Peritonsillar abscess
| Peritonsillar abscess | |
| ICD-10 | J36 |
|---|---|
| ICD-9 | 475 |
| DiseasesDB | 11141 |
| eMedicine | emerg/417 |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Peritonsillar abscess, also called PTA or Quinsy, is a recognised complication of tonsillitis and consists of a collection of pus beside the tonsil (peritonsillar space).
Causes
PTA usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises loose connective tissue and is hence susceptible to formation of abscess. PTA can also occur de novo. Both aerobic and anaerobic bacteria can be causative. Commonly involved species include streptococci, staphylococci and haemophilus.
Symptoms and signs
Unlike tonsillitis, which is more common in the pediatric age group, PTA has a more even age spread — from children to adults. Symptoms start appearing 2-8 days before the formation of abscess. Progressively worsening unilateral sore throat and pain during swallowing usually are the earliest symptoms. As the abscess develops, persistent pain in the peritonsillar area, fever, malaise, headache and change in voice (hot potato voice) may appear. Neck pain associated with tender, swollen lymph nodes, referred ear pain and breath odour are also common. Whilst these signs may be present in tonsillitis itself, a PTA should be specifically considered if there is limited ability to open the mouth (Trismus).
Physical signs include redness and edema in the tonsillar area of the affected side and swelling of the jugulodigastric lymph nodes. The uvula may be displaced towards the unaffected side.
-
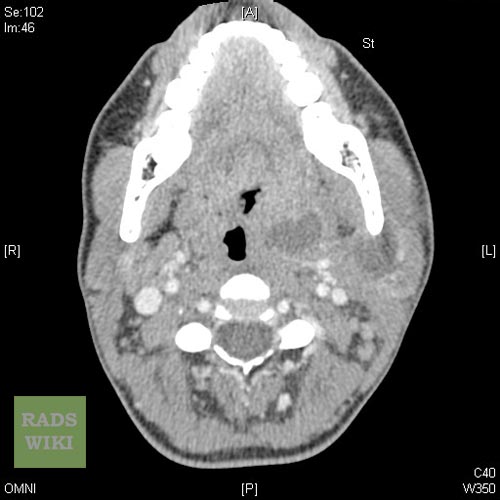
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
Treatment
Treatment is, as for all abscesses, through surgical incision and drainage of the pus, thereby relieving the pain of the stretched tissues. The drainage can often be achieved in the Outpatient Department using a guarded No. 11 blade in an awake and co-operative patient. Sometimes, a needle aspiration can suffice. Antibiotics are also given to treat the infection.
Peritonsillar abscesses are widely considered one of the most painful complications, primarily the surgical draining of the abscess itself. The patient is operated on awake, surgically slicing open the tonsil and draining the abscess.
Complications
- Parapharyngeal abscess
- Extension of abscess in other deep neck spaces leading to airway compromise
- Septicaemia
Notable Quinsy sufferers
- George Washington is believed to have died of complications arising from Quinsy.[1]
- Michel de Montaigne's quinsy brought about the paralysis of his tongue.
- Georges Bizet
- James Gregory of the band The Ordinary Boys was almost killed by quinsy because it was left untreated
- Brian Sweeney
- Alan Burrows
References
- ↑ Mount Vernon Plantation (2006). "Part 4. President and Back Home". Meet George Washington. Mount Vernon Ladies Association. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help)
External links
Template:Respiratory pathology Template:SIB
ka:პერიტონზილური აბსცესი nl:Peritonsillair abces fi:Kurkkupaise