Perinatal infection: Difference between revisions
| Line 434: | Line 434: | ||
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3]. | Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3]. | ||
{| class="wikitable" | |||
|- | |||
! Disease !! Medical Therapy !! Surgery !! prevention | |||
|- | |||
| Toxoplasmosis ||*Mother: immediate administration of spiramycin | |||
*Fetus: When confirmed or highly suspected, switch to pyrimethamine, sulfadiazine, and folinic acid. | |||
*Newborn: pyrimethamine, sulfadiazine, and folinic acid.<ref name="test">[ Cline, Matthew K., Chasse Bailey-Dorton, and Maria Cayelli. "Update in Maternity Care: Maternal Infections." Clinics in Office Practice 27, no. 1 (March 2000): 13–33.|| | |||
||*Avoid raw, undercooked, and cured meats. | |||
*Wash hands frequently, especially after touching soil (e.g., during gardening). | |||
*Avoid contact with cat litter.<ref name="test">[Guerina NG. Congenital toxoplasmosis: Clinical features and diagnosis. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. https://www.uptodate.com/contents/congenital-toxoplasmosis-clinical-features-and-diagnosis. Last updated January 6, 2017. Accessed March 22, 2017 ]</ref> | |||
|- | |||
| Example || Example || Example || Example | |||
|- | |||
| Example || Example || Example || Example | |||
|- | |||
| Example || Example || Example || Example | |||
|- | |||
| Example || Example || Example || Example | |||
|- | |||
| Example || Example || Example || Example | |||
|- | |||
| Example || Example || Example || Example | |||
|} | |||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
Revision as of 18:57, 8 October 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Congenital and perinatal infections represent major causes of permanent disability among children worldwide. Linked together by the acronym TORCH, denoting Toxoplasma gondii, rubella virus, cytomegalovirus, and herpes virus, congenital infections can result from only a modest number of human pathogens that cross the placenta and infect the fetus. Although congenital rubella syndrome has been eliminated in the Americas by immunization, several pathogens discussed in this chapter cannot currently be prevented by vaccines or effectively treated with the available antimicrobial drugs. Due to the immaturity of the immune system, newborn infants are at risk for postnatally acquired infections with certain viruses and several bacteria. This chapter summarizes the epidemiology, pathogenesis, clinical manifestations, diagnosis, treatment, and prevention of selected pathogens that can damage the developing nervous system. As emphasized by the persisting challenges of preventing congenital cytomegalovirus infection and the emergence of severe brain damage associated with congenital Zika syndrome, these pathogens remain important causes of cerebral palsy, epilepsy, and intellectual disability.
Historical Perspective
- For approximately 100 years,The concept that certain human pathogens can damage the developing nervous system in utero or perinatally has been appreciated. Although women encounter numerous infectious agents during their pregnancies, relatively few pathogens cross the placenta and cause intrauterine fetal infections.
- In the 1970s investigators at Emory University and the Centers for Disease Control and Prevention (CDC) coined the term TORCH, an acronym underscoring Toxoplasma gondii, rubella virus, cytomegalovirus, and herpesviruses as important, potential causes of congenital infection (Nahmias, 1974). The TORCH concept emphasized that these agents can produce similar clinical manifestations in infected infants. Although congenital rubella virus syndrome has since disappeared in countries with compulsory immunization against this virus (CDC, 2005; WHO, 2017), the TORCH agents, as well as more recently recognized pathogens, such as lymphocytic choriomeningitis virus and Zika virus, remain major causes of long-term neurodevelopmental disabilities among children throughout the world (Bale, 2009).
- The discussion uses the terms congenital and intrauterine interchangeably to indicate that infections occurred before the birth of the infant. By contrast, infections that take place after the birth of the infant are designated perinatal. Because certain perinatal infections, such as those due to enteroviruses, parechoviruses, and herpes simplex viruses, can also damage the immature developing brain, the chapter appropriately contains current information regarding the recognition and management of these infections as well. The agents causing congenital or perinatal infections can produce permanent hearing loss, vision loss, cerebral palsy, cognitive impairment, developmental delay, behavioral disorders or epilepsy in surviving infants and children.[1]
Classification
Perinatal infection is vertically transmitted infection ,which starts at gestational ages between 22[2] and 28 weeks[3] (with regional variations in the definition) and ending seven completed days after birth[2]
Heading text
Pathophysiology
In the spectrum of optimal virulence, vertical transmission tends to evolve benign symbiosis, so is a critical concept for evolutionary medicine. Because a pathogen's ability to pass from mother to chd depends significantly on the hosts' ability to reproduce, pathogens' transmissibility tends to be inversely related to their virulence. In other words, as pathogens become more harmful to, and thus decrease the reproduction rate of, their host organism, they are less likely to be passed on to the hosts' offspring, since they will have fewer offspring.[4]. Although HIV is sometimes transmitted through perinatal transmission, its virulence can be accounted for because its primary mode of transmission is not vertical. Moreover, medicine has further decreased the frequency of vertical transmission of HIV. The incidence of perinatal HIV cases in the United States has declined as a result of the implementation of recommendations on HIV counselling and voluntary testing practices and the use of zidovudine therapy by providers to reduce perinatal HIV transmission.[5]. The price paid in the evolution of symbiosis is, however, great: for many generations, almost all cases of vertical transmission continue to be pathological—in particular if any other routes of transmission exist. Many generations of random mutation and selection are needed to evolve symbiosis. During this time, the vast majority of vertical transmission cases exhibit the initial virulence. In dual inheritance theory, vertical transmission refers to the passing of cultural traits from parents to children.[6].
| maternal infection | |||||||||||||||||||
| placental infection and inflammation | |||||||||||||||||||
| intrauterine growth retardation | fetal infection | ||||||||||||||||||
Causes
Perinatal infection may be caused TORCHES CLAP
- Toxoplasmosis
- Rubella
- Cytomegalovirus
- chlamydia
- Herpes simplex
- Hepatitis B& C
- Enterovirus
- Syphilis
- group B streptococcus
- Chicken box
- Lyme disease
- listeriosis
- AIDS
- Parvovirus B19
- Zika virus(lastest addition)
| Disease | pathogenesis | Associated Conditions | Histopathology | Lab finding & Other evaluation | Prognosis | |
|---|---|---|---|---|---|---|
| Toxoplasmosis | Classic triad Chorioretinitis Hydrocephalus Intracranial calcifications (ring-enhancing lesions) Petechiae and purpura (blueberry muffin rash) | Example | Example | Example | Example | Example |
| Syphilis | Example | Example | Example | Example | Example | Example |
| Listeriosis | Example | Example | Example | Example | Example | Example |
| Varicella zoster virus (VZV) | Example | Example | Example | Example | Example | Example |
| Parvovirus B19 | Example | Example | Example | Example | Example | Example |
| Rubella | Example | Example | Example | Example | Example | Example |
| Cytomegaly virus (CMV) | Example | Example | Example | Example | Example | Example |
| Herpes simplex virus (HSV) | Example | Example | Example | Example | Example | Example |
| Example | Example | Example | Example | Example | Example | Example |
Differentiating [disease name] from other Diseases
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics
| disease | prevalence/ epidemiology |
|---|---|
| congenital toxoplasmosis | reported to be anywhere from 1 in 1000 to 1 in 10,000 births.[7]The rate of congenital infection is about 15% in the first trimester, 25% in the second trimester, and 60% in the third trimester.[8]The severity of congenital infection, however, increases with gestational age. Spiramycin has been reported to decrease the rate of fetal infection by 60%.[9] |
| congenital rubella syndrome | The prototype of the perinatal infections was first recognized by the Australian ophthalmologist Gregg in 1941 during a rubella epidemic.[10]Although large numbers of cases occur in epidemics, the sporadic incidence is low. Eighty to 90% of the adult population is immune, and with the use of rubella vaccine, the susceptible population can be further reduced. Nonetheless, sporadic cases do occur, posing a serious threat to the pregnant woman and her fetus. Although the incidence of rubella reached an all-time reported low in 1988, there has been a distinct increase in the incidence since then, reaching the highest level since 1982 during 1990. Distinct outbreaks seemed to occur in two settings: (1) in locations in which unvaccinated adults congregate, such as workplaces, colleges, and prisons, and (2) among children in religious communities with low levels of vaccination.There also has been an increase in the reported cases of congenital rubella syndrome, but the absolute numbers are quite small.[11] |
| cytomegalovirus | CMV is acquired by 1–2% of all newborns, and approximately 10% of these newborns show some evidence of damage if they are carefully followed. This makes the incidence of significant neonatal infection 1 in 500 to 1000 births. Congenital transmission of CMV can occur with primary infection, reactivation or recurrent maternal infection during pregnancy, although the risk of congenital infection is much higher with primary infection (30–40% with primary infection versus less than 1% with recurrent infection). Maternal recurrent CMV occurs more frequently than primary infection (1–14% vs. 0.7–4%). [12] There is a steady acquisition of CMV from birth to the reproductive age, by which time 50% of women have serologic evidence of prior infection.CMV is transmitted by contact with infected blood, saliva, urine or by sexual contact. CMV is isolated from the endocervix of 3–5% of sexually active women. This provides for additional exposure during the birth process.[13] |
| Herpesvirus | Most (85%) genital infections are caused by Herpesvirus hominis (HSV) type II, with the major perinatal concern being infection acquired by the infant during the birth process.48 Such infections are infrequent (1 in 5000–20,000), but the morbidity and mortality are high. In contrast, the frequency of maternal infection is relatively high. When prenatal patients are screened by both endocervical culture and observation for lesions, the rate is 0.5–1.0%. The comparison of these rates would indicate a relatively low attack rate, although some authors have suggested that the risk of neonatal infection is as high as 50% when vaginal delivery occurs through an infected birth canal.[14] |
| Parvovirus | The annual incidence of acute parvovirus infection during pregnancy is 1 in 400 pregnancies. The seroconversion rate is approximately 16%. The risk of acute infection is highest for susceptible pregnant women with school age children and those who are teachers. The risk of vertical transmission to the fetus is 33%. [15] |
| human immunodeficiency virus | The human immunodeficiency virus (HIV) epidemic is now over 30 years old. The number of cases of people living with HIV/AIDS globally rose from 29 million in 2001 to 33.2 million in 2007.[16] |
| Varicella zoster virus | The varicella zoster virus (VZV) is a member of the herpesvirus group but is not as well known for its perinatal impact. This is in part due to the fact that infection is rare in pregnancy (90% of adults are immune).[17] |
| Hepatitis | It is not known to cause any fetal or neonatal disease but is, nonetheless, a serious illness. Anyone, pregnant or not, who is exposed by contact or travel in endemic areas should receive immune serum globulin (0.02–0.05 mL/kg). If exposure is prolonged and close, the higher dose should be used and repeated every 4–6 months.[18] |
| Influenza | Influenza is one of the more common viral infections to which pregnant women are exposed. When epidemics occur, the problem is magnified because of the patient's susceptibility to a new strain. In addition to the risks of seasonal influenza, pregnant women have experienced excess mortality during the influenza pandemics of 1918–19, 1957–58, and, most recently, the 2009 H1N1 pandemic.[19] |
| Mumps | Mumps is a rare complication of pregnancy, with estimates of incidence varying from 0.8 to 10 cases per 10,000. The severity of the disease is not greater in pregnancy, and 30% of infections are asymptomatic.[20] |
| Genital condylomata | Although the exact prevalence is not known, new techniques, especially DNA sequencing, provide evidence of the ubiquity of this infection. Although the major concern about HPV in women is its role in genital dysplasia and neoplasia, the other concern in pregnancy is fetal/neonatal infection.[21] |
| group B streptococcal infection | Despite the high colonization rate of GBS, the attack rate is quite low. Early-onset infection occurs at a rate of 3–4 per 1000 live births and is manifest within the first 5–7 days of life, usually within 48 hours.[22] |
| Listeriosis | here is very little known about its ecology, colonization rates, or attack rates. There are several reasons for this lack of information, including the difficulties in culturing the organism in the laboratory and its morphologic similarity to diphtheroids [23] |
| Tuberculosis | During the 19th and early 20th centuries, it was the subject of many novels and dramatic operas. The advent of chemotherapeutic agents radically changed the attitudes toward and management of this dreaded disease.[24]The development of effective treatment has essentially reduced the possibility of this disease having any substantial effects on pregnancy.There may be an increase in disease activity in the postpartum period, but since the advent of effective therapy this has little clinical significance. [25] |
| Syphilis | The incidence of syphilis in adults has risen dramatically in the past few years, particularly in endemic urban areas. Congenital syphilis is also seen with increasing frequency in these same areas.[26] |
| Gonorrhea | Maternal infection most often is asymptomatic, and in some populations the rate of endocervical colonization exceeds 5%. Salpingitis rarely occurs in the first trimester, and with PROM, cervical colonization can lead to chorioamnionitis in late pregnancy. [27] Disseminated gonorrhea occurs in pregnancy;[28] gonococcal arthritis has a special propensity for pregnancy, with 40% of cases occurring in gravidas.[29] |
| Mycoplasmas | These associations have not been conclusively established, and, consequently, treatment should be used only if there is reasonable evidence for causality in a given situation.[30] |
| Chlamydia | The rate of asymptomatic cervical infection in obstetric populations is high (5–10%), as is urethral infection in the male (sexual transmission occurs). Newborns acquire the organism at birth in significant numbers, and conjunctivitis is common. [31] |
| Salmonella | Typhoid fever is currently a rare disease in the United States. When the disease does occur in pregnancy, it may, like any serious febrile illness, result in spontaneous abortion or premature labor. In those cases in which the exposure of the fetus to maternal disease has been less than 2–3 weeks, the organism has not been recovered from aborted fetuses.[32] |
| Trichomonas vaginalis | Trichomonas vaginalis is likely the most common parasite to infect women. Newborns can be infected at birth; however, the manifestations are generally benign.[33] |
| Malaria | Malaria is not a common problem for obstetric practice in the United States, but in endemic areas it is a serious concern and a leading cause of anemia in pregnancy. Perhaps the most likely consideration is a pregnant woman who must travel to an endemic area [34] |
| Candidiasis | Vaginitis caused by Candida albicans is very common during pregnancy. [35] |
| Coccidioidomycosis | Coccidioides immitis most often produces a rather benign and self-limited respiratory infection. It is endemic in the Southwestern United States and in 10% of cases progresses to disseminated infection. If the latter occurs in pregnancy, the placenta may be involved; however, there are no documented cases of congenital infection.[36] |
Age
- Patients of all age groups may develop perinatal infection.
Gender
- perinatal infection affects boy and girls children equally.
Race
- There is no racial predilection for perinatal infection.
Risk Factors
- Common risk factors in the development of [Perinatal infection ] [37]are
| Fetal causes | maternal causes |
|---|---|
| Birth weight | chorioamnionitis |
| Ceseran delivary | Hypertension (pregestational and gestational including preeclampsia) |
| Multiple delivary | Diabetes (pregestational and gestational) |
| Fetal distress | |
| Meconium aspiration | |
| Patent ductus arteriosus |
Infant outcomes
| Infant outcome |
|---|
| Mechanical ventilation |
| Pneumothorax |
| Respiratory distress syndrome |
| Chronic lung disease |
| Necrotizing enterocolitis |
| Interventricular hemorrhage |
| Hypoxic - ischemic encephalopathy |
| Retinopathy of prematurity |
| Extracorporeal life support |
| In hospital death |
In addition, we evaluated combined grade 3 and grade 4 intraventricular hemorrhage and combined stages 3 through 5 ROP to align with common categorization of these more clinically important outcomes.
Natural History, Complications and Prognosis
Early clinical features include
| Feature | CMV | LCM VIRUS | Rubella virus | Toxoplasma gondii | Treponema pallidum | Zika virus |
|---|---|---|---|---|---|---|
| Systemic | ||||||
| Jaundice | +++ | - | ++ | +++ | +++ | - |
| Hepatosplenomegaly | +++ | - | ++ | +++ | ++ | - |
| Rash | Petechial | Bullous (rare) | Petechial “blue-berry” | Petechial | Petechial | - |
| Anemia | ++ | - | + | - | + | - |
| Neurologic/eye | ||||||
| Microcephaly | ++ | + | ++ | +/- | - | +++ |
| Macrocephaly | +/- | ++ | - | +++ | - | + |
| Chorioretinitis | + | +++ | + | +++ | + | ++ |
| Cataract | - | - | ++ | - | - | + |
-: not seen; +/: rare; +: occasional; ++: common; +++: very common.[38]
Diagnosis
Diagnostic Criteria
- The diagnosis of [perinatal diagnosis] [39]is made when
- Chlamydia can be diagnosed by taking a cotton swab sample of the cervix and vagina during the third trimester of the pregnancy. Chlamydial cell cultures take three to seven days to grow. DNA probes are available for more rapid diagnosis.
- Past or recent infection with cytomegalovirus (CMV) can be identified by documentation of seroconversion of a previously seronegative patient (the development of IgG antibodies to CMV in a patient who was previously negative for these antibodies) and CMV can be grown from body fluids.[40]
- Genital herpes is suspected with the outbreak of a particular kind of genital sore. The sore can be cultured and tested to confirm that HSV-2 is present.
- Hepatitis B can be identified through a blood test for the hepatitis B surface antigen (HBsAg) in pregnant women. The test is part of prenatal health programs.
- Human immunodeficiency virus (HIV) can be detected using a blood test and is part of most prenatal screening programs.
- Human papillomavirus (HPV) causes the growth of warts in the genital area. The wart tissue can be removed with a scalpel and tested to determine what type of HPV virus caused the infection.
- Pregnant women are usually tested for antibodies to rubella, which would indicate that they have been previously exposed to the virus and, therefore, would not develop infection during pregnancy if exposed.
- Group beta streptococcus (GBS) can be detected by a vaginal or rectal swab culture and sometimes from a urine culture. Blood tests can be used to confirm GBS infection in infants who exhibit symptoms.
- Pregnant women are usually tested for syphilis as part of the prenatal screening, generally with a blood test.
- ZIKA virus Methods for testing include both serologic and molecular tests. Laboratory tests in include ZIKV IgM, ZIKV NAT, and plaque reduction neutralization testing.[41]
History and Symptoms
If a developing fetus is infected by a TORCH agent, the outcome of the pregnancy may be miscarriage, stillbirth, delayed fetal growth and maturation (intrauterine growth retardation), or early delivery. In addition, newborns infected by any one of the TORCH agents may develop a spectrum of similar symptoms and findings. These may include
- listlessness (lethargy),
- fever,
- difficulties feeding,
- enlargement of the liver and spleen (hepatomegaly),
- and decreased levels of the oxygen-carrying pigment (hemoglobin) in the blood (anemia).
In addition, affected infants may develop
- areas of bleeding, resulting in reddish or purplish spots or areas of discoloration visible through the skin (petechia or purpura);
- yellowish discoloration of the skin, whites of the eyes, and mucous membranes (jaundice);
- inflammation of the middle and innermost layers of the eyes (chorioretinitis); and/or other symptoms and findings.
Each infectious agent may also cause additional abnormalities that may vary in degree and severity, depending upon the stage of fetal development at time of infection and/or other factors.
Following is a more specific description of the TORCH agents.
Toxoplasmosis is an infectious disease caused by the microscopic parasitic organism called Toxoplasma gondii. Classic triad of toxoplasmosis Chorioretinitis (a form of posterior uveitis) Diffuse intracranial calcifications Hydrocephalus
Rubella is a viral infection characterized by fever, upper respiratory infection, swelling of the lymph nodes, skin rash, and joint pain. Severely affected newborns and infants may have visual and/or hearing impairment, heart defects, calcium deposits in the brain, and/or other abnormalities.
Cytomegalovirus (CMV) Infection is a viral infection that may occur during pregnancy, after birth, or at any age. In severely affected newborns, associated symptoms and findings may include growth retardation, an abnormally small head (microcephaly), enlargement of the liver and spleen (hepatosplenomegaly), inflammation of the liver (hepatitis), low levels of the oxygen-carrying pigment in the blood due to premature destruction of red blood cells (hemolytic anemia), calcium deposits in the brain, and/or other abnormalities.
Neonatal Herpes is a rare disorder affecting newborns infected with the Herpes simplex virus (HSV). This disorder may vary from mild to severe. In most cases, the disorder is transmitted to an infant from an infected mother with active genital lesions at the time of delivery. In the event that a mother has a severe primary genital outbreak, it is possible that a mother may transmit the infection to the fetus. After delivery, direct contact with either genital or oral herpes sores may result in neonatal herpes. Severely affected newborns may develop fluid-filled blisters on the skin (cutaneous vesicles), lesions in the mouth area, inflammation of the mucous membrane lining the eyelids and whites of the eyes (conjunctivitis), abnormally diminished muscle tone, inflammation of the liver (hepatitis), difficulties breathing, and/or other symptoms and findings.
Parvovirus B19 Infection during pregnancy occurs in 1–5% of pregnancies. The virus can cause miscarriage, fetal anaemia, hydrops fetalis (abnormal accumulation of fluid in the fetal tissues), myocarditis, and/or intrauterine fetal death.
Syphilis
Early congenital syphilis
Hepatomegaly and jaundice
Rhinorrhea with white or bloody nasal discharge
Maculopapular rash on palms and soles
Skeletal abnormalities (e.g., metaphyseal dystrophy, periostitis)
Generalized lymphadenopathy (nontender)
Listeriosis Intrauterine transmission Increased risk of premature birth and spontaneous abortion Early-onset syndrome: granulomatosis infantiseptica Severe systemic infection characterized by disseminated abscesses (may develop in any organ system) Most common findings: respiratory distress and skin lesions Signs of meningitis may already develop. Transmission during birth or postnatally (via contact with the mother or contaminated environment)
enterovirus
Wide spectrum of clinical presentations,
from non-specific febrile illness to fatal multisystem disease, Fever, irritability,poor feeding, lethargy Maculopapular rash in 50% Respiratory symptoms in 50% Gastrointestinal symptoms in 20% Hepatitis in 50% May have myocarditis, meningoencephalitis
Physical Examination
| Finding(s) | Possible congenital infections |
|---|---|
| Intrauterine growth retardation | Rubella, cytomegalovirus (CMV), toxoplasmosis |
| Anemia with hydrops | Parvovirus B19, syphilis, CMV, toxoplasmosis |
| Bone lesions | Syphilis, rubella |
| Cerebral calcification |
|
| Congenital heart disease | Rubella |
| Hearing loss (commonly progressive) | Rubella, CMV, toxoplasmosis, syphilis |
| Hepatosplenomegaly | CMV, rubella, toxoplasmosis, HSV, syphilis, enterovirus, parvovirus B19 |
| Hydrocephalus | Toxoplasmosis, CMV, syphilis, possibly enterovirus |
| Hydrops, ascites, pleural effusions | Parvovirus B19, CMV, toxoplasmosis, syphilis |
| Jaundice with or without thrombocytopenia | CMV, toxoplasmosis, rubella, HSV, syphilis, enterovirus |
| Limb paralysis with atrophy and cicatrices | Varicella |
| Maculopapular exanthem | Syphilis, measles, rubella, enterovirus |
| Microcephaly | CMV, toxoplasmosis, rubella, varicella, HSV |
| Myocarditis/encephalomyocarditis | Echovirus, coxsackie B, other enterovirus |
| Ocular findings | CMV, toxoplasmosis, rubella, HSV, syphilis, enterovirus, parvovirus B19 |
| Progressive hepatic failure and clotting abnormalities | Echovirus, coxsackie B, other enterovirus, HSV, toxoplasmosis |
| Pseudoparalysis, pain | Syphilis |
| Vesicles | HSV, syphilis, varicella, enterovirus |
Laboratory Findings
- rubella may be diagnosed by detection of specific IgM, but virus detection is the technique of choice.
- VZV may be diagnosed by serological techniques in up to 71% of cases. Detection of virus in vesicle scrapings or swabs from the oropharynx is the technique of choice for neonatal HSV.
- enterovirus infections are best diagnosed by detection of viral RNA.
- HIV-1 may be diagnosed within 3 months of birth by testing serial blood samples with a combination of techniques. Maternal infection with HBV, HCV, HIV and HTLV1/11 may be diagnosed by serological techniques and genital PVs by detection of viral DNA. Chorionic villus samples, amniotic fluid and fetal blood may be obtained for prenatal diagnosis of infection.
- detection of virus in amniotic fluid is the technique of choice for prenatal diagnosis of CMV, insufficient data is currently available to determine whether it may be used for intrauterine rubella.
- The most reliable technique for diagnosis of fetal B19 infection is detection of viral DNA .
the use of TORCH screening should be discouraged.[42]
Electrocardiogram
There are no ECG findings associated with [disease name].
OR
An ECG may be helpful in the diagnosis of [disease name]. Findings on an ECG suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
X-ray
There are no x-ray findings associated with [disease name].
OR
An x-ray may be helpful in the diagnosis of [disease name]. Findings on an x-ray suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no x-ray findings associated with [disease name]. However, an x-ray may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
Echocardiography or Ultrasound
There are no echocardiography/ultrasound findings associated with [disease name].
OR
Echocardiography/ultrasound may be helpful in the diagnosis of [disease name]. Findings on an echocardiography/ultrasound suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
There are no echocardiography/ultrasound findings associated with [disease name]. However, an echocardiography/ultrasound may be helpful in the diagnosis of complications of [disease name], which include [complication 1], [complication 2], and [complication 3].
CT scan
CT scan may be helpful in the diagnosis of Toxoplasmosis include dilated ventricles with multiple subependymal and parenchymal calcifications .
MRI
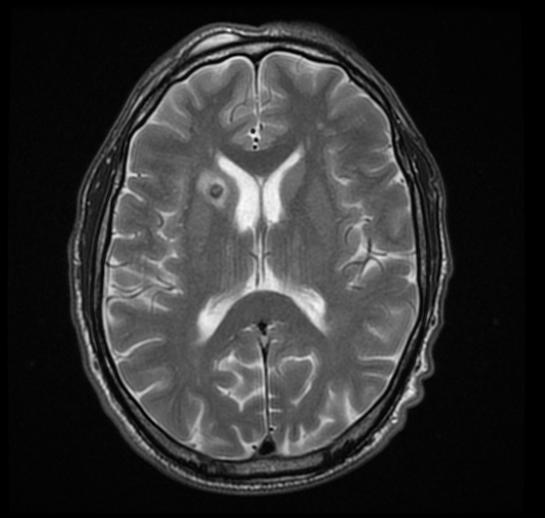
MRI may be helpful in the diagnosis of [Toxoplasmosis]. Findings on MRI suggestive of/diagnosis include ring enhanced lesion
-
Caption1
Other Imaging Findings
Imaging features of selected congenital infections [43]
| Imaging feature | CMV | LCM virus | Rubella virus | Toxoplasma gondii | Zika Virus |
|---|---|---|---|---|---|
| Calcifications | +++ | +++ | +++ | +++ | +++ |
| Polymicrogyria | +++ | ++ | - | - | +++ |
| Hydrocephalus | + (passive) | ++ (obstructive and passive) | - | ++ (obstructive) | ++ (obstructive and passive) |
| Lissencephaly | ++ | + | - | - | ++ |
| Cerebellar hypoplasia | ++ | + | - | - | ++ |
| White matter lesions | +++ | +/- | ++ | + | ++ |
| Fetal brain disruption | - | - | - | - | +++ |
CMV=cytomegalovirus; LCM virus =lymphocytic choriomeningitis virus. (-) absent; (+) uncommon or rare; (++) common; (+++) very common.
Other Diagnostic Studies
There are no other diagnostic studies associated with [disease name].
OR
[Diagnostic study] may be helpful in the diagnosis of [disease name]. Findings suggestive of/diagnostic of [disease name] include [finding 1], [finding 2], and [finding 3].
OR
Other diagnostic studies for [disease name] include [diagnostic study 1], which demonstrates [finding 1], [finding 2], and [finding 3], and [diagnostic study 2], which demonstrates [finding 1], [finding 2], and [finding 3].
| Disease | Medical Therapy | Surgery | prevention |
|---|---|---|---|
| Toxoplasmosis | *Mother: immediate administration of spiramycin
| ||
| Example | Example | Example | Example |
| Example | Example | Example | Example |
| Example | Example | Example | Example |
| Example | Example | Example | Example |
| Example | Example | Example | Example |
| Example | Example | Example | Example |
Treatment
Medical Therapy
- The mainstay of therapy for [ Toxoplasmosis].[44] is
- Mother: immediate administration of spiramycin
- Fetus: When confirmed or highly suspected, switch to pyrimethamine, sulfadiazine, and folinic acid.
- Newborn: pyrimethamine, sulfadiazine, and folinic acid
- The mainstay of therapy for [ Syphilis] is
14 days of IV penicillin G for both pregnant women and newborns
- The mainstay of therapy for [ lysteriosis] is
IV ampicillin and gentamicin (for both mother and newborn)
- The mainstay of therapy for [ Varicella ] is
For pregnant women or newborns with (severe) infection: acyclovir Administer postexposure prophylaxis in newborns if mother displays symptoms of varicella < 5 days before delivery: IgG antibodies (varicella-zoster immune globulin, VZIG)
- The mainstay of therapy for [ Parvovirus B19 ] is
Intrauterine fetal blood transfusion in cases of severe fetal anemia
- The mainstay of therapy for [ Rubella ] is
Intrauterine rubella infection > 16 weeks: reassurance Congenital rubella syndrome: supportive care (based on individual disease manifestations) and surveillance (including monitoring for late-term complication
- The mainstay of therapy for [ congenital CMV ] is
Fetus Severe anemia: intrauterine blood transfusions Thrombocytopenia: platelet transfusions Newborn Supportive therapy of symptoms (e.g., fluid/electrolyte imbalances, anemia, thrombocytopenia, seizures, secondary infections) Ganciclovir, valganciclovir, or foscarnet Mother: valacyclovir is the only therapy approved during pregnancy; trials with CMV specific hyperimmune globulin ongoing.
Surgery
only for herpes simplex [45] :Cesarean section in women with active genital lesions or prodromal symptoms (e.g., burning pain)
Prevention
Minimizing the risk of transmitting a maternal infection to a fetus is often a major concern for parents. The first step is identifying possible maternal infections. Proper prenatal care in many cases allows for early diagnosis and thus early treatment of certain infections, thus improving the newborn's prognosis [46]
A woman's nutritional status may contribute to her ability to fight off infections, particularly in cases of malnutrition . A well-balanced diet rich in nutrients such as folic acid , calcium, iron, zinc, vitamin D, and the B vitamins is recommended for pregnant women. Mothers are recommended to eat approximately 300 additional calories day (above and beyond a normal non pregnancy diet) to support the fetus's growth and development [47]
Prevention f Toxoplasmosis .[44]
- Avoid raw, undercooked, and cured meats.
- Wash hands frequently, especially after touching soil (e.g., during gardening).
- Avoid contact with cat litter.
Prevention of syphilis [48]
- Maternal screening in early pregnancy
- Nationally notifiable condition: Congenital syphilis and syphilitic childbirth must be reported to local or state health department.
Prevention of Listeriosis [49]
- Avoidance of soft cheeses
- Avoidance of potentially contaminated water and food: See “Food and water safety” in food poisoning.
- Nationally notifiable condition: Listeriosis must be reported to the local or state health department.
Prevention of varicella infection [50]
- Immunization of seronegative women before pregnancy
- VZIG in pregnant women without immunity within 10 days of exposure
Prevention of Parvovirus infection (B 19)[51]
- Hand hygiene (frequent hand washing)
- Pregnant women with risk factors for TORCH infection should avoid potentially contaminated workplaces (e.g., schools, pediatric clinics)
Prevention of congenital rubella[52]
- Immunization of seronegative women before pregnancy
- Nationally notifiable condition: Suspected congenital rubella syndrome must be reported to the local or state health department.
Prevention of Toxoplasmosis [53]
- Frequent hand washing, especially after contact with bodily secretions of small children (e.g., diaper changing)
- Avoidance of food sharing with children
- Avoidance of kissing small children on the mouth
Prevention of herpes simplex virus[54]
- Antiviral therapy (acyclovir) beginning at 36 weeks of gestation for individuals with a known history of HSV lesions
- Cesarean section in women with active genital lesions or prodromal symptoms (e.g., burning pain)
prevention of ZIKV include the following:[55]
- Avoidance of travel to ZIKV endemic areas during pregnancy.
- The use of N,N-Diethyl-meta-toluamide, which has been recommended in pregnancy to prevent ZIKV infection,85 long sleeves and pants or permethrin-treated
clothing, and use of mosquito nets and window screens if living in or traveling to an endemic area.
- If living in an endemic area, areas of standing water (such as tires, buckets,planters, etc) should be eliminated because they are a breeding area for
mosquitoes.
- All pregnant women and their partners should receive counseling on prevention measures including avoidance of mosquito bites and sexual transmission.
- If a couple has a male partner and he travels to an area with ZIKV, they should use
condoms or abstain from sexual activity for 6 months (even in the absence of symptoms).
- If a female travels to an area with risk of ZIKV, condoms or abstinence from sexual activity for 8 weeks (even in the absence of symptoms) is recommended.
- If a pregnant patient and her partner travel to or live in an area with ZIKV, condoms should be used each time the couple has sex for the remainder of pregnancy, or they should
abstain from sexual activity.
References
- ↑ [Ostrander, B., & Bale, J. F. (2019). Congenital and perinatal infections. Neonatal Neurology, 133–153. doi:10.1016/b978-0-444-64029-1.00006-0 ], additional text.
- ↑ 2.0 2.1 "Definitions and Indicators in Family Planning. Maternal & Child Health and Reproductive Health" (PDF). Archived from the original (PDF) on 25 January 2012. Unknown parameter
|url-status=ignored (help) By European Regional Office, World Health Organization. Revised March 1999 & January 2001. In turn citing: WHO Geneva, WHA20.19, WHA43.27, Article 23 - ↑ Singh, Meharban (2010). Care of the Newborn. p. 7. Edition 7. ISBN 9788170820536
- ↑ Stewart, Andrew D.; Logsdon, John M.; Kelley, Steven E. (April 2005). "An empirical study of the evolution of virulence under both horizontal and vertical transmission". Evolution. 59 (4): 730–739. doi:10.1554/03-330. ISSN 0014-3820. PMID 15926685. Unknown parameter
|s2cid=ignored (help) - ↑ Joo, Esther; Carmack, Anne; Garcia-Buñuel, Elizabeth; Kelly, Chester J. (February 2000). "Implementation of guidelines for HIV counseling and voluntary HIV testing of pregnant women". American Journal of Public Health. 90 (2): 273–276. doi:10.2105/AJPH.90.2.273. ISSN 0090-0036. PMC 1446152. PMID 10667191.
- ↑ Cavalli-Sforza, Luigi Luca; Feldman, Marcus W. (1981). Cultural Transmission and Evolution: A Quantitative Approach. Monographs in Population Biology. 16. Princeton University Press. pp. 1–388. ISBN 0-691-08283-9. PMID 7300842. Retrieved 30 April 2016.
- ↑ [ Remington JS, McLeod R, Desmonts G: Toxoplasmosis. In Remington JS, Klein JO (eds): Infectious Diseases of the Fetus and Newborn Infant, 4th edn, pp 140–247, Philadelphia, WB Saunders, 1995], additional text.
- ↑ [ Sever JL, Larsen JN, Grossman JH: Toxoplasmosis. In: Handbook of Perinatal Infections, pp 157–163. Boston, Little, Brown, 1979], additional text.
- ↑ [Mombro M, Perathoner C, Leone A, Nicocia M, Moirhagi Ruggenni A, et al: Congenital toxoplasmosis: 10 year follow up. Eur J Pediatr 1995: 154: 635-639 ], additional text.
- ↑ [Gregg NM: Congenital cataract following German measles in the mother. Trans Ophthalmol Soc Aust 3: 35, 1941], additional text.
- ↑ [ Centers for Disease Control: Increase in Rubella and Congenital Rubella Syndrome B United States, 1988 B 1991. MMWR Morb Mortal Wkly Rep 40: 93, 1991], additional text.
- ↑ [Daniel Y, Gull I, Peyser R, Lesing JB: Congenital cytomegalovisus infection. Eur J Obstet Gynecol Reprod Biol 63: 7, 1995 ], additional text.
- ↑ [ Dannemann BR, Vaughan WC, Thulliez P, et al: Differential agglutination test for diagnosis of recently acquired infection with Toxoplasma gondii. J Clin Microb 28: 1928, 1990], additional text.
- ↑ [Kaufman RH, Gardner HL, Brown D: Herpes genitalis treated by photoinactivation of virus. Am J Obstet Gynecol 117: 1144, 1973 ], additional text.
- ↑ [ Cosmi E, Mari G, Chaie LD, et al: Noninvasive diagnosis by Doppler ultrasonography of fetal anemia resulting from parvovirus infection. Am J Obstet Gynecol 2002; 187: 1290-3], additional text.
- ↑ [ UNAIDS, 2007 AIDS Epidemic Update; December 2007 ], additional text.
- ↑ [Savage MO, Mossa A, Gordon RR: Maternal varicella infections as a cause of fetal malformations. Lancet 1: 352, 1973 ], additional text.
- ↑ [ Amstey MS: Treatment and prevention of viral infections. Clin Obstet Gynecol 31: 501, 1988 ], additional text.
- ↑ [ACOG committee opinion #468, october 2010. www.acog.org/from_home/publications/immunization/co468.pdf ], additional text.
- ↑ [ Siegel M, Fuerst HT: Low birth weight and maternal virus diseasses: A prospective study of rubella, measles, mumps, chickenpox, and hepatitis. JAMA 197: 88, 1966 ], additional text.
- ↑ [ Shah DV, Kashima HK, Busema J: Reducing mortality from respiratory papillomas. Contemp Obstet Gynecol 20: 65, 1987], additional text.
- ↑ [ Howard JB, McCracken GH Jr: The spectrum of group B streptococcal infections in infancy. Am J Dis Child 128: 815, 1974 ], additional text.
- ↑ [Bojsen-Moller J: Human listeriosis: Diagnostic, epidemiologic and clinical studies. Acta Pathol Microbiol Immunol Scand 229 (Suppl): 1, 1972], additional text.
- ↑ [ Pridie RB, Stradling P: Management of pulmonary tuberculosis during pregnancy. BMJ 2: 78, 1961 ], additional text.
- ↑ [ Hamadeh MA, Glassroth J: Tuberculosis and pregnancy. Chest 101: 1114, 1992 ], additional text.
- ↑ [ Minkoff HL, McCalla S, Delke I et al: The relationship of cocaine use of syphilis and human immunodeficiency virus infections among inner city parturient women. Am J Obstet Gynecol 163: 521, 1990], additional text.
- ↑ [ Handsfield HH, Hodson WA, Holmes KK: Neonatal gonococcal infection: I. Orogastric contamination with Neisseria gonorrhoeae. JAMA 225: 697, 1973], additional text.
- ↑ [ Watring WG, Vaughn DL: Gonococcemia in pregnancy. Obstet Gynecol 48: 428, 1976 ], additional text.
- ↑ [Chapman DR, Fernandez-Rocha L: Gonococcal arthritis in pregnancy: Ten-year review. South Med J 68: 1333, 1975], additional text.
- ↑ [Klein JO, Buckland D, Finland M: Colonization of newborn infants by mycoplasmas. N Engl J Med 280: 1025, 1969 ], additional text.
- ↑ [ Schacter J: Chlamydial infections. N Engl J Med 298:a, 428; b, 490; 540, 1978 ], additional text.
- ↑ [Hornick RB: Nontyphoidal salmonellosis. In Hoeprich PD (ed): Infectious Diseases, pp 555–561. Philadelphia, Harper & Row, 1977], additional text.
- ↑ [Sever JL, Larsen JN, Grossman JH: Toxoplasmosis. In: Handbook of Perinatal Infections, pp 157–163. Boston, Little, Brown, 1979], additional text.
- ↑ [ Sever JL, Larsen JN, Grossman JH: Toxoplasmosis. In: Handbook of Perinatal Infections, pp 157–163. Boston, Little, Brown, 1979], additional text.
- ↑ [Dvorak AM, Gavaller B: Congenital systemic candidiasis. N Engl J Med 274: 540, 1966 ], additional text.
- ↑ [Purtilo DT: Opportunistic mycotic infections in pregnant women. Am J Obstet Gynecol 122: 607, 1975], additional text.
- ↑ [ https://pediatrics.aappublications.org/content/143/2/e20181487], additional text.
- ↑ [ Ostrander, B., & Bale, J. F. (2019). Congenital and perinatal infections. Neonatal Neurology, 133–153. doi:10.1016/b978-0-444-64029-1.00006-0 ], additional text.
- ↑ [Ford-Jones, E. Lee, and Greg Ryan. "Implications for the Fetus of Maternal Infections in Pregnancy." In Infectious Diseases , 2nd ed. Edited by Jonathan Cohen et all. New York: Mosby, 2004 ], additional text.
- ↑ [ Lazzarotto T, Guerra B, Gabrielli L, et al. Update on the prevention, diagnosis and management of cytomegalovirus infection during pregnancy. Clin Microbiol Infect 2011;17:1285–93. ], additional text.
- ↑ [ Rabe IB, Staples JE, Villanueva J, et al. Interim guidance for interpretation of Zika virus antibody test results. MMWR Morb Mortal Wkly Rep 2016;65:543–6. ], additional text.
- ↑ [Best, J. M. (1996). Laboratory diagnosis of intrauterine and perinatal virus infections. Clinical and Diagnostic Virology, 5(2-3), 121–129. doi:10.1016/0928-0197(96)00213-9 ], additional text.
- ↑ [Ostrander, B., & Bale, J. F. (2019). Congenital and perinatal infections. Neonatal Neurology, 133–153. doi:10.1016/b978-0-444-64029-1.00006-0 ], additional text.
- ↑ 44.0 44.1 [ Cline, Matthew K., Chasse Bailey-Dorton, and Maria Cayelli. "Update in Maternity Care: Maternal Infections." Clinics in Office Practice 27, no. 1 (March 2000): 13–33. Read more: http://www.healthofchildren.com/P/Perinatal-Infection.html#ixzz6YvWnLQK0]
- ↑ [ Riley LE, Wald A. Genital herpes simplex virus infection and pregnancy. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. http://www.uptodate.com/contents/genital-herpes-simplex-virus-infection-and-pregnancy. Last updated June 18, 2016. Accessed March 22, 2017.], additional text.
- ↑ [Ford-Jones, E. Lee, and Greg Ryan. "Implications for the Fetus of Maternal Infections in Pregnancy." In Infectious Diseases , 2nd ed. Edited by Jonathan Cohen et all. New York: Mosby, 2004. ], additional text.
- ↑ [Ford-Jones, E. Lee, and Greg Ryan. "Implications for the Fetus of Maternal Infections in Pregnancy." In Infectious Diseases , 2nd ed. Edited by Jonathan Cohen et all. New York: Mosby, 2004 ], additional text.
- ↑ [Centers for Disease Control and Prevention. 2017 Nationally Notifiable Conditions. https://wwwn.cdc.gov/nndss/conditions/notifiable/2017/. Updated January 1, 2017. Accessed March 22, 2017. ], additional text.
- ↑ [ Janakiraman V. Listeriosis in pregnancy: diagnosis, treatment, and prevention. Rev Obstet Gynecol. 2008; 1(4): pp. 179–85. pmid: 19173022. ], additional text.
- ↑ [ Centers for Disease Control and Prevention. 2017 Nationally Notifiable Conditions. https://wwwn.cdc.gov/nndss/conditions/notifiable/2017/. Updated January 1, 2017. Accessed March 22, 2017. ], additional text.
- ↑ [ Lamont RF, Sobel JD, Vaisbuch E, et al. Parvovirus B19 infection in human pregnancy. BJOG. 2010; 118(2): pp. 175–186. doi: 10.1111/j.1471-0528.2010.02749.x ], additional text.
- ↑ [ Centers for Disease Control and Prevention. Three Cases of Congenital Rubella Syndrome in the Postelimination Era: Maryland, Alabama, and Illinois, 2012. MMWR Morb Mortal Wkly Rep. 2013; 62(12): pp. 226–229. url: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6212a3.htm. ], additional text.
- ↑ [Demmler-Harrison GJ. Congenital cytomegalovirus infection: Management and outcome. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. http://www.uptodate.com/contents/congenital-cytomegalovirus-infection-management-and-outcome. Last updated July 29, 2016. Accessed March 22, 2017. ], additional text.
- ↑ [ Demmler-Harrison GJ. Neonatal herpes simplex virus infection: Management and prevention. In: Post TW, ed. UpToDate. Waltham, MA: UpToDate. http://www.uptodate.com/contents/neonatal-herpes-simplex-virus-infection-management-and-prevention. Last updated February 16, 2016. Accessed March 22, 2017. ], additional text.
- ↑ [ Centers for Disease Control and Prevention (CDC). Zika virus prevention. Available at: https://www.cdc.gov/zika/prevention/index.html. Accessed April 24, 2017 ], additional text.