Polyarteritis nodosa
Template:DiseaseDisorder infobox Template:Search infobox Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [3]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
For the heart in Polyarteritis Nodosa click here
Overview
Polyarteritis nodosa (or periarteritis nodosa) is a vasculitis of medium-sized arteries, which become swollen and damaged from attack by rogue immune cells. Polyarteritis nodosa is also called Kussmaul disease or Kussmaul-Meier disease.[1]
Pathophysiology
Polyarteritis nodosa is a disease of unknown cause that affects arteries, the blood vessels that carry oxygenated blood to organs and tissues. It occurs when certain immune cells attack the affected arteries. One hypothesis is that this condition is caused by antibodies against HBV, via a type III hypersensitivity reaction.
Epidemiology and Demographics
The condition affects adults more frequently than children. It damages the tissues supplied by the affected arteries because they don't receive enough oxygen and nourishment without a proper blood supply. Polyarteritis nodosa is more common in people with hepatitis B infection.
Diagnosis
Symptoms
List of Symptoms
- Fatigue
- Weakness
- Fever
- Abdominal pain
- Decreased appetite
- Unintentional weight loss
- Muscle aches
- Joint aches
In this disease, symptoms result from damage to affected organs, often the skin, heart, kidneys, and nervous system.
Generalised symptoms include fever, fatigue, weakness, loss of appetite, and weight loss. Muscle and joint aches are common. The skin may show rashes, swelling, ulcers, and lumps.
Nerve involvement may cause sensory changes with numbness, pain, burning, and weakness. Central nervous system involvement may cause strokes or seizures. Kidney involvement can produce varying degrees of renal failure.
Involvement of the arteries of the heart may cause a heart attack, heart failure, and inflammation of the sac around the heart (pericarditis).
Laboratory Studies
There are no specific lab tests for diagnosing polyarteritis nodosa. Diagnosis is generally based upon the physical examination and a few laboratory studies that help to confirm the diagnosis:
- CBC (may demonstrate an elevated white blood count)
- ESR (often elevated)
- Perinuclear pattern of antineutrophil cytoplasmic antibodies (p-ANCA) - not associated with "classic" polyarteritis nodosa, but is present in a form of the disease affecting smaller blood vessels, known as microscopic polyangiitis or leukocytoclastic angiitis.
- Tissue biopsy (reveals inflammation in small arteries, called arteritis)
- Elevated c reactive protein
Diagnostic Criteria
A patient is said to have polyarteritis nodosa if he or she has 3 of the 10 following signs:
- Weight loss ≥4 kg.
- Livedo reticularis (a mottled purplish skin discoloration over the extremities or torso).
- Testicular pain or tenderness. (occasionally, a site biopsied for diagnosis).
- Muscle pain, weakness, or leg tenderness.
- Nerve disease (either single or multiple).
- Diastolic blood pressure greater than 90mmHg (high blood pressure).
- Elevated kidney blood tests (BUN greater than 40 mg/dl or creatinine greater than 1.5 mg/dl).
- Hepatitis B virus tests positive (for surface antigen or antibody).
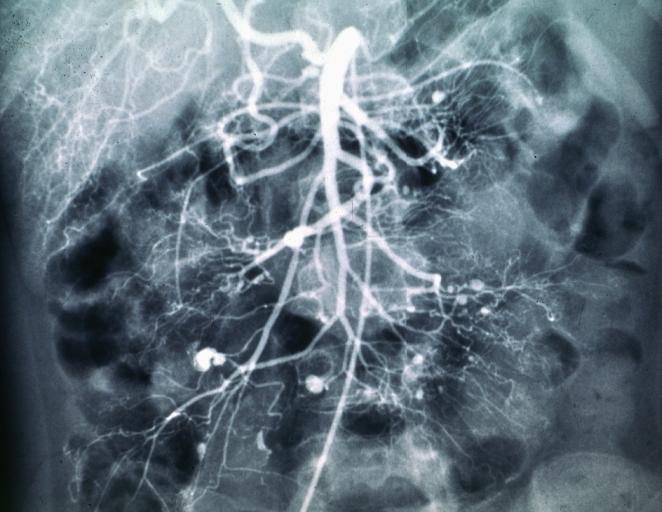
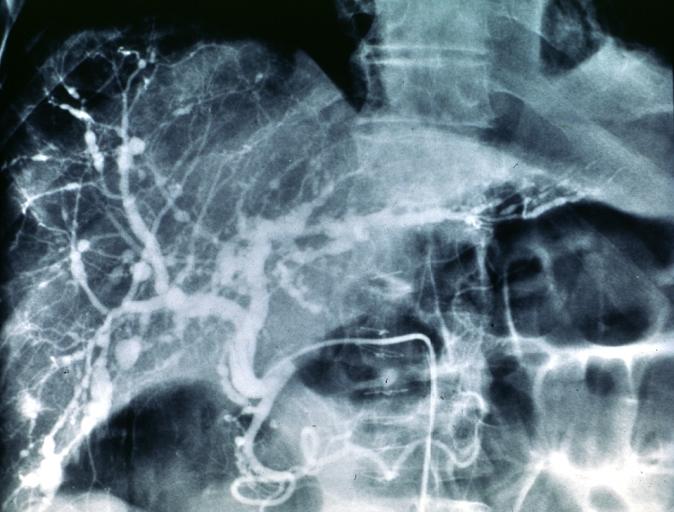
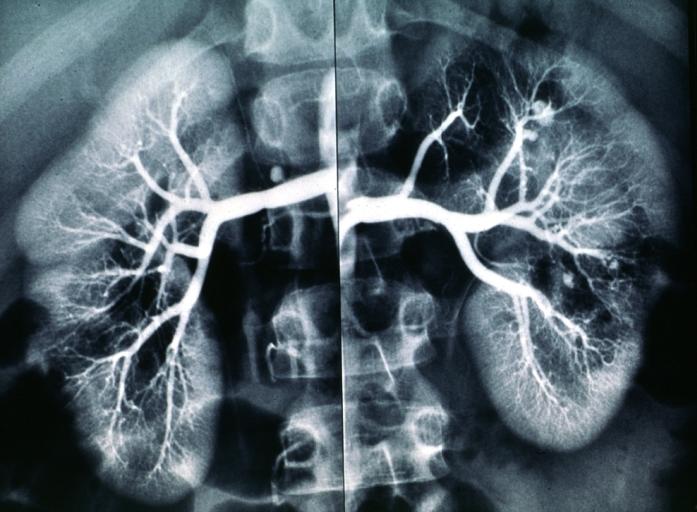
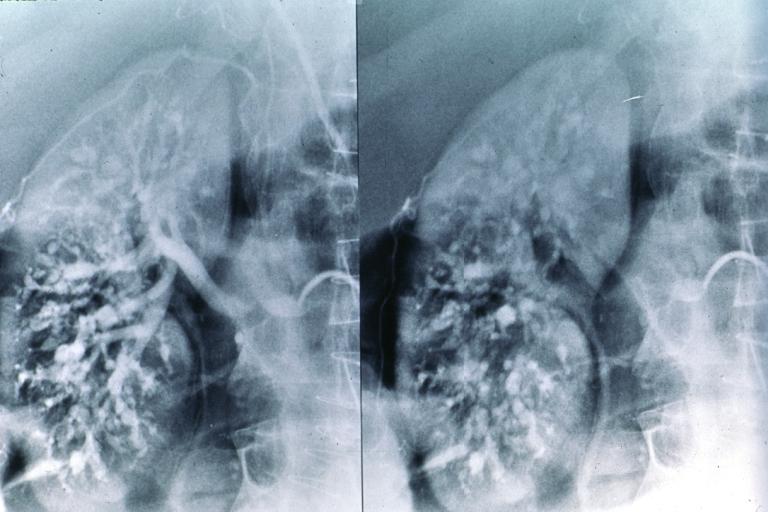
- Arteriogram (angiogram) showing the arteries that are dilated (aneurysms) or constricted by the blood vessel inflammation.
- Biopsy of tissue showing the arteritis (typically inflamed arteries).[2]
Diagnostic x-ray images
Treatment and Prognosis
Treatment involves medications to suppress the immune system, including prednisone and cyclophosphamide. Therapy results in remissions or cures in 90% of cases. Untreated, the disease is fatal in most cases. The most serious associated conditions generally involve the kidneys and gastrointestinal tract. Without treatment, the outlook is poor.
Complications
- Stroke
- Kidney failure
- Heart attack
- Intestinal necrosis and perforation
Prevention
This disease cannot be currently prevented, but early treatment can prevent some damage and symptoms.
References
- ↑ Template:WhoNamedIt
- ↑ Shiel, Jr., William C, http://www.medicinenet.com/polyarteritis_nodosa/article.htm
External links
Template:Diseases of the musculoskeletal system and connective tissue
Template:SIB
de:Polyarteriitis nodosa nl:Polyarteritis nodosa sv:Polyarteritis nodosa