Pneumocystis jirovecii pneumonia
For patient information click here
| Pneumocystis jirovecii pneumonia |
|
Pneumocystis jirovecii pneumonia Microchapters |
|
Differentiating Pneumocystis jirovecii pneumonia from other Diseases |
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Pneumocystis jirovecii pneumonia On the Web |
|
American Roentgen Ray Society Images of Pneumocystis jirovecii pneumonia |
|
Risk calculators and risk factors for Pneumocystis jirovecii pneumonia |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Pneumocystis jirovecii (previously classified as Pneumocystis carinii) was previously classified as a protozoa. Currently, it is considered a fungus based on nucleic acid and biochemical analysis.
Epidemiology and Demographics
Pneumocystis jirovecii pneumonia exists worldwide, in humans and animals. Serologic evidence indicates that most healthy children have been exposed by age 3 to 4. Pneumocystis pneumonia (PCP) occurs in immunosuppressed individuals and in premature, malnourished infants.
Pathophysiology & Etiology
Pneumocystis jirovecii (previously classified as Pneumocystis carinii) was previously classified as a protozoa. Currently, it is considered a fungus based on nucleic acid and biochemical analysis.
This is a generalized life cycle proposed by John J. Ruffolo, Ph.D. (Cushion, MT, 1988) for the various species of Pneumocystis. These fungi are found in the lungs of mammals where they reside without causing overt infection until the host's immune system becomes debilitated. Then, an oftentimes lethal pneumonia can result. 1 Asexual phase: trophic forms replicate by mitosis 2 to 3. Sexual phase: haploid trophic forms conjugate 1 and produce a zygote or sporocyte (early cyst) 2. The zygote undergoes meiosis and subsequent mitosis to produce eight haploid nuclei (late phase cyst) 3. Spores exhibit different shapes (such as, spherical and elongated forms). It is postulated that elongation of the spores precedes release from the spore case. It is believed that the release occurs through a rent in the cell wall. After release, the empty spore case usually collapses, but retains some residual cytoplasm 4. A trophic stage, where the organisms probably multiply by binary fission is also recognized to exist. The organism causes disease in immunosuppressed individuals.
History and Symptoms
The symptoms of Pneumocystis pneumonia (PCP) include dyspnea, nonproductive cough, and fever. Chest radiography demonstrates bilateral infiltrates. Extrapulmonary lesions occur in a minority (<3%) of patients, involving most frequently the lymph nodes, spleen, liver, and bone marrow. Typically, in untreated PCP increasing pulmonary involvement leads to death.
Laboratory Findings
The specific diagnosis is based on identification of P. jirovecii in bronchopulmonary secretions obtained as induced sputum or bronchoalveolar lavage (BAL) material. In situations where these two techniques cannot be used, transbronchial biopsy or open lung biopsy may prove necessary. Microscopic identification of P. jiroveci trophozoites and cysts is performed with stains that demonstrate either the nuclei of trophozoites and intracystic stages (such as Giemsa) or the cyst walls (such as the silver stains). In addition, immunofluorescence microscopy using monoclonal antibodies can identify the organisms with higher sensitivity than conventional microscopy.
Microscopic
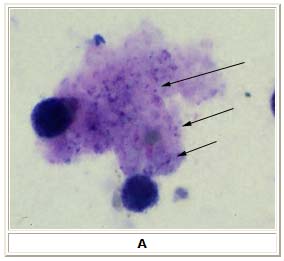
A: Pneumocystis jirovecii trophozoites in bronchoalveolar lavage (BAL) material. Giemsa stain. The trophozoites are small (size: 1 to 5 µm), and only their nuclei, stained purple, are visible (arrows). AIDS patient seen in Atlanta, Georgia.
Pneumocystis jirovecii cysts
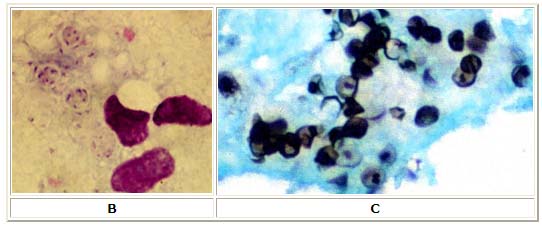
B: 3 cysts in bronchoalveolar material, Giemsa stain; the rounded cysts (size 4 to 7 µm) contain 6 to 8 intracystic bodies, whose nuclei are stained by Giemsa; the walls of the cysts are not stained; note the presence of several smaller, isolated trophozoites.
C: Cysts in lung tissue, silver stain; the walls of the cysts are stained black; the intracystic bodies are not visible with this stain; baby who died with pneumonia in California.
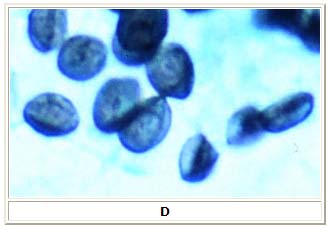
D: Pneumocystis jirovecii cysts in bronchoalveolar lavage material; silver stain; this greater magnification shows the irregular, saucer shape of the cysts.
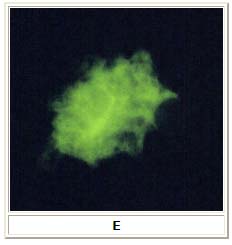
E: Indirect immunofluorescence using monoclonal antibodies against Pneumocystis jirovecii. Specimen from a patient with AIDS, seen in Georgia.
Molecular
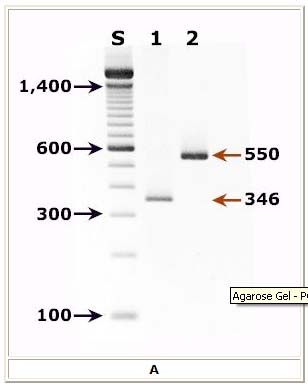
Molecular methods for detection of P. jirovecii have shown very high sensitivity and specificity and constitute the gold standard for detection of this pathogen.
A: Agarose gel (2%) analysis of PCR-amplified products from DNA extracted from a bronchoalveolar lavage (BAL) diagnostic specimen of a patient with pulmonary symptoms.
- Lane S: Molecular base pair standard (100-bp ladder). Black arrows show the size of standard bands.
- Lane 1: Single step PCR amplification with the pAZ102-E/pAZ102-H primer pair1 - diagnostic band size: 346 bp.
- Lane 2: Nested PCR amplification with the ITS nested PCR primers, 1724F/ITS2R (first round) and ITS1F/ITS2R1 (second round)2 - diagnostic band size: 550 bp.
Treatment
Pharmacotherapy
Trimethoprim-sulfamethoxazole is the drug of choice. Recommended alternatives include pentamidine; trimethoprim plus dapsone; atovaquone; and primaquine plus clindamycin.
References
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson, M.S., M.D. Template:WH Template:WS