapping.
MRI
MRI may be helpful in the diagnosis of placenta previa and accreta. Findings on MRI suggestive of placenta previa and accreta include:[24]
- Dark intraplacental T2 bands
- Bulging of placenta or uterus
- Disorganized and abnormal intraplacental vascularity
- Invasion of the placenta into the urinary bladder
- Focal interruption of the myometrial wall
Other Imaging Findings
There are no other imaging findings associated with postpartum hemorrhage.
Other Diagnostic Studies
There are no other diagnostic studies associated with postpartum hemorrhage.
Treatment
Medical Therapy
IV catheter placement, foley catheter placement, bimanual uterine massage, manual exploration of the uterine cavity with the evacuation of retained placental tissue or blood clots, and intravenous fluid therapy are recommended among all patients who develop postpartum hemorrhage.[6]
- For patients with genital tract lacerations, immediate repair with absorbable sutures should be considered.
- Pharmacologic medical therapies for postpartum hemorrhage include either oxytocin (first-line), methylergonovine, carboprost, or misoprostol.
- If oxytocin fails, the abovementioned second-line agents should be considered.
- Additional management measures for patients with estimated blood loss ≥1500-3000 mL include placement of an arterial catheter, placement of a central venous catheter, placement of a uterine balloon tamponade, tranexamic acid administration, and blood transfusion.
- For patients with estimated blood loss ≥ 3000 mL, readministration of tranexamic acid and replacing the missing clotting factors (in hemophilia A and B) should be considered.
Interventional Radiology


Embolization of the uterine artery should be considered among hemodynamically stable patients either resistant to medical treatment or with an estimated blood loss ≥ 3000 mL.[6]
Surgery
Surgery is not the first-line treatment option for patients with postpartum hemorrhage. Surgery is usually reserved for patients either with bleeding resistant to the less invasive measures, estimated blood loss ≥ 3000 mL, or hemodynamic instability.[6]
- For patients with uterine rupture or lacerations, laparoscopic repair should be considered.
- Uterine compression sutures (e.g., B-Lynch, Hayman) are recommended in patients with uterine atony resistant to less invasive approaches (bimanual uterine massage, administration of uterotonic agents, etc.).
- If uterine compression sutures or balloon tamponades fail, bilateral uterine artery ligation should be considered.
- If the management with bilateral uterine artery ligation fails, the next step could be the ligation of a bilateral utero-ovarian artery. The last choice before the hysterectomy is the ligation of the internal iliac artery.
- If all measures fail to control the bleeding, hysterectomy should be considered as a life-saving measure. However, hysterectomy might be considered at an earlier step in the treatment for patients without fertility desires.
- If the management with bilateral uterine artery ligation fails, the next step could be the ligation of a bilateral utero-ovarian artery. The last choice before the hysterectomy is the ligation of the internal iliac artery.
- If uterine compression sutures or balloon tamponades fail, bilateral uterine artery ligation should be considered.
Primary Prevention
Effective measures for the primary prevention of postpartum hemorrhage include[6]
- Replenishing iron stores and increasing hemoglobin concentration in patients with high risk (ideally prior to conception)
- Preparation for the labor according to the risk factors
- Risk factors that indicate a moderate risk of postpartum hemorrhage include prior cesarean section or uterine surgery, multiple birth, chorioamnionitis, BMI (body-mass index) >40, fetal macrosomia ( >4000 g), prior postpartum hemorrhage, intrauterine fetal demise, and more than 4 previous vaginal deliveries.
- Effective measures for the primary prevention of postpartum hemorrhage in patients with moderate risk include blood typing and screening.
- Risk factors that indicate a high risk of postpartum hemorrhage include placenta previa, maternal coagulopathy, active bleeding on admission, the possibility of the placenta accreta spectrum according to the imaging findings, hemoglobin <10 mg/dl, and platelet count <100,000/μl.
- Effective measures for the primary prevention of postpartum hemorrhage in patients with high risk include blood typing and cross-matching of at least two units of packed red blood cells (pRBC).
- Risk factors that indicate a moderate risk of postpartum hemorrhage include prior cesarean section or uterine surgery, multiple birth, chorioamnionitis, BMI (body-mass index) >40, fetal macrosomia ( >4000 g), prior postpartum hemorrhage, intrauterine fetal demise, and more than 4 previous vaginal deliveries.
- The active management of the third stage of labor (AMTSL) compared to the physiological (expectant) management reduces the risk of postpartum hemorrhage.
Secondary Prevention
Effective measures for the secondary prevention of postpartum hemorrhage include the administration of 800 mcg sublingual misoprostol to patients with postpartum blood loss ≥350 mL.[27]
References
- ↑ 1.0 1.1 Prata N, Bell S, Weidert K (2013). "Prevention of postpartum hemorrhage in low-resource settings: current perspectives". Int J Womens Health. 5: 737–52. doi:10.2147/IJWH.S51661. PMC 3833941. PMID 24259988.
- ↑ Hofmeyr GJ, Mshweshwe NT, Gülmezoglu AM (January 2015). "Controlled cord traction for the third stage of labor". Cochrane Database Syst Rev. 1: CD008020. doi:10.1002/14651858.CD008020.pub2. PMC 6464177. PMID 25631379.
- ↑ Prendiville WJ, Harding JE, Elbourne DR, Stirrat GM (November 1988). "The Bristol third stage trial: active versus physiological management of third stage of labour". BMJ. 297 (6659): 1295–300. doi:10.1136/bmj.297.6659.1295. PMC 1834913. PMID 3144366.
- ↑ El-Hamamy E, Wright A, B-Lynch C (May 2009). "The B-Lynch suture technique for postpartum haemorrhage: a decade of experience and outcome". J Obstet Gynaecol. 29 (4): 278–83. doi:10.1080/01443610902797645. PMID 19835492.
- ↑ Derman RJ, Kodkany BS, Goudar SS, Geller SE, Naik VA, Bellad MB, Patted SS, Patel A, Edlavitch SA, Hartwell T, Chakraborty H, Moss N (October 2006). "Oral misoprostol in preventing postpartum haemorrhage in resource-poor communities: a randomised controlled trial". Lancet. 368 (9543): 1248–53. doi:10.1016/S0140-6736(06)69522-6. PMID 17027730.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 Bienstock JL, Eke AC, Hueppchen NA (2021). "Postpartum Hemorrhage". N Engl J Med. 384 (17): 1635–1645. doi:10.1056/NEJMra1513247. PMID 33913640 Check
|pmid=value (help). - ↑ Breathnach F, Geary M (2009). "Uterine atony: definition, prevention, nonsurgical management, and uterine tamponade". Semin Perinatol. 33 (2): 82–7. doi:10.1053/j.semperi.2008.12.001. PMID 19324236.
- ↑ "ACOG Practice Bulletin No. 198: Prevention and Management of Obstetric Lacerations at Vaginal Delivery". Obstet Gynecol. 132 (3): e87–e102. September 2018. doi:10.1097/AOG.0000000000002841. PMID 30134424.
- ↑ Silver RM, Major H (March 2010). "Maternal coagulation disorders and postpartum hemorrhage". Clin Obstet Gynecol. 53 (1): 252–64. doi:10.1097/GRF.0b013e3181cef930. PMID 20142661.
- ↑ 10.0 10.1 10.2 10.3 10.4 "ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: postpartum hemorrhage". Obstet Gynecol. 108 (4): 1039–47. October 2006. doi:10.1097/00006250-200610000-00046. PMID 17012482.
- ↑ 11.0 11.1 11.2 Oyelese Y, Ananth CV (March 2010). "Postpartum hemorrhage: epidemiology, risk factors, and causes". Clin Obstet Gynecol. 53 (1): 147–56. doi:10.1097/GRF.0b013e3181cc406d. PMID 20142652.
- ↑ Shirazee HH, Saha SK, Das I, Mondal T, Samanta S, Sarkar M (October 2010). "Postpartum haemorrhage: a cause of maternal morbidity". J Indian Med Assoc. 108 (10): 663–6. PMID 21510550.
- ↑ 13.0 13.1 Gyamfi-Bannerman C, Srinivas SK, Wright JD, Goffman D, Siddiq Z, D'Alton ME; et al. (2018). "Postpartum hemorrhage outcomes and race". Am J Obstet Gynecol. 219 (2): 185.e1–185.e10. doi:10.1016/j.ajog.2018.04.052. PMID 29752934. Review in: Evid Based Nurs. 2019 Apr;22(2):57
- ↑ Fukami T, Koga H, Goto M, Ando M, Matsuoka S, Tohyama A, Yamamoto H, Nakamura S, Koyanagi T, To Y, Kondo H, Eguchi F, Tsujioka H (2019). "Incidence and risk factors for postpartum hemorrhage among transvaginal deliveries at a tertiary perinatal medical facility in Japan". PLoS One. 14 (1): e0208873. doi:10.1371/journal.pone.0208873. PMC 6326562. PMID 30625154.
- ↑ Le Bas A, Chandraharan E, Addei A, Arulkumaran S (March 2014). "Use of the "obstetric shock index" as an adjunct in identifying significant blood loss in patients with massive postpartum hemorrhage". Int J Gynaecol Obstet. 124 (3): 253–5. doi:10.1016/j.ijgo.2013.08.020. PMID 24373705.
- ↑ Chandraharan E, Krishna A (September 2017). "Diagnosis and management of postpartum haemorrhage". BMJ. 358: j3875. doi:10.1136/bmj.j3875. PMID 28954732.
- ↑ Wormer KC, Jamil RT, Bryant SB. PMID 29763164. Missing or empty
|title=(help) - ↑ Quiñones JN, Uxer JB, Gogle J, Scorza WE, Smulian JC (March 2010). "Clinical evaluation during postpartum hemorrhage". Clin Obstet Gynecol. 53 (1): 157–64. doi:10.1097/GRF.0b013e3181cd5d36. PMID 20142653.
- ↑ Rath WH (May 2011). "Postpartum hemorrhage--update on problems of definitions and diagnosis". Acta Obstet Gynecol Scand. 90 (5): 421–8. doi:10.1111/j.1600-0412.2011.01107.x. PMID 21332452.
- ↑ Karpati PC, Rossignol M, Pirot M, Cholley B, Vicaut E, Henry P, Kévorkian JP, Schurando P, Peynet J, Jacob D, Payen D, Mebazaa A (January 2004). "High incidence of myocardial ischemia during postpartum hemorrhage". Anesthesiology. 100 (1): 30–6, discussion 5A. doi:10.1097/00000542-200401000-00009. PMID 14695721.
- ↑ Oba T, Hasegawa J, Sekizawa A (July 2017). "Postpartum ultrasound: postpartum assessment using ultrasonography". J Matern Fetal Neonatal Med. 30 (14): 1726–1729. doi:10.1080/14767058.2016.1223034. PMID 27578054.
- ↑ <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/84897">rID: 84897</a>)
- ↑ Sierra A, Burrel M, Sebastia C, Radosevic A, Barrufet M, Albela S, Buñesch L, Domingo MA, Salvador R, Real I (2012). "Utility of multidetector CT in severe postpartum hemorrhage". Radiographics. 32 (5): 1463–81. doi:10.1148/rg.325115113. PMID 22977030.
- ↑ Chen D, Xu J, Ye P, Li M, Duan X, Zhao F, Liu X, Wang X, Peng B (March 2020). "Risk scoring system with MRI for intraoperative massive hemorrhage in placenta previa and accreta". J Magn Reson Imaging. 51 (3): 947–958. doi:10.1002/jmri.26922. PMID 31507024.
- ↑ <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/24678">rID: 24678</a>)
- ↑ <a href="https://radiopaedia.org/">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/24678">rID: 24678</a>)
- ↑ Raghavan S, Geller S, Miller S, Goudar SS, Anger H, Yadavannavar MC, Dabash R, Bidri SR, Gudadinni MR, Udgiri R, Koch AR, Bellad MB, Winikoff B (January 2016). "Misoprostol for primary versus secondary prevention of postpartum haemorrhage: a cluster-randomised non-inferiority community trial". BJOG. 123 (1): 120–7. doi:10.1111/1471-0528.13540. PMC 5014137. PMID 26333044.