Pineoblastoma
Template:Pineoblastoma Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Sujit Routray, M.D. [2]
|
WikiDoc Resources for Pineoblastoma |
|
Articles |
|---|
|
Most recent articles on Pineoblastoma Most cited articles on Pineoblastoma |
|
Media |
|
Powerpoint slides on Pineoblastoma |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pineoblastoma at Clinical Trials.gov Trial results on Pineoblastoma Clinical Trials on Pineoblastoma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pineoblastoma NICE Guidance on Pineoblastoma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pineoblastoma Discussion groups on Pineoblastoma Patient Handouts on Pineoblastoma Directions to Hospitals Treating Pineoblastoma Risk calculators and risk factors for Pineoblastoma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pineoblastoma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Synonyms and keywords: Pineoblastomas; Pinealoblastoma; Pinealoblastomas; PB; Pineal parenchymal tumor; Pineal gland tumor; Brain tumor
Overview
Pineoblastoma is a rare, malignant pineal parenchymal tumor. It is a supratentorial midline primitive neuroectodermal tumor. It is considered as a WHO grade IV tumor according to the WHO classification of tumors of the central nervous system.
Pathophysiology
Pathogenesis
Pineoblastoma originates from the neuroectodermal cells. It is the least differentiated pineal gland tumors, with pineocytoma and pineal parenchymal tumour with intermediate differentiation representing better differentiated tumors along the same spectrum.[1]
Associated Conditions
- Pineoblastoma may occur in patients with hereditary uni- or bilateral retinoblastoma.
- When retinoblastoma patients present with pineoblastoma, this is characterized as "trilateral retinoblastoma".[2]
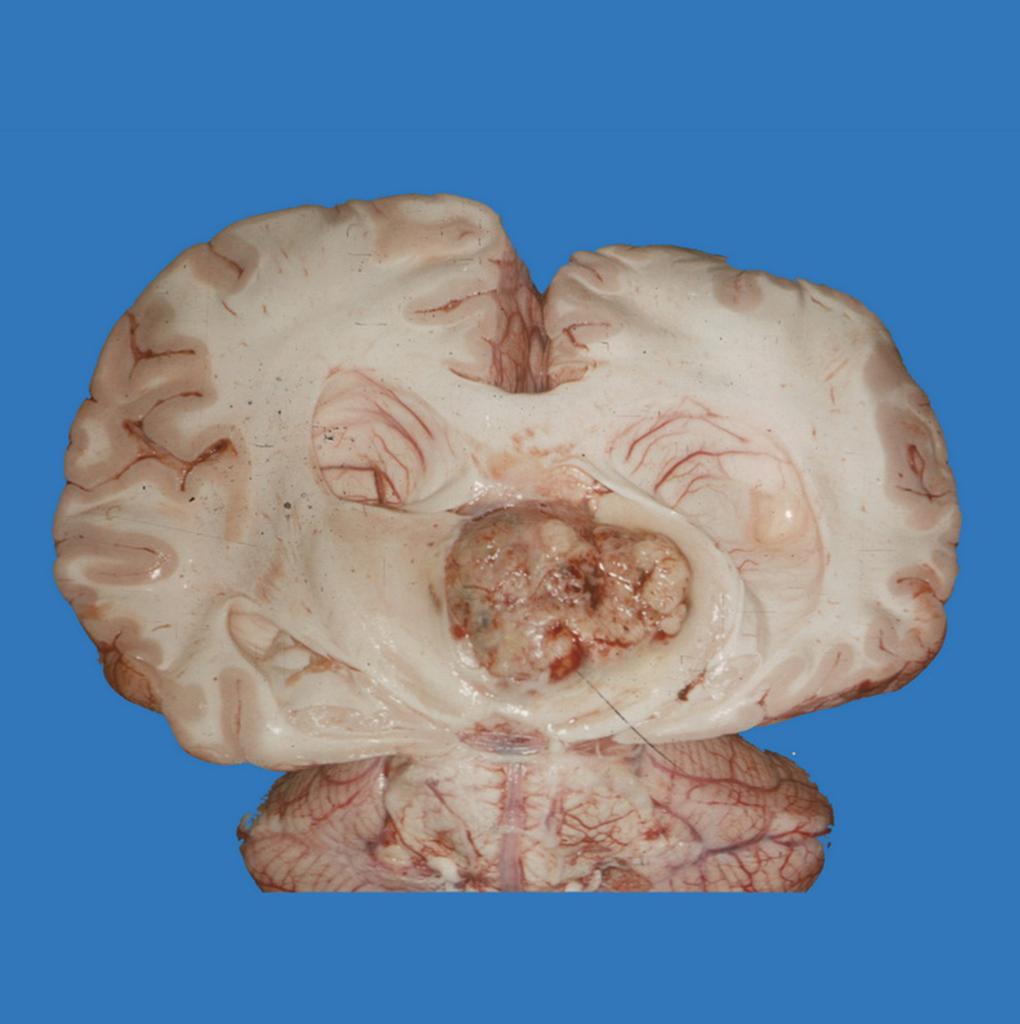
Gross Pathology
On gross pathology, pineoblastoma is characterized by solid, large poorly defined masses.[3]
Microscopic Pathology
On microscopic histopathological analysis, pineoblastoma is characterized by:[1][5][6]
- Hypercellular appearance
- Tightly packed small round blue cells (high nuclear to cytoplasmic ratio)
- Oval and angulated hyperchromatic nuclei with atypia
- Mitoses
- Homer-wright & Flexner-Winterstein rosettes
- Fleurettes
Immunohistochemistry
Pineoblastoma is demonstrated by positivity to tumor markers such as:[6][7]
Differentiating Pineoblastoma from other Diseases
Pineoblastoma must be differentiated from:[8][9]
- Pineocytoma
- Pineal parenchymal tumor with intermediate differentiation
- Papillary tumor of the pineal region
- Pineal germinoma
- Pineal embryonal carcinoma
- Pineal choriocarcinoma
- Pineal yolk sac carcinoma (endodermal sinus tumor)
- Pineal teratoma
- Pineal cyst
- Astrocytoma of the pineal gland
- Meningioma near pineal gland
- Pineal metastasis
- Cavernoma in pineal region
- Aneurysm in pineal region
Epidemiology and Demographics
Prevalence
- Pineoblastoma constitutes approximately 0.1% of the intracranial neoplasms.[10]
- Pineoblastoma together with germ cell tumors are the most common pineal tumors in children.[11]
Age
Pineoblastoma is a disease that tends to affect children and young adults.[12]
Gender
Pineoblastoma affects men and women equally.[13]
Natural History, Complications and Prognosis
Natural History
- Pineoblastoma is the most agressive pineal parenchymal tumor.
- If left untreated, patients with pineoblastoma may progress to develop seizures, obstructive hydrocephalus, local recurrence, and CSF metastasis.[14]
Complications
Common complications of pineoblastoma include:[14][15]
- Obstructive hydrocephalus
- Local recurrence
- CSF metastasis
Prognosis
Prognosis is generally poor, and the 5-year survival rate of patients with pineoblastoma is approximately 58%.[16]
History and Symptoms
History
The clinical presentation of pineoblastoma is mainly from the obstructive hydrocephalus secondary to compression of the tectum of the midbrain and obstruction of the aqueduct.[14]
Symptoms
Physical Examination
- Compression of the superior colliculi can lead to a characteristic upward gaze palsy, known as Parinaud syndrome.
- Common physical examination findings of pineoblastoma include:[10][14]
HEENT
- Bulging soft spots (fontanelles)
- Eyes that are constantly looking down (sunsetting sign)
- Deficiency in upward-gaze
- Pupillary light-near dissociation (pupils respond to near stimuli but not light)
- Convergence-retraction nystagmus
- Papilledema
Neurological
Laboratory Diagnosis
There are no specific laboratory findings for pineocytoma. However, the following findings are of significant
- Both serum and CSF should be assayed for alpha-fetoprotein and beta human chorionic gonadotropin (beta-hCG) to help diagnose a germ cell tumor.
- Immunohistochemistry may be of value in detecting these markers or placental alkaline phosphatase.
CT
- Head CT scan may be diagnostic of pineoblastoma.
- Findings on CT scan suggestive of pineoblastoma include a mass with a solid component that tends to be slightly hyperdense compared to adjacent brain due to high cellularity. Calcification is present that is peripherally disperse or "exploded", similar to pineocytoma.[17]
MRI
- Brain MRI may be diagnostic of pineoblastoma.
- Features on MRI suggestive of pineoblastoma include:[18]
| MRI component | Findings |
|---|---|
|
T1 |
|
|
T2 |
|
|
T1 with gadolinium contrast [T1 C+ (Gd)] |
|
|
Diffuse weighted imaging/Apparent diffusion coefficient [DWI/ADC] |
|
Other Imaging Findings
Other imaging studies for pineoblastoma include magnetic resonance spectroscopy (MR spectroscopy), which demonstrates:[19]
- Elevation of the choline and lipid lactate peaks
- Depression of the neural markers (N-acetyl aspartate (NAA) and creatine (Cr)
- Prominent glutamate and taurine peaks at 3.4 ppm with shot TE signal voxel MR spectroscopy
Other Diagnostic Studies
Stereotactic biopsy
- A direct, visually guided biopsy of the pineal gland mass with open or neuroendoscopic surgery has been preferred due to concerns about injury to the deep cerebral veins.
- An open procedure also allows CSF to be obtained for
- Tumor marker studies
- Permits direct visualization of the third ventricle for staging purposes
- Sllows a third ventriculostomy to be performed for CSF diversion if needed.
- The diagnostic yield of stereotactic biopsy ranges from 94 to 100 percent.
- If the biopsy is nondiagnostic, equivocal, or suggests a benign tumor such as mature teratoma or meningioma, surgery is recommended to establish a definitive diagnosis or to identify focal areas of malignant disease
Treatment
- The predominant therapy for pineoblastoma is surgical resection. Adjunctive chemotherapy and radiation may be required.[11][16]
- The main goal of open surgery on pineoblastoma is the complete tumor removal with minimal morbidity, whenever possible. However, even if gross total excision cannot be achieved, establishment of an accurate diagnosis, maximal cytoreduction, and restoration of the CSF pathway may be achieved.
| Management Options of Penial Gland tumors | |
|---|---|
| CSF diversion |
|
| Surgical resection |
|
| Radiation |
|
| Stereotactic radiosurgery |
|
| Chemotherapy as part of multimodality therapy |
|
- Gross total resection has been associated with improved survival, similar to treatment with craniospinal irradiation and multi-agent chemotherapy.[11]
- Children under the age of 36 months with pineoblastoma should be treated with multi-agent chemotherapy for 12 to 24 months with the goal of delaying radiation past the age of 36 months. Craniospinal irradiation before this age of 3 has been associated with significant cognitive and neuroendocrine sequelae.
- Tate et al. summarized the existing literature on patients with pineoblastoma and found that children under 5 years of age and subtotal tumor resection markedly worsened patient survival. According to the Children's Oncology Group trials, these tumors require craniospinal irradiation (with local tumor doses of at least 50 Gy) and adjuvant chemotherapy. When carboplatin and vincristine were administered during craniospinal irradiation followed by 6 months of non-intensive non-cisplatin containing adjuvant chemotherapy, an 84% 2-years progression free survival was reported in pineoblastomas without evidence of dissemination at presentation.
- Patients with pineoblastoma will develop hydrocephalus in majority of the cases and they will require CSF diversion. Ventriculo-peritoneal (V-P) shunt placement is a viable option with low morbidity and mortality rate. However, shunt malfunction in this population is as high as 20%. In addition, tumor metastasis through a CSF shunt has been reported. Endoscopic third ventriculostomy (ETVC) is an alternative option, which also permits a biopsy of the tumor in the same procedure. Ahn et al. reported that the biopsy samples, obtained in the lateral ventricle or pineal region, were more favorable towards a successful diagnosis than those in the thalamus or tectal region. Neuroendoscopic biopsy procedures have been proven safe with low complication rates.[11]
References
- ↑ 1.0 1.1 Pathology of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ Rodjan F, de Graaf P, Brisse HJ, Göricke S, Maeder P, Galluzzi P, Aerts I, Alapetite C, Desjardins L, Wieland R, Popovic MB, Diezi M, Munier FL, Hadjistilianou T, Knol DL, Moll AC, Castelijns JA (September 2012). "Trilateral retinoblastoma: neuroimaging characteristics and value of routine brain screening on admission". J. Neurooncol. 109 (3): 535–44. doi:10.1007/s11060-012-0922-4. PMC 3434888. PMID 22802019.
- ↑ Radiographic features of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ Image courtesy of Dr. Frank Gaillard. Radiopaedia (original file here). Creative Commons BY-SA-NC
- ↑ Microscopic features of pineoblastoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineoblastoma. Accessed on December 1, 2015
- ↑ 6.0 6.1 Histology of pineoblastoma. Dr Frank Gaillard. Radiopaedia 2015. http://radiopaedia.org/cases/pineoblastoma-3. Accessed on December 1, 2015
- ↑ IHC of pineoblastoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineoblastoma. Accessed on December 1, 2015
- ↑ Differential diagnoses of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ DDx of pineoblastoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineoblastoma. Accessed on December 1, 2015
- ↑ 10.0 10.1 10.2 Palled S, Kalavagunta S, Beerappa Gowda J, Umesh K, Aal M, Abdul Razack TP; et al. (2014). "Tackling a recurrent pinealoblastoma". Case Rep Oncol Med. 2014: 135435. doi:10.1155/2014/135435. PMC 4158562. PMID 25210636.
- ↑ 11.0 11.1 11.2 11.3 Alexiou, George A (2012). "Management of pineal region tumours in children". Journal of Solid Tumors. 2 (2). doi:10.5430/jst.v2n2p15. ISSN 1925-4075.
- ↑ General features of pineoblastoma. Libre Pathology 2015. http://librepathology.org/wiki/index.php/Pineal_gland#Pineoblastoma. Accessed on December 1, 2015
- ↑ Epidemiology of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ 14.0 14.1 14.2 14.3 14.4 Clinical presentation of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ Stoiber EM, Schaible B, Herfarth K, Schulz-Ertner D, Huber PE, Debus J; et al. (2010). "Long term outcome of adolescent and adult patients with pineal parenchymal tumors treated with fractionated radiotherapy between 1982 and 2003--a single institution's experience". Radiat Oncol. 5: 122. doi:10.1186/1748-717X-5-122. PMC 3019157. PMID 21184689.
- ↑ 16.0 16.1 Treatment and prognosis of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ CT findings of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ Radiographic features MRI of pineoblastoma. Dr Ayush Goel and Dr Frank Gaillard et al. Radiopaedia 2015. http://radiopaedia.org/articles/pineoblastoma. Accessed on December 1, 2015
- ↑ MR spectroscopy of pineoblastoma. Dr Mohammad A. ElBeialy. Radiopaedia 2015. http://radiopaedia.org/cases/pineoblastoma-6. Accessed on December 1, 2015