Peritonsillar abscess: Difference between revisions
Prince Djan (talk | contribs) |
Prince Djan (talk | contribs) (→Causes) |
||
| Line 51: | Line 51: | ||
==Causes== | ==Causes== | ||
PTA usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises loose connective tissue and is hence susceptible to formation of abscess. | PTA usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises loose connective tissue and is hence susceptible to formation of abscess. Peritonsilar abscess can also occur ''de novo''. | ||
Both aerobic and anaerobic bacteria can be causative. | Both aerobic and anaerobic bacteria can be causative. | ||
===Life-threatening causes=== | |||
Life-threatening conditions may result in death or permanent disability within 24 hours if left untreated. Peritonsillar abscess may become a life-threatening condition and must be treated as such irrespective of the cause. | |||
===Most common cause=== | |||
The most frequent pathogen of peritonsillar abscess is Streptococcus pyogenes. | |||
===Common causes=== | |||
Some common causes of peritonsillar abscess include: | |||
Fusobacterium necrophorum | |||
Streptococcus milleri | |||
[[Staphylococci]] | |||
[[Haemophilus]] | |||
==Differentiating Peritonsillar abscess from Other Diseases== | ==Differentiating Peritonsillar abscess from Other Diseases== | ||
Revision as of 20:54, 22 February 2017
| Peritonsillar abscess | |
| ICD-10 | J36 |
|---|---|
| ICD-9 | 475 |
| DiseasesDB | 11141 |
| eMedicine | emerg/417 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Kiran Singh, M.D. [2] Prince Tano Djan, BSc, MBChB [3]
Overview
Peritonsillar abscess, also called PTA or Quinsy, is a recognised complication of tonsillitis and consists of a collection of pus beside the tonsil (peritonsillar space).
Historical perspective
The outline below shows the historical perspective of peritonsillar abscess.[1]
- In Second and third century BC, Celcius was the first to document in literature the treatment and pathogenesis of tonsillar pathology.
- In 1700s peritonsillar abscess was first described.
- In the 1930s and 1940s prior to the advent of antibiotics, surgical management was the most common treatment option for peritonsillar abscess. Interval tonsillectomy was mostly done after symptom resolution.
- By 1947, Chaud tonsillectomy or immediate surgical tonsillectomy became the treatment option.
Classification
Pathophysiology
Anatomy
A good understanding of the tonsil and its surrounding space is important in the pathogenesis of peritonsillar abscess. Located within the soft palate is the supratonsillar space occupied by series of 20 to 25 salivary glands described as Weber's glands. The ducts of these glands form a common duct which opens onto the posterior surface of the tonsil after passing through the tonsillar capsule. It is proposed that the secretions from these glands play a rule in food digestion.
The palatine tonsils are found in an anatomical structure called tonsillar fossa. This fossa is bounded anteriorly by palatoglossal muscle, posteriorly by palatopharyngeal muscle, laterally by a fibrous capsule and tonsillar crypts medially. Contents of the tonsillar crypts are expelled by contraction of the tonsillopharyngeus muscle.[2]
Pathogenesis
The pathogenesis of peritonsillar abscess is still not well-understood. There are two proposed theories believed to be involved in the pathogensis of peritonsillar abscess formation.[2][1][3]
- 1. It is proposed to arise from an extension of exudative tonsillitis.
Some authorities believe that blockage of drainage from tonsillar crypt in acute tonsillitis results in spread of infection into the peritonsillar space.
- 2. Involvement of Weber's gland. account for the abscess formation. Some believe that peritonsillar abscess arises from infectious process involving group of salivary glands called Weber's glands located in the supratonsillar space.
Antigenic response following any disturbance arising from within the tonsillar crypt mucosa allows for lymphocytic interaction. This disruption in the crypt epithelium may be preceded by infectious process. Invasion and proliferation of the tonsillar crypt by infectious pathogens results in localized edema and influx of neutrophils. This is clinically seen as inflammed tonsil with or without exudation.[2] Pus accumulation within tissue behind the supratonsillar space leads to tonsillar bulging, uvula and palate deviation.
Causes
PTA usually arises as a complication of an untreated or partially treated episode of acute tonsillitis. The infection, in these cases, spreads to the peritonsillar area (peritonsillitis). This region comprises loose connective tissue and is hence susceptible to formation of abscess. Peritonsilar abscess can also occur de novo. Both aerobic and anaerobic bacteria can be causative.
Life-threatening causes
Life-threatening conditions may result in death or permanent disability within 24 hours if left untreated. Peritonsillar abscess may become a life-threatening condition and must be treated as such irrespective of the cause.
Most common cause
The most frequent pathogen of peritonsillar abscess is Streptococcus pyogenes.
Common causes
Some common causes of peritonsillar abscess include: Fusobacterium necrophorum Streptococcus milleri Staphylococci Haemophilus
Differentiating Peritonsillar abscess from Other Diseases
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Natural history
Complications
The following are some complications that may follow peritonsillar abscess:
Peritonsillar abscess may spread through the deep fascia of the neck with associated rapid progression to a more serious infection.
Prognosis
Diagnosis
History and Symptoms
- Unlike tonsillitis, which is more common in the pediatric age group, peritonsillar abscess has a more even age spread — from children to adults.
- Symptoms start appearing 2-8 days before the formation of abscess. Common symptoms are:
- Drooling
- Dysphagia
- Foul smelling breath
- Fever
- Headache
- Hoarseness,muffled voice (also called hot potato voice)
- Odynophagia
- Otalgia (on the side of the abscess)
- Sore throat ( may be severe and unilateral)
- Stridor[7]
Physical Examination
Signs
- Contralateral deflection of the uvula
- Facial swelling
- Tender submandibular and anterior cervical lymph nodes.
- Tonsillar hypertrophy with likely peritonsillar edema.
- Trismus[8]
Laboratory Findings
Imaging Findings
Treatment
Medical Therapy
Antimicrobial Regimen
Surgery
Prevention
Primary prevention
Secondary Prevention
-
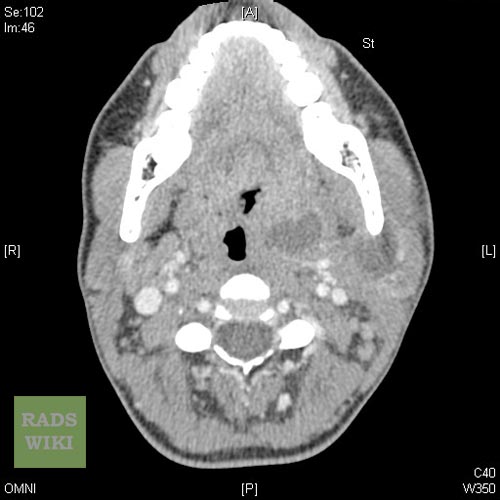
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
-
Peritonsillar abscess Image courtesy of RadsWiki and copylefted
Treatment
Treatment is, as for all abscesses, through surgical incision and drainage of the pus, thereby relieving the pain of the stretched tissues. The drainage can often be achieved in the Outpatient Department using a guarded No. 11 blade in an awake and co-operative patient. Sometimes, a needle aspiration can suffice. Antibiotics are also given to treat the infection.
Peritonsillar abscesses are widely considered one of the most painful complications, primarily the surgical draining of the abscess itself. The patient is operated on awake, surgically slicing open the tonsil and draining the abscess.
Complications
- Parapharyngeal abscess
- Extension of abscess in other deep neck spaces leading to airway compromise
- Septicaemia
Notable Quinsy sufferers
- George Washington is believed to have died of complications arising from Quinsy.[9]
- Michel de Montaigne's quinsy brought about the paralysis of his tongue.
- Georges Bizet
- James Gregory of the band The Ordinary Boys was almost killed by quinsy because it was left untreated
- Brian Sweeney
- Alan Burrows
References
- ↑ 1.0 1.1 Passy V (1994). "Pathogenesis of peritonsillar abscess". Laryngoscope. 104 (2): 185–90. doi:10.1288/00005537-199402000-00011. PMID 8302122.
- ↑ 2.0 2.1 2.2 L. Michaels, H.B. Hellquist Ear, nose and throat histopathology (2nd ed.)Springer-Verlag, London (2001), pp. 281–286
- ↑ Blair AB, Booth R, Baugh R (2015). "A unifying theory of tonsillitis, intratonsillar abscess and peritonsillar abscess". Am J Otolaryngol. 36 (4): 517–20. doi:10.1016/j.amjoto.2015.03.002. PMID 25865201.
- ↑ Coughlin AM, Baugh RF, Pine HS (2014). "Lingual tonsil abscess with parapharyngeal extension: a case report". Ear Nose Throat J. 93 (9): E7–8. PMID 25255362.
- ↑ Deeva YV (2015). "[SURGICAL TREATMENT OF TONSILLAR NECK PHLEGMON]". Klin Khir (7): 47–8. PMID 26591220.
- ↑ Kawabata M, Umakoshi M, Makise T, Miyashita K, Harada M, Nagano H; et al. (2016). "Clinical classification of peritonsillar abscess based on CT and indications for immediate abscess tonsillectomy". Auris Nasus Larynx. 43 (2): 182–6. doi:10.1016/j.anl.2015.09.014. PMID 26527518.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Ferri, Fred (2015). Ferri's clinical advisor 2015 : 5 books in 1. Philadelphia, PA: Elsevier/Mosby. ISBN 978-0323083751.
- ↑ Mount Vernon Plantation (2006). "Part 4. President and Back Home". Meet George Washington. Mount Vernon Ladies Association. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help)
External links
Template:Respiratory pathology
ka:პერიტონზილური აბსცესი nl:Peritonsillair abces fi:Kurkkupaise