Polyarteritis nodosa
Template:DiseaseDisorder infobox Template:Search infobox
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Haritha Machavarapu, M.B.B.S.
For the heart in Polyarteritis Nodosa click here
Overview
Polyarteritis nodosa (or periarteritis nodosa) is a vasculitis of medium-sized arteries, which become swollen and damaged from attack by rogue immune cells. Polyarteritis nodosa is also called Kussmaul disease or Kussmaul-Meier disease.[1]
Pathophysiology
Polyarteritis nodosa is a disease of unknown cause that affects arteries, the blood vessels that carry oxygenated blood to organs and tissues. It occurs when certain immune cells attack the affected arteries.Inflammation starts in the vessel intima and results in fibrinoid necrosis by destroying the internal and external elastic lamina. Aneurysms and thrombi may develop at the site of lesions. One hypothesis is that this condition is caused by antibodies against HBV, via a type IIII hypersensitivity reaction.
Epidemiology and Demographics
The condition affects adults more frequently than children. It damages the tissues supplied by the affected arteries because they don't receive enough oxygen and nourishment without a proper blood supply. Polyarteritis nodosa is more common in people with hepatitis B infection.
Natural History, Prognosis, and Complications
Therapy results in remissions or cures in 90% of cases. Untreated, the disease is fatal in most cases. The most serious associated conditions generally involve the kidneys and gastrointestinal tract. Without treatment, the outlook is poor. Guillevin and coworkers have described five prognostic factors that predict high probability of mortality and are considered indications for another immunosuppressive drug in addition to prednisone.
- Proteinuria >1g/day
- Azotemia
- Cardiomyopathy
- Gastrointestinal involvement
- Central nervous system disease
With none of these factors, 5-year mortality is 12%. With 2 or more 5-year mortality is 46%[2]
Complications include the following:
- Stroke
- Kidney failure
- Heart attack
- Intestinal necrosis and perforation
Diagnosis
Symptoms
- Fatigue
- Weakness
- Fever
- Abdominal pain
- Decreased appetite
- Unintentional weight loss
- Muscle aches
- Joint aches
- Skin ulcers
In this disease, symptoms result from damage to affected organs, often the skin, heart, kidneys, and nervous system.
Generalized symptoms include fever, fatigue, weakness, loss of appetite, and weight loss. Muscle and joint aches are common. Cutaneous polyarteritis nodosa most frequently manifests as nodules in the lower legs. they may not leave any residual changes but sometimes livedo reticularis is observed. Ulcerations and splinter hemorrhages are the frequent complications.[3]
Nerve involvement may cause sensory changes with numbness, pain, burning, and weakness. Central nervous system involvement may cause strokes or seizures. Kidney involvement can produce varying degrees of renal failure.
Involvement of the arteries of the heart may cause a heart attack, heart failure, and inflammation of the sac around the heart (pericarditis).
Laboratory Studies
There are no specific lab tests for diagnosing polyarteritis nodosa. Diagnosis is generally based upon the physical examination and a few laboratory studies that help to confirm the diagnosis:
- CBC (may demonstrate an elevated white blood count)
- ESR (often elevated)
- Perinuclear pattern of antineutrophil cytoplasmic antibodies (p-ANCA) - not associated with "classic" polyarteritis nodosa, but is present in a form of the disease affecting smaller blood vessels, known as microscopic polyangiitis or leukocytoclastic angiitis.
- Tissue biopsy (reveals inflammation in small arteries, called arteritis)
- Elevated c reactive protein
Diagnostic Criteria
A patient is said to have polyarteritis nodosa if he or she has 3 of the 10 following signs:
- Weight loss ≥4 kg.
- Livedo reticularis (a mottled purplish skin discoloration over the extremities or torso).
- Testicular pain or tenderness. (occasionally, a site biopsied for diagnosis).
- Muscle pain, weakness, or leg tenderness.
- Nerve disease (either single or multiple).
- Diastolic blood pressure greater than 90mmHg (high blood pressure).
- Elevated kidney blood tests (BUN greater than 40 mg/dl or creatinine greater than 1.5 mg/dl).
- Hepatitis B virus tests positive (for surface antigen or antibody).
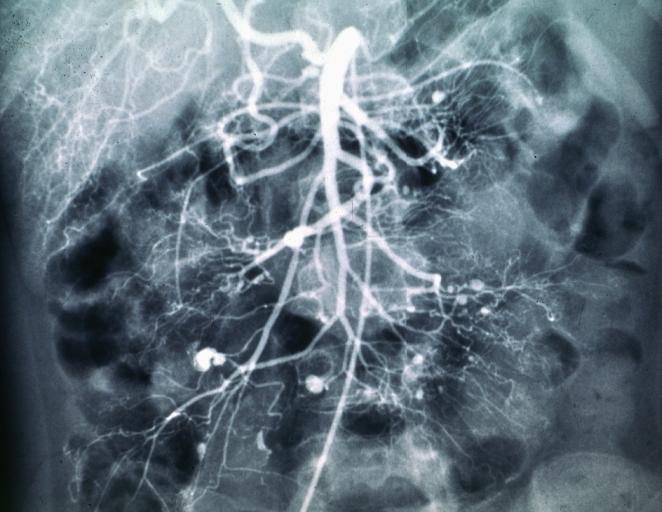
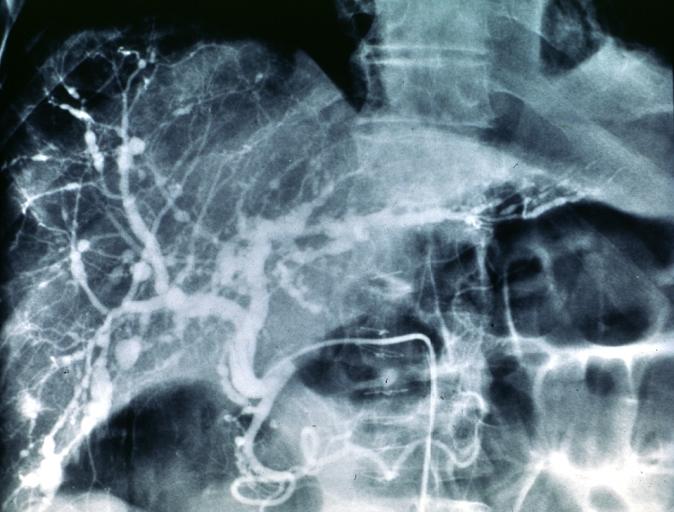
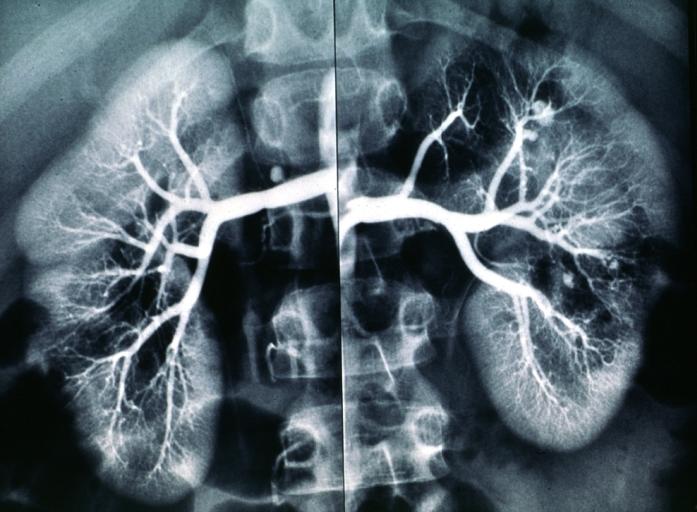
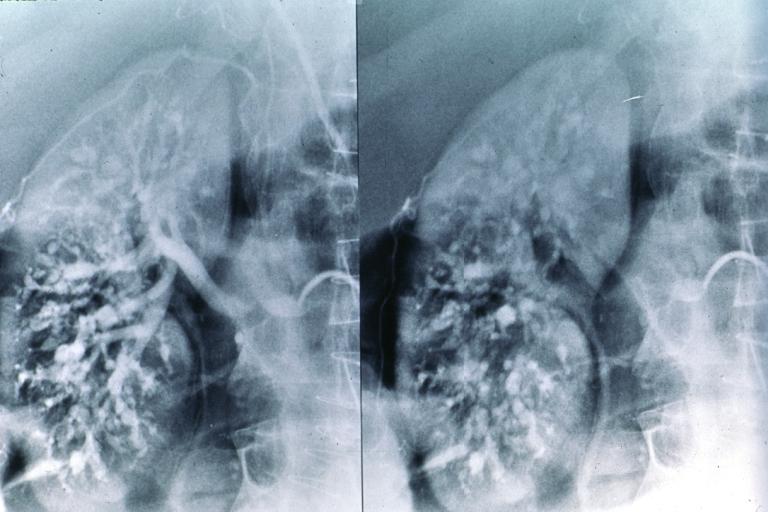
- Arteriogram (angiogram) showing the arteries that are dilated (aneurysms) or constricted by the blood vessel inflammation.
- Biopsy of tissue showing the arteritis (typically inflamed arteries).[4]
Diagnostic x-ray images
Treatment
Treatment involves medications to suppress the immune system, including prednisone and cyclophosphamide.
References
- ↑ Template:WhoNamedIt
- ↑ Kelley's Textbook of Rheumatology,8th edition
- ↑ Díaz-Pérez JL, De Lagrán ZM, Díaz-Ramón JL, Winkelmann RK (2007). "Cutaneous polyarteritis nodosa". Semin Cutan Med Surg. 26 (2): 77–86. doi:10.1016/j.sder.2007.02.003. PMID 17544958. Unknown parameter
|month=ignored (help) - ↑ Shiel, Jr., William C, http://www.medicinenet.com/polyarteritis_nodosa/article.htm
de:Polyarteriitis nodosa nl:Polyarteritis nodosa sv:Polyarteritis nodosa