Pneumococcal Vaccine 13-Valent
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Pneumococcal Vaccine 13-Valent is a vaccine that is FDA approved for the prophylaxis of infecetions caused by S. pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F and 23F in children 6 weeks to 17 years-old and adults 50 years old and older. Common adverse reactions include erythema at injection site, injection site pain, swelling at injection site, tenderness, decrease in appetite, aggravated and new onset arthralgia, difficulty moving arm, aggravated and new onset myalgia, decreased sleep, headache, hypersomnia, irritability, fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Preparation for Administration
Since this product is a suspension containing an adjuvant, shake vigorously immediately prior to use to obtain a homogenous, white suspension in the vaccine container. Do not use the vaccine, if it cannot be resuspended. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration. This product should not be used if particulate matter or discoloration is found.
Do not mix Prevnar 13 with other vaccines/products in the same syringe.
Administration Information
For intramuscular injection only.
Each 0.5 mL dose is to be injected intramuscularly using a sterile needle attached to the supplied prefilled syringe. The preferred sites for injection are the anterolateral aspect of the thigh in infants and the deltoid muscle of the upper arm in toddlers, children and adults. The vaccine should not be injected in the gluteal area or areas where there may be a major nerve trunk and/or blood vessel.
Vaccination Schedule for Adults 50 years of Age and Older
Prevnar 13 is administered as a single dose.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pneumococcal Vaccine 13-Valent in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pneumococcal Vaccine 13-Valent in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Preparation for Administration
Since this product is a suspension containing an adjuvant, shake vigorously immediately prior to use to obtain a homogenous, white suspension in the vaccine container. Do not use the vaccine, if it cannot be resuspended. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration [see Description (11)]. This product should not be used if particulate matter or discoloration is found.
Do not mix Prevnar 13 with other vaccines/products in the same syringe.
Administration Information
For intramuscular injection only.
Each 0.5 mL dose is to be injected intramuscularly using a sterile needle attached to the supplied prefilled syringe. The preferred sites for injection are the anterolateral aspect of the thigh in infants and the deltoid muscle of the upper arm in toddlers, children and adults. The vaccine should not be injected in the gluteal area or areas where there may be a major nerve trunk and/or blood vessel.
Vaccination Schedule for Infants and Toddlers
Prevnar 13 is to be administered as a four-dose series at 2, 4, 6, and 12–15 months of age.

Vaccination Schedule for Unvaccinated Children 7 Months Through 5 Years of Age
For children 7 months through 5 years of age who have not received Prevnar® or Prevnar 13, the catch-up schedule in Table 2 applies:

The immune responses induced by this catch-up schedule may result in lower antibody concentrations for some serotypes, compared to antibody concentrations following 4 doses of Prevnar 13 (given at 2, 4, 6, and 12–15 months). In children 24 months through 5 years of age, lower antibody concentrations were observed for some serotypes, compared to antibody concentrations following 3 doses of Prevnar 13 (given at 2, 4, and 6 months).
Vaccination Schedule for Children Previously Vaccinated With Prevnar Pneumococcal 7-valent Conjugate Vaccine (Diphtheria CRM197 Protein)
Children 15 months through 5 years of age who are considered completely immunized with Prevnar may receive one dose of Prevnar 13 to elicit immune responses to the six additional serotypes. This catch-up (supplemental) dose of Prevnar 13 should be administered with an interval of at least 8 weeks after the final dose of Prevnar. The immune responses induced by this Prevnar 13 schedule may result in lower antibody concentrations for the 6 additional serotypes (types 1, 3, 5, 6A, 7F, and 19A), compared to antibody concentrations following 4 doses of Prevnar 13 (given at 2, 4, 6, and 12–15 months).
Vaccination Schedule for Children 6 Years Through 17 Years of Age
In children 6 years through 17 years of age, Prevnar 13 is administered as single dose. If Prevnar was previously administered, then at least 8 weeks should elapse before receiving Prevnar 13.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pneumococcal Vaccine 13-Valent in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pneumococcal Vaccine 13-Valent in pediatric patients.
Contraindications
Severe allergic reaction (e.g., anaphylaxis) to any component of Prevnar 13 or any diphtheria toxoid-containing vaccine.
Warnings
Management of Allergic Reactions
Epinephrine and other appropriate agents used to manage immediate allergic reactions must be immediately available should an acute anaphylactic reaction occur following administration of Prevnar 13.
Altered Immunocompetence
Individuals with altered immunocompetence, including those at higher risk for invasive pneumococcal disease (e.g., individuals with congenital or acquired splenic dysfunction, HIV infection, malignancy, hematopoietic stem cell transplant, nephrotic syndrome), may have reduced antibody responses to immunization with Prevnar 13.
Apnea in Premature Infants
Apnea following intramuscular vaccination has been observed in some infants born prematurely. Decisions about when to administer an intramuscular vaccine, including Prevnar 13, to infants born prematurely should be based on consideration of the individual infant's medical status and the potential benefits and possible risks of vaccination.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse-reaction rates observed in the clinical trials of a vaccine cannot be directly compared to rates in the clinical trials of another vaccine and may not reflect the rates observed in practice. As with any vaccine, there is the possibility that broad use of Prevnar 13 could reveal adverse reactions not observed in clinical trials.
Clinical Trials Experience With Prevnar 13 in Children 6 Weeks Through 17 Years of Age
The safety of Prevnar 13 was evaluated in 13 clinical trials in which 4,729 infants (6 weeks through 11 months of age) and toddlers (12 months through 15 months of age) received at least one dose of Prevnar 13 and 2,760 infants and toddlers received at least one dose of Prevnar active control. Safety data for the first three doses are available for all 13 infant studies; dose 4 data are available for 10 studies; and data for the 6-month follow-up are available for 7 studies. The vaccination schedule and concomitant vaccinations used in these infant trials were consistent with country-specific recommendations and local clinical practice. There were no substantive differences in demographic characteristics between the vaccine groups. By race, 84.0% of subjects were White, 6.0% were Black or African-American, 5.8% were Asian and 3.8% were of 'Other' race (most of these being biracial). Overall, 52.3% of subjects were male infants.
Three studies in the US (Studies 1, 2 and 3) evaluated the safety of Prevnar 13 when administered concomitantly with routine US pediatric vaccinations at 2, 4, 6, and 12–15 months of age. Solicited local and systemic adverse events were recorded daily by parents/guardians using an electronic diary for 7 consecutive days following each vaccination. For unsolicited adverse events, study subjects were monitored from administration of the first dose until one month after the infant series, and for one month after the administration of the toddler dose. Information regarding unsolicited and serious adverse events, newly diagnosed chronic medical conditions, and hospitalizations since the last visit were collected during the clinic visit for the fourth-study dose and during a scripted telephone interview 6 months after the fourth-study dose. Serious adverse events were also collected throughout the study period. Overall, the safety data show a similar proportion of Prevnar 13 and Prevnar subjects reporting serious adverse events. Among US study subjects, a similar proportion of Prevnar 13 and Prevnar recipients reported solicited local and systemic adverse reactions as well as unsolicited adverse events.
Serious Adverse Events in All Infant and Toddler Clinical Studies
Serious adverse events were collected throughout the study period for all 13 clinical trials. This reporting period is longer than the 30-day post-vaccination period used in some vaccine trials. The longer reporting period may have resulted in serious adverse events being reported in a higher percentage of subjects than for other vaccines. Serious adverse events reported following vaccination in infants and toddlers occurred in 8.2% among Prevnar 13 recipients and 7.2% among Prevnar recipients. Serious adverse events observed during different study periods for Prevnar 13 and Prevnar respectively were: 1) 3.7% and 3.5% from dose 1 to the bleed approximately 1 month after the infant series; 2) 3.6% and 2.7% from the bleed after the infant series to the toddler dose; 3) 0.9% and 0.8% from the toddler dose to the bleed approximately 1 month after the toddler dose and 4) 2.5% and 2.8% during the 6 month follow up period after the last dose.
The most commonly reported serious adverse events were in the 'Infections and infestations' system organ class including bronchiolitis (0.9%, 1.1%), gastroenteritis, (0.9%, 0.9%), and pneumonia (0.9%, 0.5%) for Prevnar 13 and Prevnar respectively.
There were 3 (0.063%) deaths among Prevnar 13 recipients, and 1 (0.036%) death in Prevnar recipients, all as a result of sudden infant death syndrome (SIDS). These SIDS rates are consistent with published age specific background rates of SIDS from the year 2000.
Among 6,839 subjects who received at least 1 dose of Prevnar 13 in clinical trials conducted globally, there was 1 hypotonic-hyporesponsive episode adverse reaction reported (0.015%). Among 4,204 subjects who received at least 1 dose of Prevnar in clinical trials conducted globally, there were 3 hypotonic-hyporesponsive episode adverse reactions reported (0.071%). All 4 events occurred in a single clinical trial in Brazil in which subjects received whole cell pertussis vaccine at the same time as Prevnar 13 or Prevnar.
Solicited Adverse Reactions in the Three US Infant and Toddler Studies
A total of 1,907 subjects received at least 1 dose of Prevnar 13 and 701 subjects received at least 1 dose of Prevnar in the three US studies (Studies 1, 2 and 3). Most subjects were White (77.3%), 14.2% were Black or African-American, and 1.7% were Asian; 79.1% of subjects were non-Hispanic and non-Latino and 14.6% were Hispanic or Latino. Overall, 53.6% of subjects were male infants.
The incidence and severity of solicited adverse reactions that occurred within 7 days following each dose of Prevnar 13 or Prevnar administered to US infants and toddlers are shown in Tables 3 and 4.
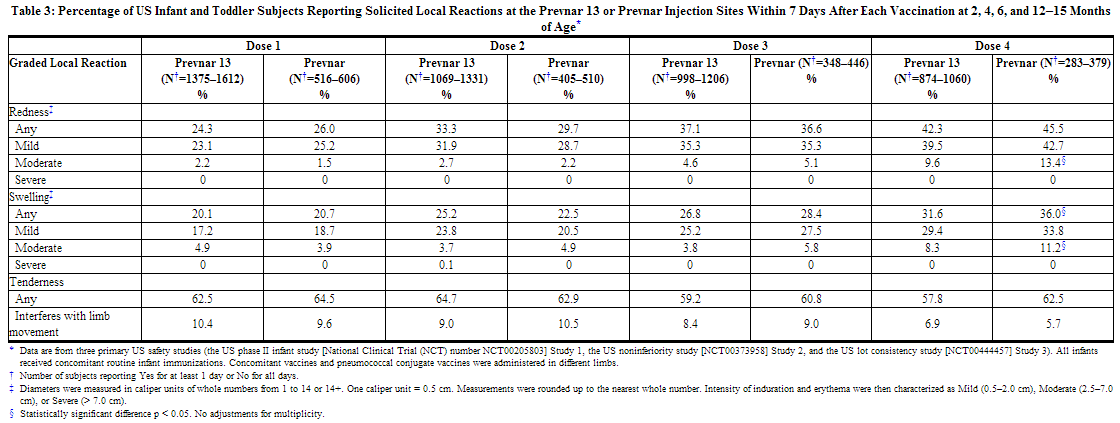

The incidence rates of any fever (≥ 38.0°C) were similar on days 1 and 2 following each dose of Prevnar 13 compared to after each dose of Prevnar administered to US infants and toddlers (day 1 = day of vaccination). After dose 1, fever was reported in 11.0–12.7% on day 1 and 6.4–6.8% on day 2. After dose 2, fever was reported in 12.3–13.1% on day 1 and 12.5–12.8% on day 2. After dose 3, fever was reported in 8.0–9.6% on day 1 and 9.1–10.5% on day 2. And after dose 4, fever was reported in 6.3–6.4% on day 1 and 7.3–9.7% on day 2.
Unsolicited Adverse Reactions in the Three US Infant and Toddler Safety Studies
The following were determined to be adverse drug reactions based on experience with Prevnar 13 in clinical trials.
Reactions occurring in greater than 1% of infants and toddlers: diarrhea, vomiting, and rash.
Reactions occurring in less than 1% of infants and toddlers: crying, hypersensitivity reaction (including face edema, dyspnea, and bronchospasm), seizures (including febrile seizures), and urticaria or urticaria-like rash.
Safety Assessments in the Catch-Up Studies in Infants and Children Through 5 Years of Age
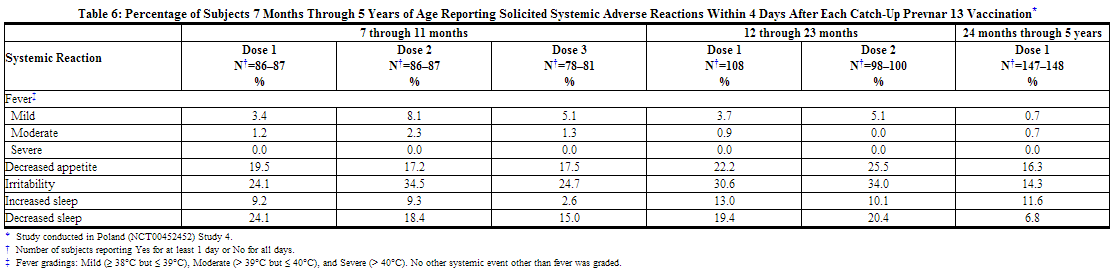
In a catch-up study conducted in Poland (Study 4), 354 children (7 months through 5 years of age) receiving at least one dose of Prevnar 13 were also monitored for safety. All subjects in this study were White and non-Hispanic. Overall, 49.6% of subjects were male infants. The incidence and severity of solicited adverse reactions that occurred within 4 days following each dose of Prevnar 13 administered to pneumococcal-vaccine naïve children 7 months through 5 years of age are shown in Tables 5 and 6.

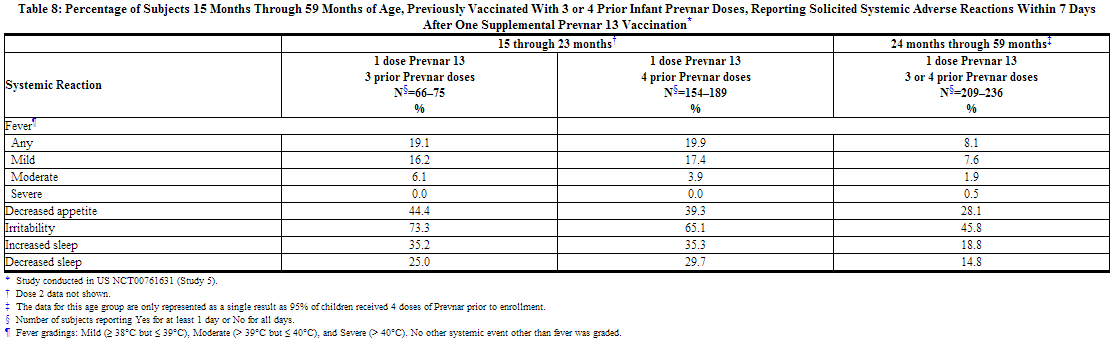
A US study (Study 5) evaluated the use of Prevnar 13 in children previously immunized with Prevnar. In this open label trial, 596 healthy children 15 through 59 months of age previously vaccinated with at least 3 doses of Prevnar, received 1 or 2 doses of Prevnar 13. Children 15 months through 23 months of age (group 1) received 2 doses, and children 24 months through 59 months of age (group 2) received one dose. Most subjects were White (74.3%), 14.9% were Black or African-American, and 1.2% were Asian; 89.3% of subjects were non-Hispanic and non-Latino and 10.7% were Hispanic or Latino. Overall, 52.2% of subjects were male. The incidence and severity of solicited adverse reactions that occurred within 7 days following one dose of Prevnar 13 administered to children 15 months through 59 months of age are shown in Tables 7 and 8.

Clinical Trials Experience With Prevnar 13 in Children 5 Through 17 Years of Age
In a US study (Study 5), the safety of Prevnar 13 was evaluated in children 5 through 9 years of age previously immunized with at least one dose of Prevnar, and in children 10 through 17 years of age with no prior pneumococcal vaccination. In this open label trial, 592 children, including those with asthma, received a single dose of Prevnar 13. The percentage of children 5 through 9 years of age who received 3 and 4 prior doses of Prevnar was 29.1% and 54.5% respectively.
Most subjects were White (72.8%), 21.8% were Black or African-American, and 1.5% were Asian; 91.4% of subjects were non-Hispanic and non-Latino and 8.6% were Hispanic or Latino. Overall, 51.2% of subjects were male.
The incidence and severity of solicited adverse reactions that occurred within 7 days following one dose of Prevnar 13 administered to children 5 through 17 years of age are shown in Tables 9 and 10.


Clinical Trials Experience With Prevnar 13 in Adults ≥ 50 Years of Age
The safety of Prevnar 13 was assessed in 6 clinical studies conducted in the US and Europe which included 6,198 adults (5,667 received Prevnar 13) ranging in age from 50 through 95 years.
The 5,667 Prevnar 13 recipients included 2,616 adults who were aged 50 through 64 years and 3,051 adults aged 65 years and older. Of the 5,667 Prevnar 13 recipients, 3,751 adults had not previously received PPSV23 ("PPSV23 unvaccinated") and 1,916 adults were previously vaccinated ("PPSV23 previously vaccinated") with PPSV23 at least 3 years prior to enrollment.
Two of the 6 clinical studies supporting safety were randomized comparing the safety and immunogenicity of Prevnar 13 with PPSV23 as a single dose in PPSV23 unvaccinated adults aged 50 through 64 years (Study 6) and in adults ≥ 70 years PPSV23 previously vaccinated (≥ 5 years prior to enrollment) (Study 7). One study was randomized comparing the safety and immunogenicity of a single dose of Prevnar 13 compared to a single dose of PPSV23 in PPSV23 unvaccinated adults aged 60 through 64 years (Study 8). One clinical safety study (Study 9) of Prevnar 13, conducted in PPSV23 previously vaccinated (≥ 3 years prior to enrollment) adults aged ≥ 68 years was a single arm study. Two studies, one in the US (Study 10) in adults age 50 through 59 years and the other in Europe (Study 11) in adults aged ≥ 65 years, evaluated the concomitant administration of Prevnar 13 with trivalent inactivated influenza vaccine (Fluarix®, A/H1N1, A/H3N2, and B, Fall 2007/Spring 2008: TIV) in these two age groups in PPSV23 unvaccinated adults.
The total safety population in the 6 studies was 6,198. In 5 of the 6 studies, more females than males were enrolled (50.2% – 61.8%). Across the 6 studies the racial distribution included: > 91% White; 0.2%–7.5% Black or African American; 0%–1.7% Asian; < 1% Native Hawaiian or other Pacific Islander; ≤ 1%, American Indian or Alaskan Native. Ethnicity data were not collected in study 6; in the 5 other studies 0.6%–4.8% were Hispanic or Latino.
In five studies, persons with pre-existing underlying diseases were enrolled if the medical condition was stable (did not require a change in therapy or hospitalization for worsening disease for 12 weeks before receipt of study vaccine) except in study 9 where subjects were enrolled if the medical condition was stable for 6 or more weeks before receipt of study vaccine.
Persons were excluded from study participation due to prior receipt of diphtheria toxoid containing vaccines within 6 months of study vaccine. However, the time of prior receipt of a diphtheria toxoid containing vaccine was not recorded.
Solicited adverse reactions for Prevnar 13 were monitored by subjects recording local adverse reactions and systemic reactions daily using an electronic diary for 14 consecutive days following vaccination. Unsolicited serious and non-serious adverse events were collected for one month after each vaccination. In addition, serious adverse events were collected for an additional 5 months after each vaccination (at the 6-month follow-up phone contact) in all studies except Study 11.
Serious Adverse Events in Adult Clinical Studies
Across the 6 studies, serious adverse events within 1 month of vaccination were reported after an initial study dose in 0.2%–1.4% of 5055 persons vaccinated with Prevnar 13 and in 0.4%–1.7% of 1124 persons vaccinated after an initial study dose of PPSV23. From 1 month to 6 months after an initial study dose, serious adverse events were reported in 1.2%–5.8% of persons vaccinated during the studies with Prevnar 13 and in 2.4%–5.5% of persons vaccinated with PPSV23. One case of erythema multiforme occurred 34 days after receipt of a second dose of Prevnar 13.
Twelve of 5,667 (0.21%) Prevnar 13 recipients and 4 of 1,391 (0.29 %) PPSV23 recipients died. Deaths occurred between day 3 and day 309 after study vaccination with Prevnar 13 or PPSV23. Two of 12 deaths occurred within 30 days of vaccination and both deaths were in subjects > 65 years of age. One death due to cardiac failure occurred 3 days after receiving placebo. This subject had received Prevnar 13 and TIV one month earlier. The other death was due to peritonitis 20 days after receiving Prevnar 13. The reported causes of the 10 remaining deaths occurring greater than 30 days after receiving Prevnar 13 were cardiac disorders (4), neoplasms (4), Mycobacterium avium complex pulmonary infection (1) and septic shock (1).
Solicited Adverse Reactions in Adult Clinical Studies
The incidence and severity of solicited adverse reactions that occurred within 14 days following each dose of Prevnar 13 or PPSV23 administered to adults in 4 studies are shown in Tables 11, 12, 13, and 14. The commonly reported local adverse reactions after Prevnar 13 vaccination in PPSV23 unvaccinated and PPSV23 previously vaccinated adults were redness, swelling and pain at the injection site, or limitation of arm movement (Tables 11 and 12). The commonly reported systemic adverse reactions in PPSV23 unvaccinated and PPSV23 previously vaccinated adults were fatigue, headache, chills, rash, decreased appetite, or muscle pain and joint pain (Tables 13 and 14).




Solicited Adverse Reactions in Adult Clinical Studies of Concomitant Administration of Prevnar 13 and TIV (Fluarix)
The safety of concomitant administration of Prevnar 13 with TIV was assessed in 2 studies in PPSV23 unvaccinated adults aged 50 through 59 years (Study 10) and aged ≥ 65 years (Study 11).
Frequencies of local reactions within 14 days postvaccination in adults aged 50 through 59 years and in adults aged ≥ 65 years were similar after Prevnar 13 was administered with TIV compared to Prevnar 13 administered alone, with the exception of mild redness at the injection site, which was increased when Prevnar 13 was administered concomitantly with TIV and mild limitation of arm movement, which was increased when Prevnar 13 was administered alone.
An increase in some solicited systemic reactions within 14 days postvaccination was noted when Prevnar 13 was administered concomitantly with TIV compared with TIV given alone (headache, chills, rash, decreased appetite, muscle and joint pain) or with Prevnar 13 given alone (fatigue, headache, chills, decreased appetite, and joint pain).
Clinical Trials Experience With Prevnar in Infants and Toddlers
The safety experience with Prevnar is relevant to Prevnar 13 because the two vaccines share common components.
Generally, the adverse reactions reported in clinical trials with Prevnar 13 were also reported in clinical trials with Prevnar.
Overall, the safety of Prevnar was evaluated in a total of five clinical studies in the U.S. in which 18,168 infants and children received a total of 58,699 doses of vaccine at 2, 4, 6, and 12–15 months of age.
Adverse events reported in clinical trials with Prevnar that occurred within 3 days of vaccination in infants and toddlers and resulted in emergency room visits or hospitalizations, but were not presented in Section 6.1 as adverse reactions for Prevnar 13 are listed below:
- Bronchiolitis
- UTI
- Acute gastroenteritis
- Asthma
- Aspiration
- Breath holding
- Influenza
- Inguinal hernia repair
- Viral syndrome
- URI
- Croup
- Thrush
- Wheezing
- Choking
- Conjunctivitis
- Pharyngitis
- Colic
- Colitis
- Congestive heart failure
- Roseola
- Sepsis
Postmarketing Experience
Post-marketing Experience With Prevnar 13 in Infants and Toddlers
The following adverse events have been reported through passive surveillance since market introduction of Prevnar 13. Because these events are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the vaccine. The following adverse events were included based on one or more of the following factors: severity, frequency of reporting, or strength of evidence for a causal relationship to Prevnar 13 vaccine.
- Administration site conditions: Vaccination-site dermatitis, vaccination-site pruritus, vaccination-site urticaria
- Blood and lymphatic system disorders: Lymphadenopathy localized to the region of the injection site
- Cardiac Disorders: Cyanosis
- Immune system disorders: Anaphylactic/anaphylactoid reaction including shock
- Nervous System Disorders: Hypotonia
- Skin and subcutaneous tissue disorders: Angioneurotic edema, erythema multiforme
- Respiratory: Apnea
- Vascular Disorders: Pallor
Post-marketing Experience With Prevnar in Infants and Toddlers
There are no adverse reactions reported for Prevnar through passive post-marketing surveillance that were not already reported for Prevnar 13.
The safety of Prevnar given concomitantly with other vaccines as part of routine care was assessed in a three-year observational study performed at Northern California Kaiser Permanente (NCKP) in which 65,927 children received three doses of Prevnar in the first year of life. Primary safety outcomes analyses included an evaluation of pre-defined adverse events occurring in temporal relationship to immunization. Rates of adverse events occurring within various time periods post-vaccination (e.g., 0–2, 0–7, 0–14, and 0–30 days) were compared to the rates of those events occurring within a control time window (i.e., 31–60 days). Secondary safety outcomes analyses included comparisons to a historical control population of infants (1995–1996, N=40,223) prior to the introduction of Prevnar. In addition, the study included extended follow-up of subjects originally enrolled in the NCKP efficacy trial (N=37,866).
The primary safety outcomes analyses did not demonstrate a consistently elevated risk of healthcare utilization for croup, gastroenteritis, allergic reactions, seizures, wheezing diagnoses, or breath-holding across doses, healthcare settings, or multiple time windows. As in prelicensure trials, fever was associated with Prevnar administration. In analyses of secondary safety outcomes, the adjusted relative risk of hospitalization for reactive airways disease was 1.23 (95% CI: 1.11, 1.35). Potential confounders, such as differences in concomitantly administered vaccines, yearly variation in respiratory infections, or secular trends in reactive airways disease incidence, could not be controlled. Extended follow-up of subjects originally enrolled in the NCKP efficacy trial revealed no increased risk of reactive airways disease among Prevnar recipients. In general, the study results support the previously described safety profile of Prevnar.
Drug Interactions
Concomitant Immunizations
In clinical trials with infants and toddlers, Prevnar 13 was administered concomitantly with the following US licensed vaccines: Pediarix [Diphtheria and Tetanus Toxoids and Acellular Pertussis Adsorbed, Hepatitis B (Recombinant) and Inactivated Poliovirus Vaccine Combined] (DTaP-HBV-IPV) and ActHIB [Haemophilus b Conjugate Vaccine (Tetanus Toxoid Conjugate)] (PRP-T) for the first three doses and with PedvaxHIB [Haemophilus b Conjugate Vaccine (Meningococcal Protein Conjugate)] (PRP-OMP), M-M-R II [Measles, Mumps, Rubella Virus Vaccine Live] (MMR) and Varivax [Varicella Virus Vaccine Live], or ProQuad [Measles, Mumps, Rubella and Varicella Virus Vaccine Live] (MMRV) and VAQTA [Hepatitis A vaccine, Inactivated] (HepA) for dose 4.
In children and adolescents, data are insufficient to assess the concomitant administration of Prevnar 13 with Human Papillomavirus Vaccine (HPV), Meningococcal Conjugate Vaccine (MCV4) and Tetanus Toxoid, Reduced Diphtheria Toxoid and Acellular Pertussis Vaccine, Adsorbed (Tdap).
In adults, Prevnar 13 was administered concomitantly with US licensed Fluarix (TIV) for the 2007/2008 influenza season [see Clinical Studies (14.3) and Adverse Reactions (6.2)]. There are no data on the concomitant administration of Prevnar 13 with diphtheria toxoid-containing vaccines and other vaccines licensed for use in adults 50 years of age and older.
When Prevnar 13 is administered at the same time as another injectable vaccine(s), the vaccines should always be administered with different syringes and given at different injection sites. Do not mix Prevnar 13 with other vaccines/products in the same syringe.
Immunosuppressive Therapies
Individuals with impaired immune responsiveness due to the use of immunosuppressive therapy (including irradiation, corticosteroids, antimetabolites, alkylating agents, and cytotoxic agents) may not respond optimally to active immunization.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B
A developmental and reproductive toxicity study has been performed in female rabbits at a dose approximately 20 times the human dose (on mg/kg basis) and revealed no evidence of impaired female fertility or harm to the fetus due to Prevnar 13. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this vaccine should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pneumococcal Vaccine 13-Valent in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Pneumococcal Vaccine 13-Valent during labor and delivery.
Nursing Mothers
It is not known whether this vaccine is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Prevnar 13 is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of Prevnar 13 in children below the age of 6 weeks have not been established.
Geriatic Use
- Of the total number of Prevnar 13 recipients (N=5,667), 3,051/5,667 or 53.8% were 65 years and older and 1,266/5,667 or 22.3% were 75 years and older.
- Antibody responses to Prevnar 13 were lower in persons ≥ 65 years of age compared to antibody responses in persons 50 through 59 years of age.
- No overall differences in safety outcomes were observed in persons aged ≥ 65 years as compared to persons 50 through 59 years of age.
Gender
There is no FDA guidance on the use of Pneumococcal Vaccine 13-Valent with respect to specific gender populations.
Race
There is no FDA guidance on the use of Pneumococcal Vaccine 13-Valent with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Pneumococcal Vaccine 13-Valent in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Pneumococcal Vaccine 13-Valent in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Pneumococcal Vaccine 13-Valent in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Pneumococcal Vaccine 13-Valent in patients who are immunocompromised.
High Risk Populations
Individuals with the diseases or conditions listed below are at increased risk of pneumococcal disease. Immunogenicity and safety data in these populations are limited.
Infants Born Prematurely
Immune responses elicited by Prevnar 13 administered on a US schedule to preterm infants have not been studied. When preterm infants (< 37 weeks gestational age, N=100) were administered 4 doses of Prevnar 13 on a non-US schedule, the serotype-specific IgG antibody responses after the third and fourth dose were lower compared to responses among term infants (≥ 37 weeks gestational age, N=100) for some serotypes; the effectiveness of Prevnar 13 in preterm infants cannot be established from this study.
Children with Sickle Cell Disease
In an open-label, single-arm, descriptive study, 2 doses of Prevnar 13 were administered 6 months apart to children ≥ 6 to < 18 years of age with sickle cell disease who previously received PPSV23 at least 6 months prior to enrollment. Children with a prior history of pneumococcal conjugate vaccination were excluded. For all vaccine serotypes, anti-pneumococcal opsonophagocytic activity (OPA) geometric mean antibody titers (GMTs) were higher after the first dose compared to pre-vaccination (N=95–131); OPA GMTs following the first and second dose were comparable. The effectiveness of Prevnar 13 in this specific population has not been established.
Adults with HIV Infection
In an open-label, single-arm, descriptive study, 3 doses of Prevnar 13 were administered 6 months apart to HIV-infected adults ≥ 50 years of age (median age 55 years), with CD4 counts ≥ 200 cells/µL and serum HIV RNA titer < 50,000 copies/mL. All subjects had been vaccinated previously with PPSV23 at least 6 months prior to enrollment. For all vaccine serotypes anti-pneumococcal OPA GMTs were higher after the first dose compared to pre-vaccination (N=94–108); OPA GMTs following the first, second and third dose were generally comparable. The effectiveness of Prevnar 13 in this specific population has not been established.
Administration and Monitoring
Administration
Intramuscular
Monitoring
There is limited information regarding Pneumococcal Vaccine 13-Valent Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Pneumococcal Vaccine 13-Valent and IV administrations.
Overdosage
There is limited information regarding Pneumococcal Vaccine 13-Valent overdosage. If you suspect drug poisoning or overdose, please contact the National Poison Help hotline (1-800-222-1222) immediately.
Pharmacology
Pneumococcal polysaccharide vaccine
| |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | J07 |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | ? |
Mechanism of Action
Prevnar 13, comprised of pneumococcal polysaccharides conjugated to a carrier protein (CRM197), elicits a T-cell dependent immune response. Protein carrier-specific T-cells provide the signals needed for maturation of the B-cell response.
Nonclinical and clinical data support opsonophagocytic activity, as measured by opsonophagocytic activity (OPA) antibody assay, as a contributor to protection against pneumococcal disease. The OPA antibody assay provides an in vitro measurement of the ability of serum antibodies to eliminate pneumococci by promoting complement-mediated phagocytosis and is believed to reflect relevant in vivo mechanisms of protection against pneumococcal disease. OPA antibody titers are expressed as the reciprocal of the highest serum dilution that reduces survival of the pneumococci by at least 50%.
In infants that have received Prevnar 13, opsonophagocytic activity correlates well with serotype specific anti-capsular polysaccharide IgG levels as measured by ELISA. A serum anti-capsular polysaccharide antibody concentration of 0.35 µg/mL as measured by ELISA one month after the third dose as a single antibody reference concentration was used to estimate the effectiveness of Prevnar 13 against invasive pneumococcal disease (IPD) in infants and children. The assay used for this determination is a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity. The single antibody reference value was based on pooled efficacy estimates from three placebo-controlled IPD efficacy trials with either Prevnar or the investigational 9-valent CRM197 conjugate pneumococcal polysaccharide vaccine. This reference concentration is only applicable on a population basis and cannot be used to predict protection against IPD on an individual basis. Functional antibodies elicited by the vaccine (as measured by a dribble opsonophagocytic activity [dOPA] antibody assay) were also evaluated in infants.
In adults, an antipolysaccharide binding antibody IgG level to predict protection against invasive pneumococcal disease or non-bacteremic pneumonia has not been defined. Noninferiority trials for Prevnar 13 were designed to show that functional OPA antibody responses (as measured by a microcolony OPA [mcOPA] antibody assay) for the Prevnar 13 serotypes are non-inferior and for some serotypes superior to the common serotypes in the currently licensed pneumococcal polysaccharide vaccine (PPSV23). OPA antibody titers measured in the mcOPA antibody assay cannot be compared directly to titers measured in the dOPA antibody assay.
Structure
Prevnar 13, Pneumococcal 13-valent Conjugate Vaccine (Diphtheria CRM197 Protein) is a sterile suspension of saccharides of the capsular antigens of Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14, 18C, 19A, 19F, and 23F, individually linked to non-toxic diphtheria CRM197 protein. Each serotype is grown in soy peptone broth. The individual polysaccharides are purified through centrifugation, precipitation, ultrafiltration, and column chromatography. The polysaccharides are chemically activated to make saccharides, which are directly conjugated by reductive amination to the protein carrier CRM197, to form the glycoconjugate. CRM197 is a nontoxic variant of diphtheria toxin isolated from cultures of Corynebacterium diphtheriae strain C7 (β197) grown in a casamino acids and yeast extract-based medium. CRM197 is purified through ultrafiltration, ammonium sulfate precipitation, and ion-exchange chromatography. The individual glycoconjugates are purified by ultrafiltration and column chromatography and analyzed for saccharide to protein ratios, molecular size, free saccharide, and free protein.
The individual glycoconjugates are compounded to formulate Prevnar 13. Potency of the formulated vaccine is determined by quantification of each of the saccharide antigens and by the saccharide to protein ratios in the individual glycoconjugates. Each 0.5 mL dose of the vaccine is formulated to contain approximately 2.2 µg of each of Streptococcus pneumoniae serotypes 1, 3, 4, 5, 6A, 7F, 9V, 14, 18C, 19A, 19F, 23F saccharides, 4.4 µg of 6B saccharides, 34 µg CRM197 carrier protein, 100 µg polysorbate 80, 295 µg succinate buffer and 125 µg aluminum as aluminum phosphate adjuvant.
The tip cap and rubber plunger of the prefilled syringe are not made with natural rubber latex.
Pharmacodynamics
There is limited information regarding Pneumococcal Vaccine 13-Valent Pharmacodynamics in the drug label.
Pharmacokinetics
There is limited information regarding Pneumococcal Vaccine 13-Valent Pharmacokinetics in the drug label.
Nonclinical Toxicology
There is limited information regarding Pneumococcal Vaccine 13-Valent Nonclinical Toxicology in the drug label.
Clinical Studies
=Prevnar Efficacy Data
Invasive Pneumococcal Disease (IPD)
Prevnar was licensed in the US for infants and children in 2000, following a randomized, double-blind clinical trial in a multiethnic population at Northern California Kaiser Permanente (NCKP) from October 1995 through August 20, 1998, in which 37,816 infants were randomized to receive either Prevnar or a control vaccine (an investigational meningococcal group C conjugate vaccine [MnCC]) at 2, 4, 6, and 12–15 months of age. In this study, the efficacy of Prevnar against invasive disease due to S. pneumoniae in cases accrued during this period was 100% in both the per-protocol and intent-to-treat analyses (95% CI: 75.4%–100% and 81.7%–100%, respectively). Data accumulated through an extended follow-up period to April 20, 1999, resulted in similar efficacy estimates of 97.4% in the per-protocol analysis and 93.9% in the intent-to-treat analysis (95% CI: 82.7% – 99.9% and 79.6% – 98.5%, respectively).
Acute Otitis Media (AOM)
The efficacy of Prevnar against otitis media was assessed in two clinical trials: a trial in Finnish infants at the National Public Health Institute and the efficacy trial in US infants at Northern California Kaiser Permanente (NCKP).
The Finnish Otitis Media (FinOM) trial was a randomized, double-blind trial in which 1,662 infants were equally randomized to receive either Prevnar or a control vaccine Recombivax HB (Hepatitis B vaccine (Recombinant) [Hep B]) at 2, 4, 6, and 12–15 months of age. In this study, conducted between December 1995 and March 1999, parents of study participants were asked to bring their children to the study clinics if the child had respiratory infections or symptoms suggesting acute otitis media (AOM). If AOM was diagnosed, tympanocentesis was performed, and the middle-ear fluid was cultured. If S. pneumoniae was isolated, serotyping was performed; the primary endpoint was efficacy against AOM episodes caused by vaccine serotypes in the per-protocol population. In the NCKP trial, the efficacy of Prevnar against otitis media was assessed from the beginning of the trial in October 1995 through April 1998. The otitis media analysis included 34,146 infants randomized to receive either Prevnar (N=17,070), or the control vaccine (N=17,076), at 2, 4, 6, and 12–15 months of age. In this trial, no routine tympanocentesis was performed, and no standard definition of otitis media was used by study physicians. The primary otitis media endpoint was efficacy against all otitis media episodes in the per-protocol population.
The vaccine efficacy against AOM episodes due to vaccine serotypes assessed in the Finnish trial, was 57% (95% CI: 44%–67%) in the per-protocol population and 54% (95% CI: 41%–64%) in the intent-to-treat population. The vaccine efficacy against AOM episodes due to vaccine-related serotypes (6A, 9N, 18B, 19A, 23A), also assessed in the Finnish trial, was 51% (95% CI: 27, 67) in the per-protocol population and 44% (95% CI: 20, 62) in the intent-to-treat population. There was a nonsignificant increase in AOM episodes caused by serotypes unrelated to the vaccine in the per-protocol population, compared to children who received the control vaccine, suggesting that children who received Prevnar appeared to be at increased risk of otitis media due to pneumococcal serotypes not represented in the vaccine. However, vaccination with Prevnar reduced pneumococcal otitis media episodes overall. In the NCKP trial, in which the endpoint was all otitis media episodes regardless of etiology, vaccine efficacy was 7% (95% CI: 4%–10%) and 6% (95% CI: 4%–9%), respectively, in the per-protocol and intent-to-treat analyses. Several other otitis media endpoints were also assessed in the two trials.
Recurrent AOM, defined as 3 episodes in 6 months or 4 episodes in 12 months, was reduced by 9% in both the per-protocol and intent-to-treat populations (95% CI: 3%–15% in per-protocol and 95% CI: 4%–14% in intent-to-treat) in the NCKP trial; a similar trend was observed in the Finnish trial. The NCKP trial also demonstrated a 20% reduction (95% CI: 2, 35) in the placement of tympanostomy tubes in the per-protocol population and a 21% reduction (95% CI: 4, 34) in the intent-to-treat population. Data from the NCKP trial accumulated through an extended follow-up period to April 20, 1999, in which a total of 37,866 children were included (18,925 in Prevnar group and 18,941 in MnCC control group), resulted in similar otitis media efficacy estimates for all endpoints.
Prevnar 13 Clinical Trials in Children 6 Weeks Through 17 Years of Age
Infants and Children 6 Weeks Through 17 Months of Age
Prevnar 13 effectiveness against invasive pneumococcal disease was inferred from comparative studies to a US licensed 7-valent pneumococcal conjugate vaccine, Prevnar, in which Prevnar 13 elicited antipolysaccharide binding and functional OPA antibodies, as measured by ELISA and dOPA assays, respectively. These studies were designed to evaluate immunologic noninferiority of Prevnar 13 to Prevnar. Clinical trials have been conducted in the US using a 2, 4, 6, and 12–15 month schedule.
The US noninferiority study (Study 2) was a randomized, double-blind, active-controlled trial in which 2 month-old infants were randomly assigned to receive either Prevnar 13 or Prevnar in a 1:1 ratio. The two vaccine groups were well balanced with respect to race, ethnicity, and age and weight at enrollment. Most subjects were White (69.1%), 19.6% were Black or African-American, and 2.4% were Asian; 82.1% of subjects were non-Hispanic and non-Latino and 17.3% were Hispanic or Latino. Overall, 54.0% of subjects were male infants.
In Study 2, immune responses were compared in subjects receiving either Prevnar 13 or Prevnar using a set of noninferiority criteria. Co-primary endpoints included the percentage of subjects with serum pneumococcal anti-capsular polysaccharide IgG ≥ 0.35 µg/mL measured one month after the third dose and serum pneumococcal anti-capsular polysaccharide IgG geometric mean concentrations (GMCs) one month after the fourth dose. The assay used for this determination was a standardized ELISA involving pre-absorption of the test sera with pneumococcal C-polysaccharide and serotype 22F polysaccharide to reduce non-specific background reactivity. Responses to the 7 common serotypes in Prevnar 13 and Prevnar recipients were compared directly. Responses to the 6 additional serotypes in Prevnar 13 recipients were each compared to the lowest response observed among the Prevnar serotypes in Prevnar recipients.
Pneumococcal Immune Responses Following Three Doses
In Study 2, the noninferiority criterion for the proportion of subjects with pneumococcal anti-capsular polysaccharide IgG antibody concentrations ≥ 0.35 µg/mL one month after the third dose was met for 10 of the 13 serotypes. The exceptions were serotypes 6B, 9V, and 3. Although the response to serotypes 6B and 9V did not meet the pre-specified noninferiority criterion, the differences were marginal.
The percentage of infants achieving pneumococcal anti-capsular polysaccharide IgG antibody concentrations ≥ 0.35 µg/mL one month after the third dose is shown below (Table 15).

Functional dOPA antibody responses were elicited for all 13 serotypes, as shown in Table 16.

Pneumococcal Immune Responses Following Four Doses
In Study 2, post-dose 4 antibody concentrations were higher for all 13 serotypes than those achieved after the third dose. The noninferiority criterion for pneumococcal anti-capsular polysaccharide GMCs after 4 doses was met for 12 of the 13 pneumococcal serotypes. The noninferiority criterion was not met for the response to serotype 3 (Table 17).

Following the fourth dose, the functional dOPA antibody response for each serotype was quantitatively greater than the response following the third dose (see Table 18).

Previously Unvaccinated Older Infants and Children 7 Months Through 5 Years of Age
In an open-label descriptive study of Prevnar 13 in Poland (Study 4), children 7 months through 11 months of age, 12 months through 23 months of age and 24 months through 5 years of age (prior to the 6th birthday) who were naïve to pneumococcal conjugate vaccine, were given 3, 2 or 1 dose of Prevnar 13 respectively, according to the age-appropriate schedules in Table 2. Serum IgG concentrations were measured one month after the final dose in each age group and the data are shown in Table 19.

Children 15 Months Through 59 Months of Age Previously Vaccinated with Prevnar
In an open-label descriptive study in the US (Study 5), children 15 months through 59 months previously vaccinated with 3 or 4 doses of Prevnar, received 2 doses of Prevnar 13 (children > 15 through 23 months of age) or 1 dose of Prevnar 13 (children 24 months through 59 months of age). The data following one dose of Prevnar 13 in children 24 months through 59 months of age are shown in Table 20.

Children 5 Through 17 Years of Age
In a US study (Study 5), a single dose of Prevnar 13 was administered to children 5 through 9 years of age, who were previously vaccinated with at least one dose of Prevnar, and to pneumococcal vaccine-naïve children 10 through 17 years of age.
In children 5 through 9 years of age, serotype-specific IgG concentrations measured 1 month after vaccination were noninferior (i.e., the lower limit of the 2-sided 95% CI for the GMR of >0.5) to the corresponding IgG concentrations in toddlers (Study 3) 1 month after a fourth pneumococcal vaccination (after the 4th dose of Prevnar for the 7 common serotypes and after the 4th dose of Prevnar 13 for the 6 additional serotypes) as shown in Tables 21 and 22 respectively.


In children 10 through 17 years of age OPA GMTs, as measured by the mcOPA assay, 1 month after vaccination were noninferior (i.e., the lower limit of the 2-sided 95% CI for the GMR of >0.5) to mcOPA GMTs in the 5 through 9 year old group for 12 of 13 serotypes (except for serotype 3), as shown in Table 23.

Prevnar 13 Immunogenicity Clinical Trials in Adults
Five phase 3 clinical trials were conducted in the US and Europe evaluating the immunogenicity of Prevnar 13 in different adult age groups, in individuals who were either not previously vaccinated with PPSV23 (PPSV23 unvaccinated) or who had received one dose of PPSV23 (PPSV23 previously vaccinated).
Each study included healthy adults and immunocompetent adults with stable underlying conditions including chronic cardiovascular disease, chronic pulmonary disease, renal disorders, diabetes mellitus, chronic liver disease, and medical risk conditions and behaviors (e.g., alcoholism and smoking) that are known to increase the risk of serious pneumococcal pneumonia and invasive pneumococcal disease. A stable medical condition was defined as a medical condition not requiring significant change in therapy (i.e., change to new therapy category due to worsening disease) or hospitalization for worsening disease 12 weeks before receipt of the study vaccine.
Immune responses elicited by Prevnar 13 and PPSV23 were measured by a mcOPA antibody assay for the thirteen pneumococcal serotypes contained in Prevnar 13. Serotype-specific mcOPA antibody GMTs measured 1 month after each vaccination were calculated. For the 12 serotypes in common to both vaccines, noninferiority between vaccines was met if the lower limit of the 2-sided 95% confidence interval (CI) of the GMT ratio (Prevnar 13/PPSV23) was greater than 0.5.
The response to the additional serotype 6A, which is contained in Prevnar 13 but not in PPSV23, was assessed by demonstration of a ≥ 4-fold increase in the anti-6A mcOPA antibody titer above preimmunization levels. A statistically significantly greater response for Prevnar 13 was defined, for the difference in percentages (Prevnar 13 minus PPSV23) of adults achieving a ≥ 4-fold increase in anti-6A mcOPA antibody titer, as the lower limit of the 2-sided 95% CI greater than zero. For comparison of mcOPA antibody GMTs, a statistically greater response for serotype 6A was defined as the lower limit of the 2-sided 95% CI of the GMT ratio (Prevnar 13/PPSV23) greater than 2.
Of the five phase 3 clinical trials, 2 noninferiority trials were conducted in which the immune responses to Prevnar 13 were compared with the immune responses to PPSV23; one in PPSV23 unvaccinated adults aged 50 through 64 years (Study 6), and one in PPSV23 prevaccinated adults aged ≥ 70 years (Study 7). A third study compared immune responses of Prevnar 13 as a single dose compared to the response to Prevnar 13 administered one year after a dose of PPSV23 in adults aged 60 through 64 years who were PPSV23 unvaccinated at enrollment (Study 8). The study also compared immune responses of PPSV23 as a single dose compared to the responses to PPSV23 administered one year after a dose of Prevnar 13. Two studies assessed the concomitant administration of Prevnar 13 with seasonal inactivated Fluarix (TIV) in the US (Study 10) and Europe (Study 11).
Clinical Trials Conducted in PPSV23 Unvaccinated Adults
In an active-controlled modified1 double-blind clinical trial (Study 6) of Prevnar 13 in the US, PPSV23 unvaccinated adults aged 60 through 64 years were randomly assigned (1:1) to receive Prevnar 13 or PPSV23. In addition, adults aged 50 through 59 years were enrolled and received one dose of Prevnar 13 (open-label).
In adults aged 60 through 64 years, the mcOPA antibody GMTs elicited by Prevnar 13 were noninferior to those elicited by PPSV23 for the 12 serotypes in common to both vaccines (see Table 24). In addition, the lower limit of the 95% confidence interval for the mcOPA antibody GMT ratio (Prevnar 13/PPSV23) was greater than 1 for 8 of the serotypes in common.
For serotype 6A, which is unique to Prevnar 13, the proportions of subjects with a ≥ 4-fold increase after Prevnar 13 (88.5%) was statistically significantly greater than after PPSV23 (49.3%) in PPSV23-unvaccinated adults aged 60 through 64 years. OPA antibody GMTs for serotype 6A were statistically significantly greater after Prevnar 13 compared with after PPSV23 (see Table 24).
The mcOPA antibody GMTs elicited by Prevnar 13 in adults aged 50 through 59 years were noninferior to the corresponding mcOPA antibody GMTs elicited by Prevnar 13 in adults aged 60 through 64 years for all 13 serotypes (see Table 24).

Clinical Trials Conducted in PPSV23 Previously Vaccinated Adults
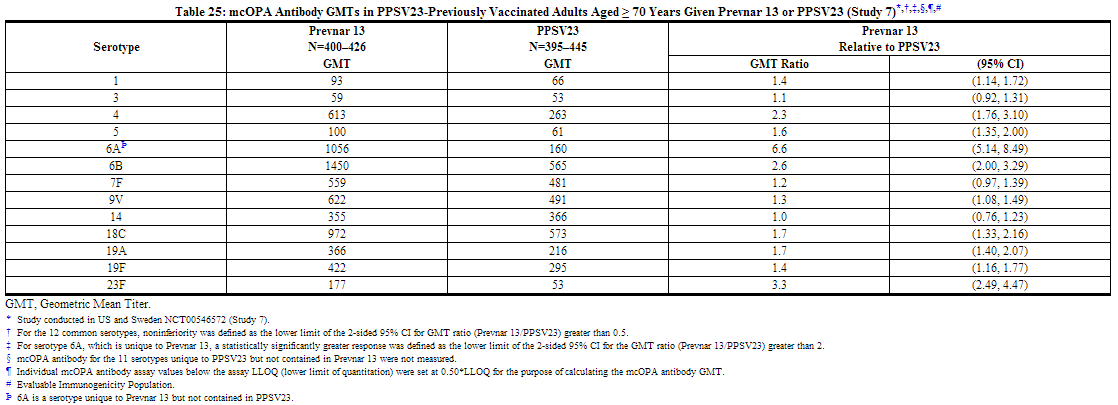
In a phase 3 active-controlled, modified double-blind clinical trial (Study 7) of Prevnar 13 in the US and Sweden, PPSV23 prevaccinated adults aged ≥ 70 years who had received one dose of PPSV23 ≥ 5 years prior were randomly assigned (1:1) to receive either Prevnar 13 or PPSV23.
The mcOPA antibody GMTs elicited by Prevnar 13 were noninferior to those elicited by PPSV23 for the 12 serotypes in common, when Prevnar 13 or PPSV23 were administered at a minimum of 5 years after a prior dose of PPSV23. In addition, the lower limit of the 95% confidence interval for the mcOPA antibody GMT ratio (Prevnar 13/PPSV23) was greater than 1 for 9 of the serotypes in common.
For serotype 6A, which is unique to Prevnar 13, the proportion of subjects with a 4-fold increase in mcOPA antibody titers after Prevnar 13 (71.1%) was statistically significantly greater than after PPSV23 (27.3%) in PPSV23-prevaccinated adults aged ≥ 70 years. mcOPA antibody GMTs for serotype 6A were statistically significantly greater after Prevnar 13 compared with after PPSV23.
This clinical trial demonstrated that in adults aged ≥ 70 years and prevaccinated with PPSV23 ≥ 5 years prior, vaccination with Prevnar 13 elicited noninferior immune responses as compared with re-vaccination with PPSV23 (see Table 25).
Clinical Trial of Sequential Vaccination of Prevnar 13 and PPSV23 in PPSV23 Unvaccinated Adults
In a randomized clinical trial conducted in PPSV23-unvaccinated adults 60 through 64 years of age (Study 8), 223 persons received PPSV23 followed by Prevnar 13 one year later (PPSV23/Prevnar 13), and 478 received only Prevnar 13. mcOPA antibody titers were measured 1 month after vaccination with Prevnar 13 and are shown in Table 26. mcOPA antibody GMTs in those that received Prevnar 13 one year after PPSV23 were diminished when compared to those who received Prevnar 13 alone. Similarly, in exploratory analyses in PPSV23-pre-vaccinated adults ≥70 years of age in Study 7, diminished mcOPA antibody GMTs were observed in those that received Prevnar 13 one year after PPSV23 when compared to those who received Prevnar 13 alone.

No data are available on a dosing interval greater than 1 year. No data are available in response to Prevnar 13 given one year after PPSV23 in previously unvaccinated persons.
Also in Study 8, 266 persons received Prevnar 13 followed by PPSV23 one year later (Prevnar 13/PPSV23). mcOPA antibody GMTs following PPSV23 administered one year after Prevnar 13 (Prevnar 13/PPSV23) were noninferior to those following a single dose of PPSV23 (N=237) for the 12 common serotypes [the lower limit of the 95% CI for the GMT ratio [Prevnar 13/PPSV23 relative to PPSV23] was > 0.5] (see Table 27). In Study 6, which was conducted in PPSV23-unvaccinated adults 60 through 64 years of age, 108 persons received PPSV23 3.5 to 4 years after Prevnar 13 (Prevnar 13/PPSV23) and 414 received a single dose of PPSV23. Higher serotype-specific mcOPA antibody GMT ratios [(Prevnar 13/PPSV23) / PPSV23] were generally observed compared to the one year dosing interval in Study 8.

Concomitant Vaccine Administration
Infants and Toddlers
The concomitant administration of routine US infant vaccines [see Drug Interactions (7.1)] with Prevnar 13 was evaluated in two studies: Study 2 [see Clinical Studies (14.2)], Pneumococcal Immune Responses Following Three Doses] and the US lot consistency study (Study 3). In Study 3, subjects were randomly assigned to receive one of 3 lots of Prevnar 13 or Prevnar in a 2:2:2:1 ratio. The total number of infants vaccinated was 663 (Study 2) and 1699 (Study 3). Immune responses to concomitant vaccine antigens were compared in infants receiving Prevnar and Prevnar 13. Responses to diphtheria toxoid, tetanus toxoid, pertussis, polio types 1, 2, and 3, hepatitis B, PRP-T, PRP-OMP, measles, and varicella antigens in Prevnar 13 recipients were similar to those in Prevnar recipients. Based on limited data, responses to mumps and rubella antigens in Prevnar 13 recipients were similar to those in Prevnar recipients.
Adults
Two randomized, double-blind clinical trials evaluated the immunogenicity of Prevnar 13 given with inactivated TIV (Fall 2007/ Spring 2008 Fluarix, A/H1N1, A/H3N2, and B strains) in PPSV23 unvaccinated adults aged 50 through 59 years (Study 10, conducted in the U.S.) and in adults ≥ 65 years (Study 11, conducted in Europe).
In each clinical trial one group received Prevnar 13 and TIV concurrently, followed approximately one month later by placebo. The other group received TIV and placebo concurrently, followed approximately one month later by Prevnar 13.
Antibody responses elicited by TIV were measured by hemagglutination inhibition assay (HAI) one month after TIV vaccination. The proportion of subjects achieving a ≥ 4-fold increase in HAI titer (responder) for each TIV strain was evaluated 1 month after vaccination. Noninferiority was demonstrated for each TIV vaccine antigen if the lower limit of the 95% CI for the difference in proportions of responders between the two groups [concomitant minus (TIV+Placebo)] was greater than -10%.
In subjects 50 through 59 years of age, noninferiority was demonstrated for each of the 3 TIV strains after Prevnar 13 given concomitantly with TIV compared with TIV given alone.
In subjects ≥ 65 years of age, noninferiority was demonstrated for A/H1N1 and B-strains, but not for A/H3N2, which had a lower limit of the 95% CI of -10.4%.
The studies also assessed the antibody responses of Prevnar 13 when Prevnar 13 was given concomitantly with TIV compared with Prevnar 13 given alone. The antipolysaccharide binding antibody responses (IgG) were measured by ELISA IgG one month after Prevnar 13 vaccination in a subset of subjects. Noninferiority was demonstrated if the lower limit of the 2-sided, 95% CI for the IgG GMC ratios (Prevnar 13+ TIV relative to Prevnar 13 alone) was > 0.5. In a post hoc analysis, mcOPA antibody response was evaluated using the same criterion.
In subjects 50 through 59 years of age, Prevnar 13 IgG antibody responses, as measured by ELISA, met noninferiority for all 13 serotypes after Prevnar 13 was given concomitantly with TIV compared to Prevnar 13 given alone, and noninferiority of the mcOPA antibody GMT ratios was observed for 10 of 13 serotypes.
In subjects ≥ 65 years of age, Prevnar 13 IgG antibody responses, as measured by ELISA, met noninferiority for 12 of 13 serotypes after Prevnar 13 was given concomitantly with TIV compared with Prevnar 13 given alone, and noninferiority of the mcOPA antibody GMT ratios was observed for all of the 13 serotypes.
How Supplied
- Prefilled Syringe, 1 Dose (10 per package) – NDC 0005-1971-02.
- Prefilled Syringe, 1 Dose (1 per package) – NDC 0005-1971-04 (Pfizer Helpful Answers Program).
- Prefilled Syringe, 1 Dose (1 per package) – NDC 0005-1971-05.
Storage
- After shipping, Prevnar 13 may arrive at temperatures between 2°C to 25°C (36°F to 77°F).
- Upon receipt, store refrigerated at 2°C to 8°C (36°F to 46°F).
- Do not freeze. Discard if the vaccine has been frozen.
- The tip cap and rubber plunger of the prefilled syringe are not made with natural rubber latex.
Images
Drug Images
{{#ask: Page Name::Pneumococcal Vaccine 13-Valent |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Pneumococcal Vaccine 13-Valent |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Prior to administration of this vaccine, inform the individual, parent, guardian, or other responsible adult of the following:
- The potential benefits and risks of immunization with Prevnar 13 [see Warnings and Precautions (5) and Adverse Reactions (6)].
- The importance of completing the immunization series unless contraindicated.
- Any suspected adverse reactions should be reported to their healthcare professional.
Provide the Vaccine Information Statements, which are available free of charge at the Centers for Disease Control and Prevention (CDC) website (www.cdc.gov/vaccines).
Precautions with Alcohol
Alcohol-Pneumococcal Vaccine 13-Valent interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Prevnar 13
Look-Alike Drug Names
There is limited information regarding Pneumococcal Vaccine 13-Valent Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Pneumococcal Vaccine 13-Valent |Label Name=Pneumococcal Vaccine 13-Valent Package1.png
}}
{{#subobject:
|Label Page=Pneumococcal Vaccine 13-Valent |Label Name=Pneumococcal Vaccine 13-Valent Package2.png
}}