Pegylated interferon alfa-2a: Difference between revisions
Gloria Picoy (talk | contribs) No edit summary |
Gloria Picoy (talk | contribs) No edit summary |
||
| (One intermediate revision by the same user not shown) | |||
| Line 5: | Line 5: | ||
|drugClass=alfa interferon | |drugClass=alfa interferon | ||
|indicationType=treatment | |indicationType=treatment | ||
|indication=chronic hepatitis C (CHC) and chronic hepatitis B (CHB) | |indication=chronic hepatitis C ([[CHC]]) and chronic hepatitis B ([[CHB]]) | ||
|hasBlackBoxWarning=Yes | |hasBlackBoxWarning=Yes | ||
|adverseReactions=fatigue/asthenia, pyrexia, myalgia | |adverseReactions=[[fatigue]]/[[asthenia]], [[pyrexia]], [[myalgia]] and [[headache]] | ||
|blackBoxWarningTitle=Risk of Serious Disorders | |blackBoxWarningTitle=Risk of Serious Disorders | ||
|blackBoxWarningBody=Alpha interferons may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping Pegylated interferon alfa-2a therapy. | |blackBoxWarningBody=Alpha interferons may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping Pegylated interferon alfa-2a therapy. | ||
|fdaLIADAdult======Chronic Hepatitis C===== | |fdaLIADAdult======Chronic Hepatitis C===== | ||
* Pegylated interferon alfa-2a, as part of a combination regimen with other hepatitis C virus (HCV) antiviral drugs, is indicated for the treatment of adults with chronic hepatitis C (CHC) with compensated liver disease. Pegylated interferon alfa-2a monotherapy is only indicated for the treatment of patients with CHC with compensated liver disease if there are contraindications or significant intolerance to other HCV antiviral drugs. | * Pegylated interferon alfa-2a, as part of a combination regimen with other hepatitis C virus ([[HCV]]) antiviral drugs, is indicated for the treatment of adults with chronic hepatitis C ([[CHC]]) with compensated liver disease. Pegylated interferon alfa-2a monotherapy is only indicated for the treatment of patients with CHC with compensated liver disease if there are contraindications or significant intolerance to other HCV antiviral drugs. | ||
* Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other HCV antiviral drugs. | * Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other HCV antiviral drugs. | ||
=====Chronic Hepatitis B (CHB)===== | =====Chronic Hepatitis B (CHB)===== | ||
* Pegylated interferon alfa-2a is indicated for the treatment of adult patients with HBeAg-positive and HBeAg-negative chronic hepatitis B infection who have compensated liver disease and evidence of viral replication and liver inflammation. | * Pegylated interferon alfa-2a is indicated for the treatment of adult patients with HBeAg-positive and HBeAg-negative chronic hepatitis B infection who have compensated liver disease and evidence of viral replication and liver inflammation. | ||
* Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other HCV antiviral drugs. | * Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other [[HCV]] antiviral drugs. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Pegylated interferon alfa-2a in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Pegylated interferon alfa-2a in adult patients. | ||
|offLabelAdultNoGuideSupport=* Chronic hepatitis C virus infection in patients who previously failed or relapsed after treatment with a nonpegylated interferon with or without ribavirin | |offLabelAdultNoGuideSupport=* Chronic hepatitis C virus infection in patients who previously failed or relapsed after treatment with a nonpegylated interferon with or without ribavirin | ||
| Line 25: | Line 25: | ||
|offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Pegylated interferon alfa-2a in pediatric patients. | |offLabelPedNoGuideSupport=There is limited information regarding <i>Off-Label Non–Guideline-Supported Use</i> of Pegylated interferon alfa-2a in pediatric patients. | ||
|contraindications=Pegylated interferon alfa-2a is contraindicated in patients with: | |contraindications=Pegylated interferon alfa-2a is contraindicated in patients with: | ||
* Known hypersensitivity reactions such as urticaria, angioedema, bronchoconstriction, anaphylaxis, or Stevens-Johnson syndrome to alpha interferons, including Pegylated interferon alfa-2a, or any of its components. | * Known [[hypersensitivity reactions]] such as [[urticaria]], [[angioedema]], [[bronchoconstriction]], [[anaphylaxis]], or [[Stevens-Johnson syndrome]] to alpha interferons, including Pegylated interferon alfa-2a, or any of its components. | ||
* Autoimmune hepatitis | * [[Autoimmune hepatitis]] | ||
* Hepatic decompensation (Child-Pugh score greater than 6 [class B and C]) in cirrhotic patients before treatment | * Hepatic decompensation (Child-Pugh score greater than 6 [class B and C]) in [[cirrhotic]] patients before treatment | ||
* Hepatic decompensation with Child-Pugh score greater than or equal to 6 in cirrhotic CHC patients coinfected with HIV before treatment | * Hepatic decompensation with Child-Pugh score greater than or equal to 6 in cirrhotic CHC patients coinfected with HIV before treatment | ||
Pegylated interferon alfa-2a is contraindicated in neonates and infants because it contains benzyl alcohol. Benzyl alcohol is associated with an increased incidence of neurologic and other complications which are sometimes fatal in neonates and infants. | Pegylated interferon alfa-2a is contraindicated in neonates and infants because it contains benzyl alcohol. Benzyl alcohol is associated with an increased incidence of neurologic and other complications which are sometimes fatal in neonates and infants. | ||
| Line 38: | Line 38: | ||
=====Neuropsychiatric Reactions===== | =====Neuropsychiatric Reactions===== | ||
Life-threatening or fatal neuropsychiatric reactions may manifest in all patients receiving therapy with Pegylated interferon alfa-2a and include suicide, suicidal ideation, homicidal ideation, depression, relapse of drug addiction, and drug overdose. These reactions may occur in patients with and without previous psychiatric illness. | Life-threatening or fatal [[neuropsychiatric reactions]] may manifest in all patients receiving therapy with Pegylated interferon alfa-2a and include [[suicide]], [[suicidal ideation]], [[homicidal ideation]], [[depression]], relapse of drug addiction, and [[drug overdose]]. These reactions may occur in patients with and without previous psychiatric illness. | ||
Pegylated interferon alfa-2a should be used with extreme caution in all patients who report a history of depression. Neuropsychiatric adverse events observed with alpha interferon treatment include aggressive behavior, psychoses, hallucinations, bipolar disorders, and mania. Physicians should monitor all patients for evidence of depression and other psychiatric symptoms. Patients should be advised to report any sign or symptom of depression or suicidal ideation to their prescribing physicians. In severe cases, therapy should be stopped immediately and psychiatric intervention instituted. | Pegylated interferon alfa-2a should be used with extreme caution in all patients who report a history of depression. Neuropsychiatric adverse events observed with alpha interferon treatment include [[aggressive behavior]], [[psychoses]], [[hallucinations]], [[bipolar disorders]], and [[mania]]. Physicians should monitor all patients for evidence of depression and other psychiatric symptoms. Patients should be advised to report any sign or symptom of [[depression]]] or suicidal ideation to their prescribing physicians. In severe cases, therapy should be stopped immediately and psychiatric intervention instituted. | ||
=====Cardiovascular Disorders===== | =====Cardiovascular Disorders===== | ||
Hypertension, supraventricular arrhythmias, chest pain, and myocardial infarction have been observed in patients treated with Pegylated interferon alfa-2a. Pegylated interferon alfa-2a should be administered with caution to patients with pre-existing cardiac disease. Because cardiac disease may be worsened by ribavirin-induced anemia, patients with a history of significant or unstable cardiac disease should not receive Pegylated interferon alfa-2a/ribavirin. | [[Hypertension]], [[supraventricular arrhythmias]], [[chest pain]], and [[myocardial infarction]] have been observed in patients treated with Pegylated interferon alfa-2a. Pegylated interferon alfa-2a should be administered with caution to patients with pre-existing cardiac disease. Because cardiac disease may be worsened by ribavirin-induced [[anemia]], patients with a history of significant or unstable cardiac disease should not receive Pegylated interferon alfa-2a/ribavirin. | ||
=====Bone Marrow Suppression===== | =====Bone Marrow Suppression===== | ||
Pegylated interferon alfa-2a suppresses bone marrow function and may result in severe cytopenias. Ribavirin may potentiate the neutropenia and lymphopenia induced by alpha interferons including Pegylated interferon alfa-2a. Very rarely, alpha interferons may be associated with aplastic anemia. It is advised that complete blood counts (CBC) be obtained pre-treatment and monitored routinely during therapy. | Pegylated interferon alfa-2a suppresses bone marrow function and may result in severe [[cytopenias]]. Ribavirin may potentiate the [[neutropenia]] and [[lymphopenia]] induced by alpha interferons including Pegylated interferon alfa-2a. Very rarely, alpha interferons may be associated with [[aplastic anemia]]. It is advised that complete blood counts (CBC) be obtained pre-treatment and monitored routinely during therapy. | ||
Pegylated interferon alfa-2a/ribavirin should be used with caution in patients with baseline neutrophil counts less than 1,500 cells/mm3, with baseline platelet counts less than 90,000 cells/mm3 or baseline hemoglobin less than 10 g/dL. Pegylated interferon alfa-2a therapy should be discontinued, at least temporarily, in patients who develop severe decreases in neutrophil and/or platelet counts. | Pegylated interferon alfa-2a/ribavirin should be used with caution in patients with baseline neutrophil counts less than 1,500 cells/mm3, with baseline platelet counts less than 90,000 cells/mm3 or baseline hemoglobin less than 10 g/dL. Pegylated interferon alfa-2a therapy should be discontinued, at least temporarily, in patients who develop severe decreases in neutrophil and/or platelet counts. | ||
Severe neutropenia and thrombocytopenia occur with a greater incidence in HIV coinfected patients than monoinfected patients and may result in serious infections or bleeding. | Severe [[neutropenia]] and [[thrombocytopenia]] occur with a greater incidence in HIV coinfected patients than monoinfected patients and may result in [[serious infections]] or [[bleeding]]. | ||
Pancytopenia (marked decreases in RBCs, neutrophils and platelets) and bone marrow suppression have been reported in the literature to occur within 3 to 7 weeks after the concomitant administration of pegylated interferon/ribavirin and azathioprine. In this limited number of patients (n=8), myelotoxicity was reversible within 4 to 6 weeks upon withdrawal of both HCV antiviral therapy and concomitant azathioprine and did not recur upon reintroduction of either treatment alone. Pegylated interferon alfa-2a, ribavirin, and azathioprine should be discontinued for pancytopenia, and pegylated interferon/ribavirin should not be re-introduced with concomitant azathioprine. | Pancytopenia (marked decreases in RBCs, neutrophils and platelets) and bone marrow suppression have been reported in the literature to occur within 3 to 7 weeks after the concomitant administration of pegylated interferon/ribavirin and azathioprine. In this limited number of patients (n=8), [[myelotoxicity]] was reversible within 4 to 6 weeks upon withdrawal of both HCV antiviral therapy and concomitant azathioprine and did not recur upon reintroduction of either treatment alone. Pegylated interferon alfa-2a, ribavirin, and azathioprine should be discontinued for pancytopenia, and pegylated interferon/ribavirin should not be re-introduced with concomitant azathioprine. | ||
=====Autoimmune Disorders===== | =====Autoimmune Disorders===== | ||
Development or exacerbation of autoimmune disorders including myositis, hepatitis, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, psoriasis, rheumatoid arthritis, interstitial nephritis, thyroiditis, and systemic lupus erythematosus have been reported in patients receiving alpha interferon. Pegylated interferon alfa-2a should be used with caution in patients with autoimmune disorders. | Development or exacerbation of autoimmune disorders including [[myositis]], [[hepatitis]], [[thrombotic thrombocytopenic purpura]], [[idiopathic thrombocytopenic purpura]], [[psoriasis]], [[rheumatoid arthritis]], [[interstitial nephritis]], [[thyroiditis]], and [[systemic lupus erythematosus]] have been reported in patients receiving alpha interferon. Pegylated interferon alfa-2a should be used with caution in patients with autoimmune disorders. | ||
=====Endocrine Disorders===== | =====Endocrine Disorders===== | ||
| Line 61: | Line 61: | ||
=====Ophthalmologic Disorders===== | =====Ophthalmologic Disorders===== | ||
Decrease or loss of vision, retinopathy including macular edema, retinal artery or vein thrombosis, retinal hemorrhages and cotton wool spots, optic neuritis, papilledema and serous retinal detachment are induced or aggravated by treatment with Pegylated interferon alfa-2a or other alpha interferons. All patients should receive an eye examination at baseline. Patients with pre-existing ophthalmologic disorders (e.g., diabetic or hypertensive retinopathy) should receive periodic ophthalmologic exams during interferon alpha treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. Pegylated interferon alfa-2a treatment should be discontinued in patients who develop new or worsening ophthalmologic disorders. | Decrease or loss of vision, retinopathy including [[macular edema]], [[retinal artery]] or [[vein thrombosis]], [[retinal hemorrhages]] and [[cotton wool spots]], [[optic neuritis]], [[papilledema]] and [[serous retinal detachment]] are induced or aggravated by treatment with Pegylated interferon alfa-2a or other alpha interferons. All patients should receive an eye examination at baseline. Patients with pre-existing ophthalmologic disorders (e.g., diabetic or [[hypertensive retinopathy]]) should receive periodic ophthalmologic exams during interferon alpha treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. Pegylated interferon alfa-2a treatment should be discontinued in patients who develop new or worsening ophthalmologic disorders. | ||
=====Cerebrovascular Disorders===== | =====Cerebrovascular Disorders===== | ||
Ischemic and hemorrhagic cerebrovascular events have been observed in patients treated with interferon alfa-based therapies, including Pegylated interferon alfa-2a. Events occurred in patients with few or no reported risk factors for stroke, including patients less than 45 years of age. Because these are spontaneous reports, estimates of frequency cannot be made and a causal relationship between interferon alfa-based therapies and these events is difficult to establish. | Ischemic and [[hemorrhagic cerebrovascular events]] have been observed in patients treated with interferon alfa-based therapies, including Pegylated interferon alfa-2a. Events occurred in patients with few or no reported risk factors for [[stroke]], including patients less than 45 years of age. Because these are spontaneous reports, estimates of frequency cannot be made and a causal relationship between interferon alfa-based therapies and these events is difficult to establish. | ||
=====Hepatic Failure and Hepatitis Exacerbations===== | =====Hepatic Failure and Hepatitis Exacerbations===== | ||
Chronic hepatitis C (CHC) patients with cirrhosis may be at risk of hepatic decompensation and death when treated with alpha interferons, including Pegylated interferon alfa-2a. Cirrhotic CHC patients coinfected with HIV receiving highly active antiretroviral therapy (HAART) and interferon alfa-2a with or without ribavirin appear to be at increased risk for the development of hepatic decompensation compared to patients not receiving HAART. In Study 7 | Chronic hepatitis C ([[CHC]]) patients with cirrhosis may be at risk of hepatic decompensation and death when treated with alpha interferons, including Pegylated interferon alfa-2a. Cirrhotic CHC patients coinfected with HIV receiving highly active antiretroviral therapy (HAART) and interferon alfa-2a with or without ribavirin appear to be at increased risk for the development of hepatic decompensation compared to patients not receiving HAART. In Study 7}, among 129 CHC/HIV cirrhotic subjects receiving HAART, 14 (11%) of these subjects across all treatment arms developed hepatic decompensation resulting in 6 deaths. All 14 subjects were on NRTIs, including stavudine, didanosine, abacavir, zidovudine, and lamivudine. These small numbers of patients do not permit discrimination between specific NRTIs for the associated risk. During treatment, patients' clinical status and hepatic function should be closely monitored, and Pegylated interferon alfa-2a/ribavirin treatment should be immediately discontinued in patients with hepatic decompensation. | ||
Exacerbations of hepatitis during hepatitis B therapy are not uncommon and are characterized by transient and potentially severe increases in serum ALT. Chronic hepatitis B subjects experienced transient acute exacerbations (flares) of hepatitis B (ALT elevation greater than 10-fold higher than the upper limit of normal) during Pegylated interferon alfa-2a treatment (12% and 18%) and post-treatment (7% and 12%) in HBeAg negative and HBeAg positive subjects, respectively. Marked transaminase flares while on Pegylated interferon alfa-2a therapy have been accompanied by other liver test abnormalities. Patients experiencing ALT flares should receive more frequent monitoring of liver function. Pegylated interferon alfa-2a dose reduction should be considered in patients experiencing transaminase flares. If ALT increases are progressive despite reduction of Pegylated interferon alfa-2a dose or are accompanied by increased bilirubin or evidence of hepatic decompensation, Pegylated interferon alfa-2a should be immediately discontinued. | Exacerbations of hepatitis during hepatitis B therapy are not uncommon and are characterized by transient and potentially severe increases in serum ALT. Chronic hepatitis B subjects experienced transient acute exacerbations (flares) of hepatitis B (ALT elevation greater than 10-fold higher than the upper limit of normal) during Pegylated interferon alfa-2a treatment (12% and 18%) and post-treatment (7% and 12%) in HBeAg negative and HBeAg positive subjects, respectively. Marked transaminase flares while on Pegylated interferon alfa-2a therapy have been accompanied by other liver test abnormalities. Patients experiencing ALT flares should receive more frequent monitoring of liver function. Pegylated interferon alfa-2a dose reduction should be considered in patients experiencing transaminase flares. If ALT increases are progressive despite reduction of Pegylated interferon alfa-2a dose or are accompanied by increased bilirubin or evidence of hepatic decompensation, Pegylated interferon alfa-2a should be immediately discontinued. | ||
=====Pulmonary Disorders===== | =====Pulmonary Disorders===== | ||
Dyspnea, pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension and sarcoidosis, some resulting in respiratory failure and/or patient deaths, may be induced or aggravated by Pegylated interferon alfa-2a or alpha interferon therapy. Recurrence of respiratory failure has been observed with interferon rechallenge. Pegylated interferon alfa-2a combination treatment should be suspended in patients who develop pulmonary infiltrates or pulmonary function impairment. Patients who resume interferon treatment should be closely monitored. | [[Dyspnea]], pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension and sarcoidosis, some resulting in respiratory failure and/or patient deaths, may be induced or aggravated by Pegylated interferon alfa-2a or alpha interferon therapy. Recurrence of respiratory failure has been observed with interferon rechallenge. Pegylated interferon alfa-2a combination treatment should be suspended in patients who develop pulmonary infiltrates or pulmonary function impairment. Patients who resume interferon treatment should be closely monitored. | ||
=====Infections===== | =====Infections===== | ||
| Line 250: | Line 250: | ||
|administration=Subcutaneous | |administration=Subcutaneous | ||
|overdose=There is limited experience with overdosage. The maximum dose received by any patient was 7 times the intended dose of Pegylated interferon alfa-2a (180 mcg/day for 7 days). There were no serious reactions attributed to overdosages. Weekly doses of up to 630 mcg have been administered to patients with cancer. Dose-limiting toxicities were fatigue, elevated liver enzymes, neutropenia, and thrombocytopenia. There is no specific antidote for Pegylated interferon alfa-2a. Hemodialysis and peritoneal dialysis are not effective. | |overdose=There is limited experience with overdosage. The maximum dose received by any patient was 7 times the intended dose of Pegylated interferon alfa-2a (180 mcg/day for 7 days). There were no serious reactions attributed to overdosages. Weekly doses of up to 630 mcg have been administered to patients with cancer. Dose-limiting toxicities were fatigue, elevated liver enzymes, neutropenia, and thrombocytopenia. There is no specific antidote for Pegylated interferon alfa-2a. Hemodialysis and peritoneal dialysis are not effective. | ||
|drugBox={{Drugbox2 | |||
| Verifiedfields = changed | |||
| verifiedrevid = 470447710 | |||
| IUPAC_name = PEGylated human interferon alpha 2b | |||
| image = | |||
<!--Clinical data--> | |||
| tradename = | |||
| Drugs.com = {{drugs.com|CDI|peginterferon_alfa-2b}} | |||
| MedlinePlus = a605030 | |||
| pregnancy_AU = <!-- A / B1 / B2 / B3 / C / D / X --> | |||
| pregnancy_US = <!-- A / B / C / D / X --> | |||
| pregnancy_category = contraindicated<ref>http://www.fda.gov/downloads/Drugs/DrugSafety/UCM133677.pdf See line 27</ref> | |||
| legal_AU = <!-- Unscheduled / S2 / S4 / S8 --> | |||
| legal_UK = <!-- GSL / P / POM / CD --> | |||
| legal_US = <!-- OTC / Rx-only --> | |||
| legal_status = | |||
| routes_of_administration = | |||
<!--Pharmacokinetic data--> | |||
| bioavailability = | |||
| protein_bound = | |||
| metabolism = | |||
| elimination_half-life = 22–60 hrs | |||
| excretion = | |||
<!--Identifiers--> | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 99210-65-8 | |||
| ATC_prefix = L03 | |||
| ATC_suffix = AB10 | |||
| PubChem = | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00022 | |||
| UNII_Ref = {{fdacite|changed|FDA}} | |||
| UNII = G8RGG88B68 | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D02745 | |||
| ChEMBL_Ref = {{ebicite|changed|EBI}} | |||
| ChEMBL = 1201561 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = NA | |||
<!--Chemical data--> | |||
| C=860 | H=1353 | N=229 | O=255 | S=9 | |||
| molecular_weight = 19269.1 g/mol | |||
}} | |||
|mechAction=The biological activity of Pegylated interferon alfa-2a is derived from its recombinant human interferon α-2a moiety. Peginterferon α-2a binds to the human type 1 interferon receptor leading to receptor dimerization. Receptor dimerization activates multiple intracellular signal transduction pathways initially mediated by the JAK/STAT pathway. Given the diversity of cell types that respond to interferon α-2a, and the multiplicity of potential intracellular responses to interferon receptor activation, peginterferon α-2a is expected to have pleiotropic biological effects in the body. | |mechAction=The biological activity of Pegylated interferon alfa-2a is derived from its recombinant human interferon α-2a moiety. Peginterferon α-2a binds to the human type 1 interferon receptor leading to receptor dimerization. Receptor dimerization activates multiple intracellular signal transduction pathways initially mediated by the JAK/STAT pathway. Given the diversity of cell types that respond to interferon α-2a, and the multiplicity of potential intracellular responses to interferon receptor activation, peginterferon α-2a is expected to have pleiotropic biological effects in the body. | ||
|structure=Peginterferon alfa-2a has an approximate molecular weight of 60,000 daltons. | |structure=Peginterferon alfa-2a has an approximate molecular weight of 60,000 daltons. | ||
Latest revision as of 22:06, 4 February 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Gloria Picoy [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
Risk of Serious Disorders
See full prescribing information for complete Boxed Warning.
Alpha interferons may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping Pegylated interferon alfa-2a therapy.
|
Overview
Pegylated interferon alfa-2a is an alfa interferon that is FDA approved for the treatment of chronic hepatitis C (CHC) and chronic hepatitis B (CHB). There is a Black Box Warning for this drug as shown here. Common adverse reactions include fatigue/asthenia, pyrexia, myalgia and headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Chronic Hepatitis C
- Pegylated interferon alfa-2a, as part of a combination regimen with other hepatitis C virus (HCV) antiviral drugs, is indicated for the treatment of adults with chronic hepatitis C (CHC) with compensated liver disease. Pegylated interferon alfa-2a monotherapy is only indicated for the treatment of patients with CHC with compensated liver disease if there are contraindications or significant intolerance to other HCV antiviral drugs.
- Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other HCV antiviral drugs.
Chronic Hepatitis B (CHB)
- Pegylated interferon alfa-2a is indicated for the treatment of adult patients with HBeAg-positive and HBeAg-negative chronic hepatitis B infection who have compensated liver disease and evidence of viral replication and liver inflammation.
- Dosage: 180 mcg per week and the duration of treatment depends on indication, genotype, and whether it is administered with other HCV antiviral drugs.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pegylated interferon alfa-2a in adult patients.
Non–Guideline-Supported Use
- Chronic hepatitis C virus infection in patients who previously failed or relapsed after treatment with a nonpegylated interferon with or without ribavirin
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Chronic Hepatitis C
- Pegylated interferon alfa-2a in combination with ribavirin is indicated for treatment of pediatric patients 5 years of age and older with CHC and compensated liver disease.
- Dosage: 180 mcg/1.73 m2 × BSA per week, in combination with ribavirin, and the duration of treatment depends on genotype.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Pegylated interferon alfa-2a in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Pegylated interferon alfa-2a in pediatric patients.
Contraindications
Pegylated interferon alfa-2a is contraindicated in patients with:
- Known hypersensitivity reactions such as urticaria, angioedema, bronchoconstriction, anaphylaxis, or Stevens-Johnson syndrome to alpha interferons, including Pegylated interferon alfa-2a, or any of its components.
- Autoimmune hepatitis
- Hepatic decompensation (Child-Pugh score greater than 6 [class B and C]) in cirrhotic patients before treatment
- Hepatic decompensation with Child-Pugh score greater than or equal to 6 in cirrhotic CHC patients coinfected with HIV before treatment
Pegylated interferon alfa-2a is contraindicated in neonates and infants because it contains benzyl alcohol. Benzyl alcohol is associated with an increased incidence of neurologic and other complications which are sometimes fatal in neonates and infants.
When Pegylated interferon alfa-2a is used in combination with other HCV antiviral drugs, the contraindications applicable to those agents are applicable to combination therapies. Pegylated interferon alfa-2a combination treatment with ribavirin is contraindicated in women who are pregnant and men whose female partners are pregnant.
Refer to the prescribing information of the other HCV antiviral drugs, including ribavirin, for a list of their contraindications.
Warnings
|
Risk of Serious Disorders
See full prescribing information for complete Boxed Warning.
Alpha interferons may cause or aggravate fatal or life-threatening neuropsychiatric, autoimmune, ischemic, and infectious disorders. Patients should be monitored closely with periodic clinical and laboratory evaluations. Therapy should be withdrawn in patients with persistently severe or worsening signs or symptoms of these conditions. In many, but not all cases, these disorders resolve after stopping Pegylated interferon alfa-2a therapy.
|
Pregnancy: Use with Ribavirin
Ribavirin may cause birth defects and/or death of the exposed fetus. Patients must avoid pregnancy (female patients or female partners of male patients) while taking Pegylated interferon alfa-2a and ribavirin combination therapy. Ribavirin therapy should not be started unless a confirmed negative pregnancy test has been obtained immediately prior to initiation of therapy. Women of childbearing potential and men must use two forms of effective contraception during treatment and for at least 6 months after treatment has concluded. Routine monthly pregnancy tests must be performed during this time.
Neuropsychiatric Reactions
Life-threatening or fatal neuropsychiatric reactions may manifest in all patients receiving therapy with Pegylated interferon alfa-2a and include suicide, suicidal ideation, homicidal ideation, depression, relapse of drug addiction, and drug overdose. These reactions may occur in patients with and without previous psychiatric illness.
Pegylated interferon alfa-2a should be used with extreme caution in all patients who report a history of depression. Neuropsychiatric adverse events observed with alpha interferon treatment include aggressive behavior, psychoses, hallucinations, bipolar disorders, and mania. Physicians should monitor all patients for evidence of depression and other psychiatric symptoms. Patients should be advised to report any sign or symptom of depression] or suicidal ideation to their prescribing physicians. In severe cases, therapy should be stopped immediately and psychiatric intervention instituted.
Cardiovascular Disorders
Hypertension, supraventricular arrhythmias, chest pain, and myocardial infarction have been observed in patients treated with Pegylated interferon alfa-2a. Pegylated interferon alfa-2a should be administered with caution to patients with pre-existing cardiac disease. Because cardiac disease may be worsened by ribavirin-induced anemia, patients with a history of significant or unstable cardiac disease should not receive Pegylated interferon alfa-2a/ribavirin.
Bone Marrow Suppression
Pegylated interferon alfa-2a suppresses bone marrow function and may result in severe cytopenias. Ribavirin may potentiate the neutropenia and lymphopenia induced by alpha interferons including Pegylated interferon alfa-2a. Very rarely, alpha interferons may be associated with aplastic anemia. It is advised that complete blood counts (CBC) be obtained pre-treatment and monitored routinely during therapy.
Pegylated interferon alfa-2a/ribavirin should be used with caution in patients with baseline neutrophil counts less than 1,500 cells/mm3, with baseline platelet counts less than 90,000 cells/mm3 or baseline hemoglobin less than 10 g/dL. Pegylated interferon alfa-2a therapy should be discontinued, at least temporarily, in patients who develop severe decreases in neutrophil and/or platelet counts.
Severe neutropenia and thrombocytopenia occur with a greater incidence in HIV coinfected patients than monoinfected patients and may result in serious infections or bleeding.
Pancytopenia (marked decreases in RBCs, neutrophils and platelets) and bone marrow suppression have been reported in the literature to occur within 3 to 7 weeks after the concomitant administration of pegylated interferon/ribavirin and azathioprine. In this limited number of patients (n=8), myelotoxicity was reversible within 4 to 6 weeks upon withdrawal of both HCV antiviral therapy and concomitant azathioprine and did not recur upon reintroduction of either treatment alone. Pegylated interferon alfa-2a, ribavirin, and azathioprine should be discontinued for pancytopenia, and pegylated interferon/ribavirin should not be re-introduced with concomitant azathioprine.
Autoimmune Disorders
Development or exacerbation of autoimmune disorders including myositis, hepatitis, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura, psoriasis, rheumatoid arthritis, interstitial nephritis, thyroiditis, and systemic lupus erythematosus have been reported in patients receiving alpha interferon. Pegylated interferon alfa-2a should be used with caution in patients with autoimmune disorders.
Endocrine Disorders
Pegylated interferon alfa-2a causes or aggravates hypothyroidism and hyperthyroidism. Hyperglycemia, hypoglycemia, and diabetes mellitus have been observed to develop in patients treated with Pegylated interferon alfa-2a. Patients with these conditions at baseline who cannot be effectively treated by medication should not begin Pegylated interferon alfa-2a therapy. Patients who develop these conditions during treatment and cannot be controlled with medication may require discontinuation of Pegylated interferon alfa-2a therapy.
Ophthalmologic Disorders
Decrease or loss of vision, retinopathy including macular edema, retinal artery or vein thrombosis, retinal hemorrhages and cotton wool spots, optic neuritis, papilledema and serous retinal detachment are induced or aggravated by treatment with Pegylated interferon alfa-2a or other alpha interferons. All patients should receive an eye examination at baseline. Patients with pre-existing ophthalmologic disorders (e.g., diabetic or hypertensive retinopathy) should receive periodic ophthalmologic exams during interferon alpha treatment. Any patient who develops ocular symptoms should receive a prompt and complete eye examination. Pegylated interferon alfa-2a treatment should be discontinued in patients who develop new or worsening ophthalmologic disorders.
Cerebrovascular Disorders
Ischemic and hemorrhagic cerebrovascular events have been observed in patients treated with interferon alfa-based therapies, including Pegylated interferon alfa-2a. Events occurred in patients with few or no reported risk factors for stroke, including patients less than 45 years of age. Because these are spontaneous reports, estimates of frequency cannot be made and a causal relationship between interferon alfa-based therapies and these events is difficult to establish.
Hepatic Failure and Hepatitis Exacerbations
Chronic hepatitis C (CHC) patients with cirrhosis may be at risk of hepatic decompensation and death when treated with alpha interferons, including Pegylated interferon alfa-2a. Cirrhotic CHC patients coinfected with HIV receiving highly active antiretroviral therapy (HAART) and interferon alfa-2a with or without ribavirin appear to be at increased risk for the development of hepatic decompensation compared to patients not receiving HAART. In Study 7}, among 129 CHC/HIV cirrhotic subjects receiving HAART, 14 (11%) of these subjects across all treatment arms developed hepatic decompensation resulting in 6 deaths. All 14 subjects were on NRTIs, including stavudine, didanosine, abacavir, zidovudine, and lamivudine. These small numbers of patients do not permit discrimination between specific NRTIs for the associated risk. During treatment, patients' clinical status and hepatic function should be closely monitored, and Pegylated interferon alfa-2a/ribavirin treatment should be immediately discontinued in patients with hepatic decompensation.
Exacerbations of hepatitis during hepatitis B therapy are not uncommon and are characterized by transient and potentially severe increases in serum ALT. Chronic hepatitis B subjects experienced transient acute exacerbations (flares) of hepatitis B (ALT elevation greater than 10-fold higher than the upper limit of normal) during Pegylated interferon alfa-2a treatment (12% and 18%) and post-treatment (7% and 12%) in HBeAg negative and HBeAg positive subjects, respectively. Marked transaminase flares while on Pegylated interferon alfa-2a therapy have been accompanied by other liver test abnormalities. Patients experiencing ALT flares should receive more frequent monitoring of liver function. Pegylated interferon alfa-2a dose reduction should be considered in patients experiencing transaminase flares. If ALT increases are progressive despite reduction of Pegylated interferon alfa-2a dose or are accompanied by increased bilirubin or evidence of hepatic decompensation, Pegylated interferon alfa-2a should be immediately discontinued.
Pulmonary Disorders
Dyspnea, pulmonary infiltrates, pneumonia, bronchiolitis obliterans, interstitial pneumonitis, pulmonary hypertension and sarcoidosis, some resulting in respiratory failure and/or patient deaths, may be induced or aggravated by Pegylated interferon alfa-2a or alpha interferon therapy. Recurrence of respiratory failure has been observed with interferon rechallenge. Pegylated interferon alfa-2a combination treatment should be suspended in patients who develop pulmonary infiltrates or pulmonary function impairment. Patients who resume interferon treatment should be closely monitored.
Infections
While fever may be associated with the flu-like syndrome reported commonly during interferon therapy, other causes of high or persistent fever must be ruled out, particularly in patients with neutropenia. Serious and severe infections (bacterial, viral, or fungal), some fatal, have been reported during treatment with alpha interferons including Pegylated interferon alfa-2a. Appropriate anti-infective therapy should be started immediately and discontinuation of therapy should be considered.
Colitis
Ulcerative and hemorrhagic/ischemic colitis, sometimes fatal, have been observed within 12 weeks of starting alpha interferon treatment. Abdominal pain, bloody diarrhea, and fever are the typical manifestations of colitis. Pegylated interferon alfa-2a should be discontinued immediately if these symptoms develop. The colitis usually resolves within 1 to 3 weeks of discontinuation of alpha interferon.
Pancreatitis
Pancreatitis, sometimes fatal, has occurred during alpha interferon and ribavirin treatment. Pegylated interferon alfa-2a/ribavirin should be suspended if symptoms or signs suggestive of pancreatitis are observed. Pegylated interferon alfa-2a/ribavirin should be discontinued in patients diagnosed with pancreatitis.
Hypersensitivity
Severe acute hypersensitivity reactions (e.g., urticaria, angioedema, bronchoconstriction, and anaphylaxis) have been observed during alpha interferon and ribavirin therapy. If such reaction occurs, therapy with Pegylated interferon alfa-2a/ribavirin should be discontinued and appropriate medical therapy immediately instituted. Serious skin reactions including vesiculobullous eruptions, reactions in the spectrum of Stevens-Johnson Syndrome (erythema multiforme major) with varying degrees of skin and mucosal involvement and exfoliative dermatitis (erythroderma) have been reported in patients receiving Pegylated interferon alfa-2a with and without ribavirin. Patients developing signs or symptoms of severe skin reactions must discontinue therapy.
Impact on Growth in Pediatric Patients
Pediatric subjects treated with Pegylated interferon alfa-2a plus ribavirin combination therapy showed a delay in weight and height increases after 48 weeks of therapy compared with baseline. Both weight and height for age z-scores as well as the percentiles of the normative population for subject weight and height decreased during treatment. At the end of 2 years follow-up after treatment, most subjects had returned to baseline normative growth curve percentiles for weight and height (mean weight for age percentile was 64% at baseline and 60% at 2 years post-treatment; mean height percentile was 54% at baseline and 56% at 2 years post-treatment). At the end of treatment, 43% of subjects experienced a weight percentile decrease of 15 percentiles or more, and 25% experienced a height percentile decrease of 15 percentiles or more on the normative growth curves. At 2 years post-treatment, 16% of subjects remained 15 percentiles or more below their baseline weight curve and 11% remained 15 percentiles or more below their baseline height curve.
Peripheral Neuropathy
Peripheral neuropathy has been reported when alpha interferons were given in combination with telbivudine. In one clinical trial, an increased risk and severity of peripheral neuropathy was observed with the combination use of telbivudine and Pegylated interferon alfa-2a as compared to telbivudine alone. The safety and efficacy of telbivudine in combination with interferons for the treatment of chronic hepatitis B have not been demonstrated.
Laboratory Tests
Before beginning Pegylated interferon alfa-2a or Pegylated interferon alfa-2a combination therapy, standard hematological and biochemical laboratory tests are recommended for all patients. Pregnancy screening for women of childbearing potential must be performed. Patients who have pre-existing cardiac abnormalities should have electrocardiograms administered before treatment with Pegylated interferon alfa-2a/ribavirin.
After initiation of therapy, hematological tests should be performed at 2 weeks and 4 weeks and biochemical tests should be performed at 4 weeks. Additional testing should be performed periodically during therapy. In adult clinical studies, the CBC (including hemoglobin level and white blood cell and platelet counts) and chemistries (including liver function tests and uric acid) were measured at 1, 2, 4, 6, and 8 weeks, and then every 4 to 6 weeks or more frequently if abnormalities were found. In a pediatric clinical trial, hematological and chemistry assessments were at 1, 3, 5, and 8 weeks, then every 4 weeks. Thyroid stimulating hormone (TSH) was measured every 12 weeks. Monthly pregnancy testing should be performed during combination therapy and for 6 months after discontinuing therapy.
The entrance criteria used for the clinical studies of Pegylated interferon alfa-2a may be considered as a guideline to acceptable baseline values for initiation of treatment:
- Platelet count greater than or equal to 90,000 cells/mm3 (as low as 75,000 cells/mm3 in HCV subjects with cirrhosis or 70,000 cells/mm3 in subjects with CHC and HIV)
- Absolute neutrophil count (ANC) greater than or equal to 1,500 cells/mm3
- Serum creatinine concentration less than 1.5 × upper limit of normal
- TSH and T4 within normal limits or adequately controlled thyroid function
- CD4+ cell count greater than or equal to 200 cells/mm3 or CD4+ cell count greater than or equal to 100 cells/mm3 but less than 200 cells/mm3 and HIV-1 RNA less than 5,000 copies/mL in subjects coinfected with HIV
- Hemoglobin greater than or equal to 12 g/dL for women and greater than or equal to 13 g/dL for men in CHC monoinfected subjects
- Hemoglobin greater than or equal to 11 g/dL for women and greater than or equal to 12 g/dL for men in subjects with CHC and HIV
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying and controlled conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug, and may not reflect the rates observed in clinical practice.
Adult Subjects
In all hepatitis C studies, one or more serious adverse reactions occurred in 10% of CHC monoinfected subjects and in 19% of CHC/HIV subjects receiving Pegylated interferon alfa-2a alone or in combination with COPEGUS. The most common serious adverse reactions (3% in CHC and 5% in CHC/HIV) was bacterial infection (e.g., sepsis, osteomyelitis, endocarditis, pyelonephritis, pneumonia). Other SAEs occurred at a frequency of less than 1% and included: suicide, suicidal ideation, aggression, anxiety, drug abuse and drug overdose, angina, hepatic dysfunction, fatty liver, cholangitis, arrhythmia, diabetes mellitus, autoimmune phenomena (e.g., hyperthyroidism, hypothyroidism, sarcoidosis, systemic lupus erythematosus, rheumatoid arthritis), peripheral neuropathy, aplastic anemia, peptic ulcer, gastrointestinal bleeding, pancreatitis, colitis, corneal ulcer, pulmonary embolism, coma, myositis, cerebral hemorrhage, thrombotic thrombocytopenic purpura, psychotic disorder, and hallucination.
In clinical trials, 98 to 99 percent of subjects experienced one or more adverse reactions. For hepatitis C subjects, the most commonly reported adverse reactions were psychiatric reactions, including depression, insomnia, irritability, anxiety, and flu-like symptoms such as fatigue, pyrexia, myalgia, headache, and rigors. Other common reactions were anorexia, nausea and vomiting, diarrhea, arthralgias, injection site reactions, alopecia, and pruritus. TABLE 7 displays pooled rates of adverse reactions occurring in greater than 5% of subjects in the Pegylated interferon alfa-2a monotherapy and Pegylated interferon alfa-2a/COPEGUS combination therapy clinical trials.
Overall 11% of CHC monoinfected subjects receiving 48 weeks of therapy with Pegylated interferon alfa-2a either alone or in combination with COPEGUS discontinued therapy; 16% of CHC/HIV coinfected subjects discontinued therapy. The most common reasons for discontinuation of therapy were psychiatric, flu-like syndrome (e.g., lethargy, fatigue, headache), dermatologic and gastrointestinal disorders, and laboratory abnormalities (thrombocytopenia, neutropenia, and anemia).
Overall 39% of subjects with CHC or CHC/HIV required modification of Pegylated interferon alfa-2a and/or COPEGUS therapy. The most common reasons for dose modification of Pegylated interferon alfa-2a in CHC and CHC/HIV subjects was for neutropenia (20% and 27%, respectively) and thrombocytopenia (4% and 6%, respectively). The most common reason for dose modification of COPEGUS in CHC and CHC/HIV subjects was anemia (22% and 16%, respectively). Pegylated interferon alfa-2a dose was reduced in 12% of subjects receiving 1000 mg to 1200 mg COPEGUS for 48 weeks and in 7% of subjects receiving 800 mg COPEGUS for 24 weeks. COPEGUS dose was reduced in 21% of subjects receiving 1000 mg to 1200 mg COPEGUS for 48 weeks and in 12% of subjects receiving 800 mg COPEGUS for 24 weeks.
Chronic hepatitis C monoinfected subjects treated for 24 weeks with Pegylated interferon alfa-2a and 800 mg COPEGUS were observed to have lower incidence of serious adverse reactions (3% vs. 10%), Hgb less than 10 g/dL (3% vs. 15%), dose modification of Pegylated interferon alfa-2a (30% vs. 36%) and COPEGUS (19% vs. 38%) and of withdrawal from treatment (5% vs. 15%) compared to subjects treated for 48 weeks with Pegylated interferon alfa-2a and 1000 mg or 1200 mg COPEGUS. The overall incidence of adverse reactions appeared to be similar in the two treatment groups.

Pediatric Subjects
In a clinical trial with 114 pediatric subjects (5 to 17 years of age) treated with Pegylated interferon alfa-2a alone or in combination with COPEGUS, dose modifications were required in approximately one-third of subjects, most commonly for neutropenia and anemia. In general, the safety profile observed in pediatric subjects was similar to that seen in adults. In the pediatric study, the most prevalent adverse events in subjects treated with combination therapy for up to 48 weeks with Pegylated interferon alfa-2a and COPEGUS were influenza-like illness (91%), upper respiratory tract infection (60%), headache (64%), gastrointestinal disorder (56%), skin disorder (47%), and injection-site reaction (45%). Seven subjects receiving combination Pegylated interferon alfa-2a and COPEGUS treatment for 48 weeks discontinued therapy for safety reasons (depression, psychiatric evaluation abnormal, transient blindness, retinal exudates, hyperglycemia, type 1 diabetes mellitus, and anemia). Most of the adverse events reported in the study were mild or moderate in severity. Severe adverse events were reported in 2 subjects in the Pegylated interferon alfa-2a plus COPEGUS combination therapy group (hyperglycemia and cholecystectomy).
Growth inhibition was observed in pediatric subjects. During combination therapy for up to 48 weeks with Pegylated interferon alfa-2a and COPEGUS, negative changes in weight for age z-score and height for age z-score after 48 weeks of therapy compared with baseline were observed.
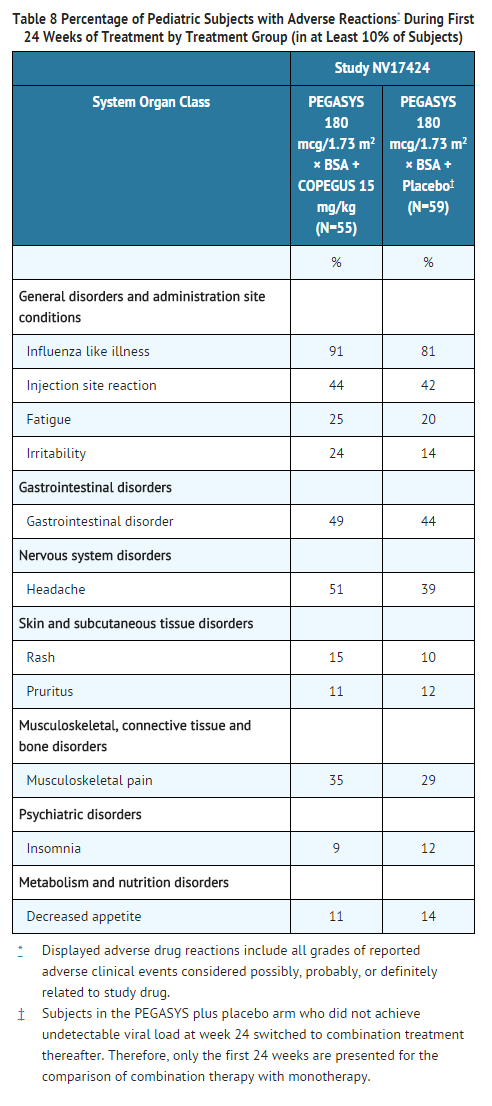
In pediatric subjects randomized to combination therapy, the incidence of most adverse reactions were similar for the entire treatment period (up to 48 weeks plus 24 weeks follow-up) in comparison to the first 24 weeks, and increased only slightly for headache, gastrointestinal disorder, irritability and rash. The majority of adverse reactions occurred in the first 24 weeks of treatment.
CHC with HIV Coinfection (Adults)
The adverse reaction profile of coinfected subjects treated with Pegylated interferon alfa-2a/COPEGUS in Study 7 was generally similar to that shown for monoinfected subjects in Study 4 (TABLE 7). Events occurring more frequently in coinfected subjects were neutropenia (40%), anemia (14%), thrombocytopenia (8%), weight decrease (16%), and mood alteration (9%).
Chronic Hepatitis B
In clinical trials of 48 week treatment duration, the adverse reaction profile of Pegylated interferon alfa-2a in chronic hepatitis B was similar to that seen in CHC Pegylated interferon alfa-2a monotherapy use, except for exacerbations of hepatitis [see WARNINGS AND PRECAUTIONS (5.9)]. Six percent of Pegylated interferon alfa-2a treated subjects in the hepatitis B studies experienced one or more serious adverse reactions.
The most common or important serious adverse reactions, all of which occurred at a frequency of less than or equal to 1%, in the hepatitis B studies were infections (sepsis, appendicitis, tuberculosis, influenza), hepatitis B flares, and thrombotic thrombocytopenic purpura.
One serious adverse reaction of anaphylactic shock occurred in a dose ranging study of 191 subjects in a subject taking a higher than the approved dose of Pegylated interferon alfa-2a.
The most commonly observed adverse reactions in the Pegylated interferon alfa-2a and lamivudine groups, respectively, were pyrexia (54% vs. 4%), headache (27% vs. 9%), fatigue (24% vs. 10%), myalgia (26% vs. 4%), alopecia (18% vs. 2%), and anorexia (16% vs. 3%).
Overall 5% of hepatitis B subjects discontinued Pegylated interferon alfa-2a therapy and 40% of subjects required modification of Pegylated interferon alfa-2a dose. The most common reason for dose modification in subjects receiving Pegylated interferon alfa-2a therapy was for laboratory abnormalities including neutropenia (20%), thrombocytopenia (13%), and ALT elevation (11%).
Laboratory Values
Adult Patients
The laboratory test values observed in the hepatitis B trials (except where noted below) were similar to those seen in the Pegylated interferon alfa-2a monotherapy CHC trials.
Neutrophils
In the hepatitis C studies, decreases in neutrophil count below normal were observed in 95% of all subjects treated with Pegylated interferon alfa-2a either alone or in combination with COPEGUS. Severe potentially life-threatening neutropenia (ANC less than 500 cells/mm3) occurred in 5% of CHC subjects and 12% of CHC/HIV subjects receiving Pegylated interferon alfa-2a either alone or in combination with COPEGUS. Modification of Pegylated interferon alfa-2a dose for neutropenia occurred in 17% of subjects receiving Pegylated interferon alfa-2a monotherapy and 22% of subjects receiving Pegylated interferon alfa-2a/COPEGUS combination therapy. In the CHC/HIV subjects 27% required modification of interferon dosage for neutropenia. Two percent of subjects with CHC and 10% of subjects with CHC/HIV required permanent reductions of Pegylated interferon alfa-2a dosage and less than 1% required permanent discontinuation. Median neutrophil counts return to pre-treatment levels 4 weeks after cessation of therapy.
Lymphocytes
Decreases in lymphocyte count are induced by interferon alpha therapy. Pegylated interferon alfa-2a plus COPEGUS combination therapy induced decreases in median total lymphocyte counts (56% in CHC and 40% in CHC/HIV, with median decrease of 1170 cells/mm3 in CHC and 800 cells/mm3 in CHC/HIV). In the hepatitis C studies, lymphopenia was observed during both monotherapy (81%) and combination therapy with Pegylated interferon alfa-2a and COPEGUS (91%). Severe lymphopenia (less than 500 cells/mm3) occurred in approximately 5% of all monotherapy subjects and 14% of all combination Pegylated interferon alfa-2a and COPEGUS therapy recipients. Dose adjustments were not required by protocol. The clinical significance of the lymphopenia is not known.
In CHC with HIV coinfection, CD4 counts decreased by 29% from baseline (median decrease of 137 cells/mm3) and CD8 counts decreased by 44% from baseline (median decrease of 389 cells/mm3) in the Pegylated interferon alfa-2a plus COPEGUS combination therapy arm. Median lymphocyte CD4 and CD8 counts return to pre-treatment levels after 4 to 12 weeks of the cessation of therapy. CD4% did not decrease during treatment.
Platelets
In the hepatitis C studies, platelet counts decreased in 52% of CHC subjects and 51% of CHC/HIV subjects treated with Pegylated interferon alfa-2a alone (respectively median decrease of 41% and 35% from baseline), and in 33% of CHC subjects and 47% of CHC/HIV subjects receiving combination therapy with COPEGUS (median decrease of 30% from baseline). Moderate to severe thrombocytopenia (less than 50,000 cells/mm3) was observed in 4% of CHC and 8% of CHC/HIV subjects. Median platelet counts return to pre-treatment levels 4 weeks after the cessation of therapy.
Hemoglobin
In the hepatitis C studies, the hemoglobin concentration decreased below 12 g/dL in 17% (median Hgb reduction of 2.2 g/dL) of monotherapy and 52% (median Hgb reduction of 3.7 g/dL) of combination therapy subjects. Severe anemia (Hgb less than 10 g/dL) was encountered in 13% of all subjects receiving combination therapy and in 2% of CHC subjects and 8% of CHC/HIV subjects receiving Pegylated interferon alfa-2a monotherapy. Dose modification for anemia in COPEGUS recipients treated for 48 weeks occurred in 22% of CHC subjects and 16% of CHC/HIV subjects.
Triglycerides
Triglyceride levels are elevated in subjects receiving alfa interferon therapy and were elevated in the majority of subjects participating in clinical studies receiving either Pegylated interferon alfa-2a alone or in combination with COPEGUS. Random levels greater than or equal to 400 mg/dL were observed in about 20% of CHC subjects. Severe elevations of triglycerides (greater than 1000 mg/dL) occurred in 2% of CHC monoinfected subjects.
In HCV/HIV coinfected subjects, fasting levels greater than or equal to 400 mg/dL were observed in up to 36% of subjects receiving either Pegylated interferon alfa-2a alone or in combination with COPEGUS. Severe elevations of triglycerides (greater than 1000 mg/dL) occurred in 7% of coinfected subjects.
ALT Elevations
Chronic Hepatitis C: One percent of subjects in the hepatitis C trials experienced marked elevations (5- to 10-fold above the upper limit of normal) in ALT levels during treatment and follow-up. These transaminase elevations were on occasion associated with hyperbilirubinemia and were managed by dose reduction or discontinuation of study treatment. Liver function test abnormalities were generally transient. One case was attributed to autoimmune hepatitis, which persisted beyond study medication discontinuation.
Chronic Hepatitis B:
Transient ALT elevations are common during hepatitis B therapy with Pegylated interferon alfa-2a. Twenty-five percent and 27% of subjects experienced elevations of 5 to 10 × ULN and 12% and 18% had elevations of greater than 10 × ULN during treatment of HBeAg negative and HBeAg positive disease, respectively. Flares have been accompanied by elevations of total bilirubin and alkaline phosphatase and less commonly with prolongation of PT and reduced albumin levels. Eleven percent of subjects had dose modifications due to ALT flares and less than 1% of subjects were withdrawn from treatment.
ALT flares of 5 to 10 × ULN occurred in 13% and 16% of subjects, while ALT flares of greater than 10 × ULN occurred in 7% and 12% of subjects in HBeAg negative and HBeAg positive disease, respectively, after discontinuation of Pegylated interferon alfa-2a therapy.
Thyroid Function
Pegylated interferon alfa-2a alone or in combination with COPEGUS was associated with the development of abnormalities in thyroid laboratory values, some with associated clinical manifestations. In the hepatitis C studies, hypothyroidism or hyperthyroidism requiring treatment, dose modification or discontinuation occurred in 4% and 1% of Pegylated interferon alfa-2a treated subjects and 4% and 2% of Pegylated interferon alfa-2a and COPEGUS treated subjects, respectively. Approximately half of the subjects, who developed thyroid abnormalities during Pegylated interferon alfa-2a treatment, still had abnormalities during the follow-up period.
Pediatric Patients
Decreases in hemoglobin, neutrophils and platelets may require dose reduction or permanent discontinuation from treatment [see DOSAGE AND ADMINISTRATION (2.3, 2.5)]. Most laboratory abnormalities noted during the clinical trial returned to baseline levels shortly after completion of treatment.
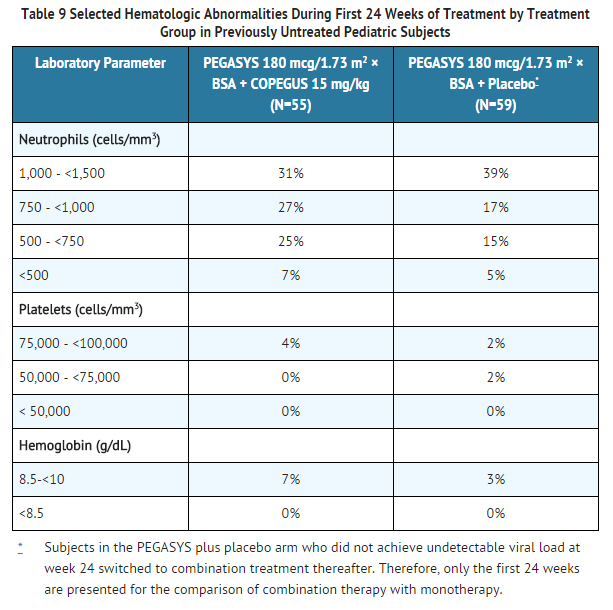
In patients randomized to combination therapy, the incidence of abnormalities during the entire treatment phase (up to 48 weeks plus 24 weeks follow-up) in comparison to the first 24 weeks increased slightly for neutrophils between 500 and 1,000 cells/mm³ and hemoglobin values between 8.5 and 10 g/dL. The majority of hematologic abnormalities occurred in the first 24 weeks of treatment.
Postmarketing Experience
The following adverse reactions have been identified and reported during post-approval use of Pegylated interferon alfa-2a therapy. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Blood and lymphatic system disorders: pure red cell aplasia
- Ear and labyrinth disorders: hearing impairment, hearing loss
- Immune system disorders: Liver graft rejection and renal graft rejection
- Metabolism and nutrition disorders: dehydration
- Skin and subcutaneous tissue disorders: serious skin reactions
- Neurological: seizures
Drug Interactions
Drugs Metabolized by Cytochrome P450
There was no effect on the pharmacokinetics of representative drugs metabolized by CYP 2C9, CYP 2C19, CYP 2D6 or CYP 3A4.
Treatment with Pegylated interferon alfa-2a once weekly for 4 weeks in healthy subjects was associated with an inhibition of P450 1A2 and a 25% increase in theophylline AUC.
Theophylline
Treatment with Pegylated interferon alfa-2a once weekly for 4 weeks in healthy subjects was associated with an inhibition of P450 1A2 and a 25% increase in theophylline AUC. Theophylline serum levels should be monitored and appropriate dose adjustments considered for patients given both theophylline and Pegylated interferon alfa-2a.
Methadone
In a PK study of HCV subjects concomitantly receiving methadone, treatment with Pegylated interferon alfa-2a once weekly for 4 weeks was associated with methadone levels that were 10% to 15% higher than at baseline. The clinical significance of this finding is unknown; however, patients should be monitored for the signs and symptoms of methadone toxicity.
The pharmacokinetics of concomitant administration of methadone and Pegylated interferon alfa-2a were evaluated in 24 Pegylated interferon alfa-2a naïve chronic hepatitis C (CHC) subjects (15 male, 9 female) who received 180 mcg Pegylated interferon alfa-2a subcutaneously weekly. All subjects were on stable methadone maintenance therapy (median dose 95 mg, range 30 mg to 150 mg) prior to receiving Pegylated interferon alfa-2a. Mean methadone PK parameters were 10% to 15% higher after 4 weeks of Pegylated interferon alfa-2a treatment as compared to baseline. Methadone did not significantly alter the PK of Pegylated interferon alfa-2a as compared to a PK study of 6 chronic hepatitis C subjects not receiving methadone.
Nucleoside Analogues
NRTIs
In Study 7 among the CHC/HIV coinfected cirrhotic subjects receiving NRTIs cases of hepatic decompensation (some fatal) were observed.
Patients receiving Pegylated interferon alfa-2a/ribavirin in combination with other HCV antiviral drugs and NRTIs should be closely monitored for treatment associated toxicities. Physicians should refer to prescribing information for other HCV antiviral drugs and the respective NRTIs for guidance regarding toxicity management. In addition, dose reduction or discontinuation of Pegylated interferon alfa-2a, ribavirin or both, should also be considered if worsening toxicities are observed.
Zidovudine
In Study 7, subjects who were administered zidovudine in combination with Pegylated interferon alfa-2a/COPEGUS developed severe neutropenia (ANC less than 500 cells/mm3) and severe anemia (hemoglobin less than 8 g/dL) more frequently than similar subjects not receiving zidovudine (neutropenia 15% vs. 9%) (anemia 5% vs. 1%). Discontinuation of zidovudine should be considered as medically appropriate. Dose reduction or discontinuation of Pegylated interferon alfa-2a, ribavirin or both should also be considered if worsening clinical toxicities are observed, including hepatic decompensation (e.g., Child-Pugh greater than 6).
Refer to the prescribing information for specific HCV antiviral drugs used in combination with Pegylated interferon alfa-2a for information on drug interaction potential.
Use in Specific Populations
Pregnancy
Pegylated interferon alfa-2a Monotherapy
Pegylated interferon alfa-2a has not been studied for its teratogenic effect. Non-pegylated interferon alfa-2a treatment of pregnant Rhesus monkeys at approximately 20 to 500 times the human weekly dose resulted in a statistically significant increase in abortions. No teratogenic effects were seen in the offspring delivered at term. Pegylated interferon alfa-2a should be assumed to have abortifacient potential. There are no adequate and well-controlled studies of Pegylated interferon alfa-2a in pregnant women. Pegylated interferon alfa-2a is to be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. Pegylated interferon alfa-2a is recommended for use in women of childbearing potential only when they are using effective contraception during therapy.
Use with Ribavirin
Pregnancy Category: X
Significant teratogenic and/or embryocidal effects have been demonstrated in all animal species exposed to ribavirin. Ribavirin therapy is contraindicated in women who are pregnant and in the male partners of women who are pregnant.
Pregnancy Category (AUS): B3
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Pegylated interferon alfa-2a in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Pegylated interferon alfa-2a during labor and delivery.
Nursing Mothers
It is not known whether peginterferon or its components are excreted in human milk. The effect of orally ingested peginterferon from breast milk on the nursing infant has not been evaluated. Because of the potential for adverse reactions from the drugs in nursing infants, a decision must be made whether to discontinue nursing or discontinue Pegylated interferon alfa-2a.
Pediatric Use
The safety and effectiveness of Pegylated interferon alfa-2a in patients below the age of 5 years have not been established.
Pegylated interferon alfa-2a contains benzyl alcohol. In neonates and infants, benzyl alcohol has been reported to be associated with an increased incidence of neurological and other complications which are sometimes fatal in neonates and infants.
Geriatic Use
Younger patients have higher virologic response rates than older patients. Clinical studies of Pegylated interferon alfa-2a alone or in combination with COPEGUS did not include sufficient numbers of subjects aged 65 or over to determine whether they respond differently from younger subjects. Adverse reactions related to alpha interferons, such as CNS, cardiac, and systemic (e.g., flu-like) effects may be more severe in the elderly and caution should be exercised in the use of Pegylated interferon alfa-2a in this population. Pegylated interferon alfa-2a is excreted by the kidney, and the risk of toxic reactions to this therapy may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function. Pegylated interferon alfa-2a should be used with caution in patients with creatinine clearance less than or equal to 50 mL/min. The dose of Pegylated interferon alfa-2a should be reduced for patients with creatinine clearance less than 30 mL/min.
Gender
Pegylated interferon alfa-2a administration yielded similar pharmacokinetics in male and female healthy subjects.
Race
There is no FDA guidance on the use of Pegylated interferon alfa-2a with respect to specific racial populations.
Renal Impairment
Renal function should be evaluated in all patients prior to initiation of Pegylated interferon alfa-2a by estimating the patient's creatinine clearance.
A clinical trial evaluated treatment with Pegylated interferon alfa-2a and COPEGUS in 50 CHC subjects with moderate (creatinine clearance 30 – 50 mL/min) or severe (creatinine clearance less than 30 mL/min) renal impairment or end stage renal disease (ESRD) requiring chronic hemodialysis (HD). In 18 subjects with ESRD receiving chronic HD, Pegylated interferon alfa-2a was administered at a dose of 135 mcg once weekly. Dose reductions and temporary interruptions of Pegylated interferon alfa-2a (due to Pegylated interferon alfa-2a-related adverse reactions, mainly anemia) were observed in up to 22% ESRD/HD subjects during treatment; and 17% of these subjects discontinued Pegylated interferon alfa-2a due to Pegylated interferon alfa-2a-related adverse reactions. Only one-third of ESRD/HD subjects received Pegylated interferon alfa-2a for 48 weeks. Subjects with severe (n=14) or moderate (n=17) renal impairment received Pegylated interferon alfa-2a 180 mcg once weekly. Pegylated interferon alfa-2a discontinuation rates were 36% and 0% in subjects with severe and moderate renal impairment, respectively, compared to 0% discontinuation rate in subjects with normal renal function.
Based on the pharmacokinetic and safety results from this trial, patients with creatinine clearance less than 30 mL/min should receive a reduced dose of Pegylated interferon alfa-2a. In addition, patients with any degree of renal impairment should be carefully monitored for laboratory abnormalities (especially decreased hemoglobin) and adverse reactions, and should undergo careful monitoring of creatinine clearance. Patients with clinically significant laboratory abnormalities or adverse reactions which are persistently severe or worsening should have therapy withdrawn. Refer to the prescribing information for specific HCV antiviral drugs used in combination with Pegylated interferon alfa-2a for information on use in patients with renal impairment.
Hepatic Impairment
Chronic hepatitis C (CHC) patients with cirrhosis may be at risk of hepatic decompensation and death when treated with alpha interferons, including Pegylated interferon alfa-2a. During treatment, patients' clinical status and hepatic function should be closely monitored, and Pegylated interferon alfa-2a treatment should be immediately discontinued if decompensation (Child-Pugh score greater than or equal to 6) is observed. Chronic hepatitis B subjects experienced transient acute exacerbations (flares) of hepatitis B (ALT elevation greater than 10-fold higher than the upper limit of normal) during Pegylated interferon alfa-2a treatment (12% and 18%) and post-treatment (7% and 12%) in HBeAg negative and HBeAg positive subjects, respectively.
Females of Reproductive Potential and Males
Pegylated interferon alfa-2a may impair fertility in women. Prolonged menstrual cycles and/or amenorrhea were observed in female cynomolgus monkeys given subcutaneous injections of 600 mcg/kg/dose (7200 mcg/m2/dose) of Pegylated interferon alfa-2a every other day for one month, at approximately 180 times the recommended weekly human dose for a 60 kg person (based on body surface area). Menstrual cycle irregularities were accompanied by both a decrease and delay in the peak 17β-estradiol and progesterone levels following administration of Pegylated interferon alfa-2a to female monkeys. A return to normal menstrual rhythm followed cessation of treatment. Every other day dosing with 100 mcg/kg (1200 mcg/m2) Pegylated interferon alfa-2a (equivalent to approximately 30 times the recommended human dose) had no effects on cycle duration or reproductive hormone status.
The effects of Pegylated interferon alfa-2a on male fertility have not been studied. However, no adverse effects on fertility were observed in male Rhesus monkeys treated with non-pegylated interferon alfa-2a for 5 months at doses up to 25 × 106 IU/kg/day.
Immunocompromised Patients
There is no FDA guidance one the use of Pegylated interferon alfa-2a in patients who are immunocompromised.
Organ Transplant Recipients
The safety and efficacy of Pegylated interferon alfa-2a treatment have not been established in patients with liver and other transplantations. As with other alpha interferons, liver and renal graft rejections have been reported on Pegylated interferon alfa-2a.
Chronic Hepatitis B
The safety and efficacy of Pegylated interferon alfa-2a have not been established in:
- Hepatitis B patients coinfected with HCV or HIV
- Hepatitis C patients coinfected with HBV or coinfected with HIV with a CD4+ cell count less than 100 cells/mm3.
Administration and Monitoring
Administration
Subcutaneous
Monitoring
There is limited information regarding Pegylated interferon alfa-2a Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Pegylated interferon alfa-2a and IV administrations.
Overdosage
There is limited experience with overdosage. The maximum dose received by any patient was 7 times the intended dose of Pegylated interferon alfa-2a (180 mcg/day for 7 days). There were no serious reactions attributed to overdosages. Weekly doses of up to 630 mcg have been administered to patients with cancer. Dose-limiting toxicities were fatigue, elevated liver enzymes, neutropenia, and thrombocytopenia. There is no specific antidote for Pegylated interferon alfa-2a. Hemodialysis and peritoneal dialysis are not effective.
Pharmacology
Pegylated interferon alfa-2a
| |
| Systematic (IUPAC) name | |
| PEGylated human interferon alpha 2b | |
| Identifiers | |
| CAS number | |
| ATC code | L03 |
| PubChem | ? |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 19269.1 g/mol |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | 22–60 hrs |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
contraindicated[1] |
| Legal status | |
| Routes | ? |
Mechanism of Action
The biological activity of Pegylated interferon alfa-2a is derived from its recombinant human interferon α-2a moiety. Peginterferon α-2a binds to the human type 1 interferon receptor leading to receptor dimerization. Receptor dimerization activates multiple intracellular signal transduction pathways initially mediated by the JAK/STAT pathway. Given the diversity of cell types that respond to interferon α-2a, and the multiplicity of potential intracellular responses to interferon receptor activation, peginterferon α-2a is expected to have pleiotropic biological effects in the body.
Structure
Peginterferon alfa-2a has an approximate molecular weight of 60,000 daltons.
Pharmacodynamics
Pegylated interferon alfa-2a stimulates the production of effector proteins such as serum neopterin and 2', 5'-oligoadenylate synthetase.
Pharmacokinetics
Maximal serum concentrations (Cmax) and AUC increased in a nonlinear dose related manner following administration of 90 to 270 mcg of Pegylated interferon alfa-2a. Maximal serum concentrations (Cmax) occur between 72 to 96 hours post-dose.
Week 48 mean trough concentrations (16 ng/mL; range 4 to 28) at 168 hours post-dose are approximately 2-fold higher than week 1 mean trough concentrations (9 ng/mL; range 0 to 15). Steady-state serum levels are reached within 5 to 8 weeks of once weekly dosing. The peak to trough ratio at week 48 is approximately 2. The mean systemic clearance in healthy subjects given Pegylated interferon alfa-2a was 94 mL/h, which is approximately 100-fold lower than that for interferon alfa-2a. The mean terminal half-life after subcutaneous dosing in subjects with chronic hepatitis C was 160 hours (range 84 to 353 hours) compared to 5 hours (range 3.7 to 8.5 hours) for ROFERON-A.
Nonclinical Toxicology
Antiviral Activity in Cell Culture
In the stable HCV cell culture model system (HCV replicon), PEG-IFN α-2a inhibited HCV RNA replication, with an EC50 value of 0.1-3 ng/mL. The combination of PEG-IFN α-2a and ribavirin was more effective at inhibiting HCV RNA replication than either agent alone.
Resistance
Different HCV genotypes display considerable clinical variability in their response to PEG-IFN-α and ribavirin therapy. Viral genetic determinants associated with the variable response have not been definitively identified.
Cross-resistance
Cross-resistance between IFN-α and ribavirin has not been observed.
Carcinogenesis
Pegylated interferon alfa-2a has not been tested for its carcinogenic potential.
Use with other HCV antiviral drugs: Refer to the prescribing information for specific antiviral drugs used in combination with Pegylated interferon alfa-2a for additional warnings.
Mutagenesis
Pegylated interferon alfa-2a did not cause DNA damage when tested in the Ames bacterial mutagenicity assay and in the in vitro chromosomal aberration assay in human lymphocytes, either in the presence or absence of metabolic activation.
Use with other HCV antiviral drugs: Refer to the prescribing information for specific HCV antiviral drugs used in combination with Pegylated interferon alfa-2a for additional warnings.
Clinical Studies
Chronic Hepatitis C Studies 1, 2, and 3: Pegylated interferon alfa-2a/COPEGUS Combination Therapy
Adult Patients
The safety and effectiveness of Pegylated interferon alfa-2a in combination with COPEGUS for the treatment of hepatitis C virus infection were assessed in two randomized controlled clinical trials. All subjects were adults, had compensated liver disease, detectable hepatitis C virus, liver biopsy diagnosis of chronic hepatitis, and were previously untreated with interferon. Approximately 20% of subjects in both studies had compensated cirrhosis (Child-Pugh class A). Subjects coinfected with HIV were excluded from these studies.
In Study 1, subjects were randomized to receive either Pegylated interferon alfa-2a 180 mcg subcutaneous once weekly with an oral placebo, Pegylated interferon alfa-2a 180 mcg once weekly with COPEGUS 1000 mg by mouth (body weight less than 75 kg) or 1200 mg by mouth (body weight greater than or equal to 75 kg) or Rebetron® (interferon alfa-2b 3 MIU subcutaneous three times a week plus ribavirin 1000 mg or 1200 mg by mouth). All subjects received 48 weeks of therapy followed by 24 weeks of treatment-free follow-up. COPEGUS or placebo treatment assignment was blinded. Sustained virological response was defined as undetectable (less than 50 IU/mL) HCV RNA on or after study week 68. Pegylated interferon alfa-2a in combination with COPEGUS resulted in a higher SVR compared to Pegylated interferon alfa-2a alone or interferon alfa-2b and ribavirin (TABLE 10). In all treatment arms, subjects with viral genotype 1, regardless of viral load, had a lower response rate.

In Study 2 (see TABLE 11), all subjects received Pegylated interferon alfa-2a 180 mcg subcutaneous once weekly and were randomized to treatment for either 24 or 48 weeks and to a COPEGUS dose of either 800 mg or 1000 mg/1200 mg (for body weight less than 75 kg/greater than or equal to 75 kg). Assignment to the four treatment arms was stratified by viral genotype and baseline HCV viral titer. Subjects with genotype 1 and high viral titer (defined as greater than 2 × 106 HCV RNA copies/mL serum) were preferentially assigned to treatment for 48 weeks.
HCV Genotypes
HCV 1 and 4 – Irrespective of baseline viral titer, treatment for 48 weeks with Pegylated interferon alfa-2a and 1000 mg or 1200 mg of COPEGUS resulted in higher SVR (defined as undetectable HCV RNA at the end of the 24-week treatment-free follow-up period) compared to shorter treatment (24 weeks) and/or 800 mg COPEGUS.
HCV 2 and 3 – Irrespective of baseline viral titer, treatment for 24 weeks with Pegylated interferon alfa-2a and 800 mg of COPEGUS resulted in a similar SVR compared to longer treatment (48 weeks) and/or 1000 mg or 1200 mg of COPEGUS.
The numbers of subjects with genotype 5 and 6 were too few to allow meaningful assessment.
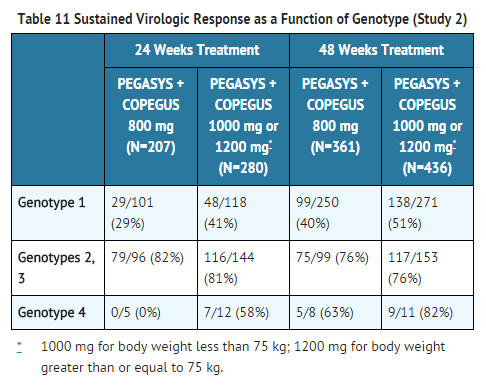
Other Treatment Response Predictors
Treatment response rates are lower in subjects with poor prognostic factors receiving pegylated interferon alpha therapy. In studies 1 and 2, treatment response rates were lower in subjects older than 40 years (50% vs. 66%), in subjects with cirrhosis (47% vs. 59%), in subjects weighing over 85 kg (49% vs. 60%), and in subjects with genotype 1 with high vs. low viral load (43% vs. 56%). African-American subjects had lower response rates compared to Caucasians.
Paired liver biopsies were performed on approximately 20% of subjects in studies 4 and 5. Modest reductions in inflammation compared to baseline were seen in all treatment groups.
In studies 1 and 2, lack of early virologic response by 12 weeks (defined as HCV RNA undetectable or greater than 2 log10 lower than baseline) was grounds for discontinuation of treatment. Of subjects who lacked an early viral response by 12 weeks and completed a recommended course of therapy despite a protocol-defined option to discontinue therapy, 5/39 (13%) achieved an SVR. Of subjects who lacked an early viral response by 24 weeks, 19 completed a full course of therapy and none achieved an SVR.
Pediatric Patients
Previously untreated pediatric subjects 5 through 17 years of age (55% less than 12 years old) with chronic hepatitis C, compensated liver disease and detectable HCV RNA were treated with COPEGUS approximately 15 mg/kg/day plus Pegylated interferon alfa-2a 180 mcg/1.73 m2 × body surface area once weekly for 48 weeks. All subjects were followed for 24 weeks post-treatment. Sustained virological response (SVR) was defined as undetectable (less than 50 IU/mL) HCV RNA on or after study week 68. A total of 114 subjects were randomized to receive either combination treatment of COPEGUS plus Pegylated interferon alfa-2a or Pegylated interferon alfa-2a monotherapy; subjects failing Pegylated interferon alfa-2a monotherapy at 24 weeks or later could receive open-label COPEGUS plus Pegylated interferon alfa-2a. The initial randomized arms were balanced for demographic factors; 55 subjects received initial combination treatment of COPEGUS plus Pegylated interferon alfa-2a and 59 received Pegylated interferon alfa-2a plus placebo; in the overall intent-to-treat population, 45% were female, 80% were Caucasian, and 81% were infected with HCV genotype 1.
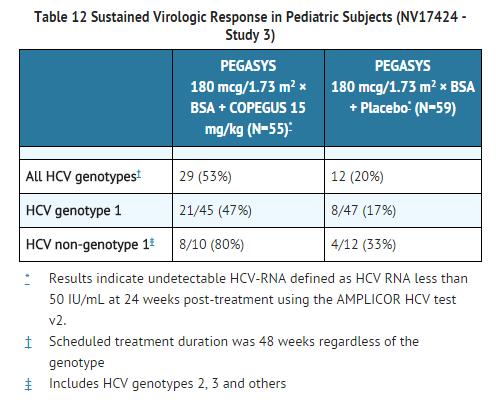
Chronic Hepatitis C and Coinfection with HIV (CHC/HIV)
Study 4: Pegylated interferon alfa-2a Monotherapy and Pegylated interferon alfa-2a/COPEGUS Combination Therapy
In Study 4, subjects with CHC/HIV were randomized to receive either Pegylated interferon alfa-2a 180 mcg subcutaneous once weekly plus an oral placebo, Pegylated interferon alfa-2a 180 mcg once weekly plus COPEGUS 800 mg by mouth daily or ROFERON-A (interferon alfa-2a), 3 MIU subcutaneous three times a week plus COPEGUS 800 mg by mouth daily. All subjects received 48 weeks of therapy and sustained virologic response (SVR) was assessed at 24 weeks of treatment-free follow-up. COPEGUS or placebo treatment assignment was blinded in the Pegylated interferon alfa-2a treatment arms. All subjects were adults, had compensated liver disease, detectable hepatitis C virus, liver biopsy diagnosis of chronic hepatitis C, and were previously untreated with interferon. Subjects also had CD4+ cell count greater than or equal to 200 cells/mm3 or CD4+ cell count greater than or equal to 100 cells/mm3 but less than 200 cells/mm3 and HIV-1 RNA less than 5,000 cells/mm3, and stable status of HIV. Approximately 15% of subjects in the study had cirrhosis.
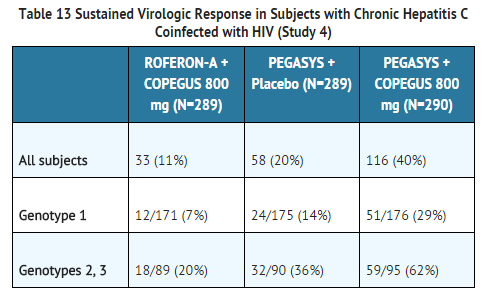
Treatment response rates are lower in CHC/HIV subjects with poor prognostic factors (including HCV genotype 1, HCV RNA greater than 800,000 IU/mL, and cirrhosis) receiving pegylated interferon alpha therapy. Geographic region is not a prognostic factor for response. However, poor prognostic factors occur more frequently in the US population than in the non-US population.
Of the subjects who did not demonstrate either undetectable HCV RNA or at least a 2 log10 reduction from baseline in HCV RNA titer by 12 weeks of Pegylated interferon alfa-2a and ribavirin combination therapy, 2% (2/85) achieved an SVR.
In CHC subjects with HIV coinfection who received 48 weeks of Pegylated interferon alfa-2a alone or in combination with ribavirin treatment, mean and median HIV RNA titers did not increase above baseline during treatment or 24 weeks post-treatment.
Chronic Hepatitis C Studies 5, 6, and 7: Pegylated interferon alfa-2a Monotherapy
The safety and effectiveness of Pegylated interferon alfa-2a for the treatment of hepatitis C virus infection were assessed in three randomized, open-label, active-controlled clinical studies. All subjects were adults, had compensated liver disease, detectable hepatitis C virus (HCV), liver biopsy diagnosis of chronic hepatitis, and were previously untreated with interferon. All subjects received therapy by subcutaneous injection for 48 weeks, and were followed for an additional 24 weeks to assess the durability of response. In studies 5 and 6, approximately 20% of subjects had cirrhosis or bridging fibrosis. Study 7 enrolled subjects with a histological diagnosis of cirrhosis (78%) or bridging fibrosis (22%).
In Study 5 (n=630), subjects received either ROFERON-A (interferon alfa-2a) 3 MIU three times a week, Pegylated interferon alfa-2a 135 mcg once weekly or Pegylated interferon alfa-2a 180 mcg once weekly. In Study 6 (n=526), subjects received either ROFERON-A 6 MIU three times a week for 12 weeks followed by 3 MIU three times a week for 36 weeks or Pegylated interferon alfa-2a 180 mcg once weekly. In Study 7 (n=269), subjects received ROFERON-A 3 MIU three times a week, Pegylated interferon alfa-2a 90 mcg once weekly or Pegylated interferon alfa-2a 180 mcg once each week.
In all three studies, treatment with Pegylated interferon alfa-2a 180 mcg resulted in significantly more subjects who experienced a sustained response (defined as undetectable HCV RNA [less than 50 IU/mL] using the COBAS AMPLICOR® HCV Test, version 2 and normalization of ALT on or after study week 68) compared to treatment with ROFERON-A.
In Study 5, response to Pegylated interferon alfa-2a 135 mcg was not different from response to 180 mcg. In Study 7, response to Pegylated interferon alfa-2a 90 mcg was intermediate between Pegylated interferon alfa-2a 180 mcg and ROFERON-A.
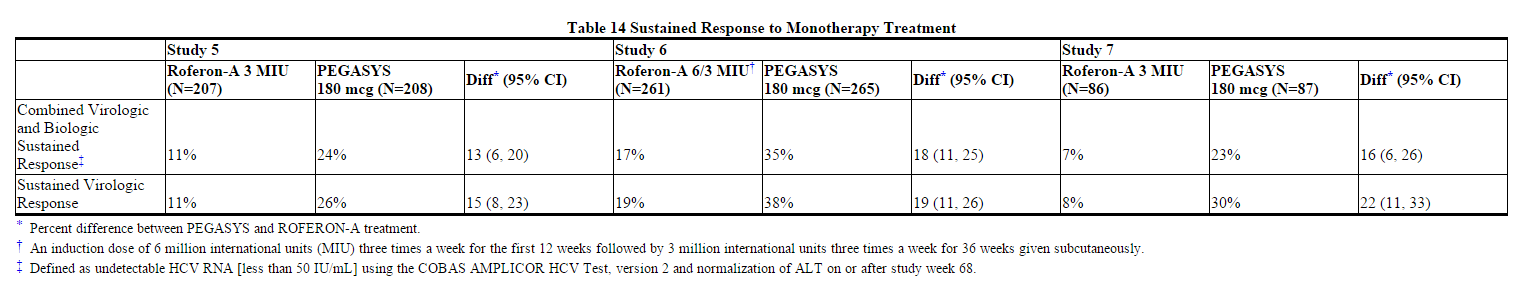
Matched pre- and post-treatment liver biopsies were obtained in approximately 70% of subjects. Similar modest reductions in inflammation compared to baseline were observed in all treatment groups.
Of the subjects who did not demonstrate either undetectable HCV RNA or at least a 2 log10 drop in HCV RNA titer from baseline by 12 weeks of Pegylated interferon alfa-2a 180 mcg therapy, 2% (3/156) achieved a sustained virologic response.
Averaged over Study 5, Study 6, and Study 7, response rates to Pegylated interferon alfa-2a were 23% among subjects with viral genotype 1 and 48% among subjects with other viral genotypes. The treatment response rates were similar in men and women.
Chronic Hepatitis B Studies 8 and 9: Pegylated interferon alfa-2a Monotherapy
The safety and effectiveness of Pegylated interferon alfa-2a for the treatment of chronic hepatitis B were assessed in controlled clinical trials in HBeAg positive (Study 8) and HBeAg negative (Study 9) subjects with chronic hepatitis B.
Subjects were randomized to Pegylated interferon alfa-2a 180 mcg subcutaneous once weekly, Pegylated interferon alfa-2a 180 mcg subcutaneous once weekly combined with lamivudine 100 mg once daily by mouth or lamivudine 100 mg once daily by mouth. All subjects received 48 weeks of their assigned therapy followed by 24 weeks of treatment-free follow-up. Assignment to receipt of Pegylated interferon alfa-2a or no Pegylated interferon alfa-2a was not masked.
All subjects were adults with compensated liver disease, had chronic hepatitis B virus (HBV) infection, and evidence of HBV replication (serum HBV greater than 500,000 copies/mL for Study 8 and greater than 100,000 copies/mL for Study 8) as measured by PCR (COBAS AMPLICOR® HBV Assay). All subjects had serum alanine aminotransferase (ALT) between 1 and 10 times the upper limit of normal (ULN) and liver biopsy findings compatible with the diagnosis of chronic hepatitis.
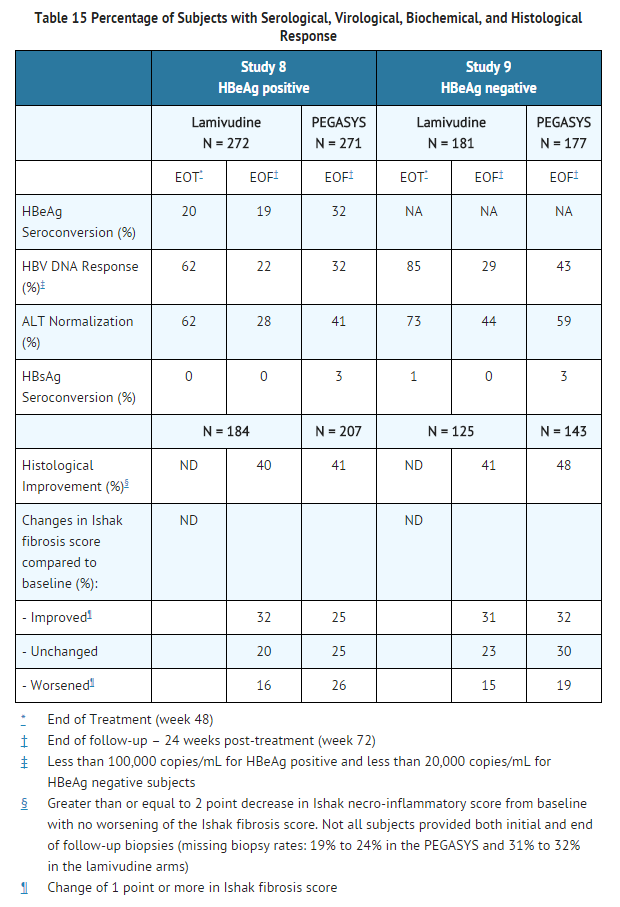
Pegylated interferon alfa-2a co-administered with lamivudine did not result in any additional sustained response when compared to Pegylated interferon alfa-2a monotherapy.
Conclusions regarding comparative efficacy of Pegylated interferon alfa-2a and lamivudine treatment based upon the end of follow-up results are limited by the different mechanisms of action of the two compounds. Most treatment effects of lamivudine are unlikely to persist 24 weeks after therapy is withdrawn.
How Supplied
- Pegylated interferon alfa-2a injection 180 mcg/mL in a vial
- Pegylated interferon alfa-2a injection 180 mcg/0.5 mL in a prefilled syringe
- Pegylated interferon alfa-2a injection 180 mcg/0.5 mL in an autoinjector
- Pegylated interferon alfa-2a injection 135 mcg/0.5 mL in an autoinjector
Storage
Store in the refrigerator at 2°C to 8°C (36°F to 46°F).
Images
Drug Images
{{#ask: Page Name::Pegylated interferon alfa-2a |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
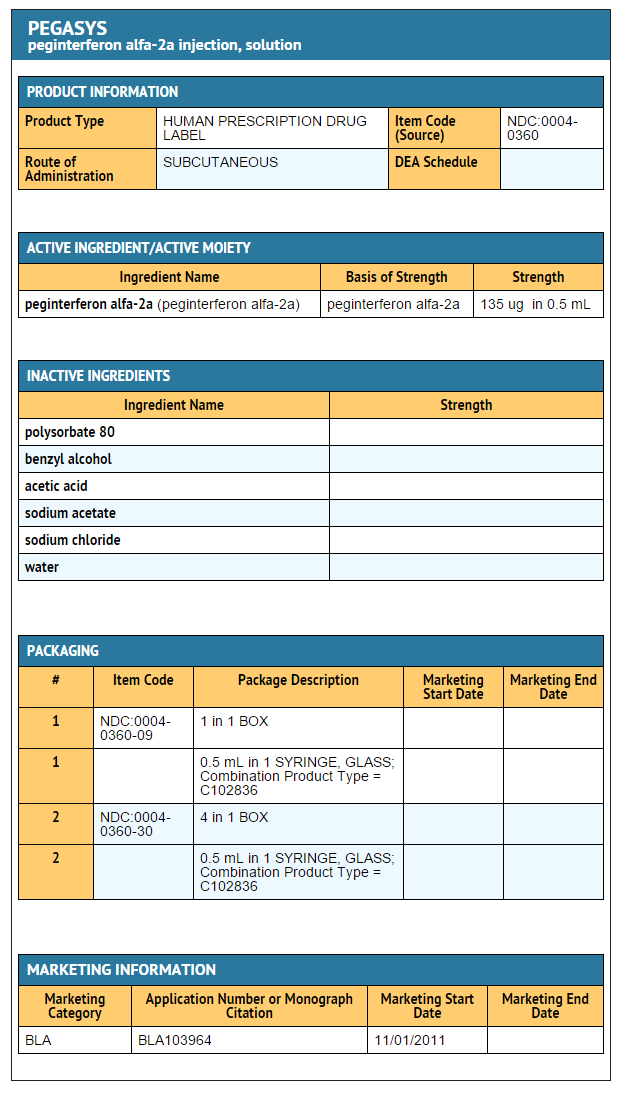
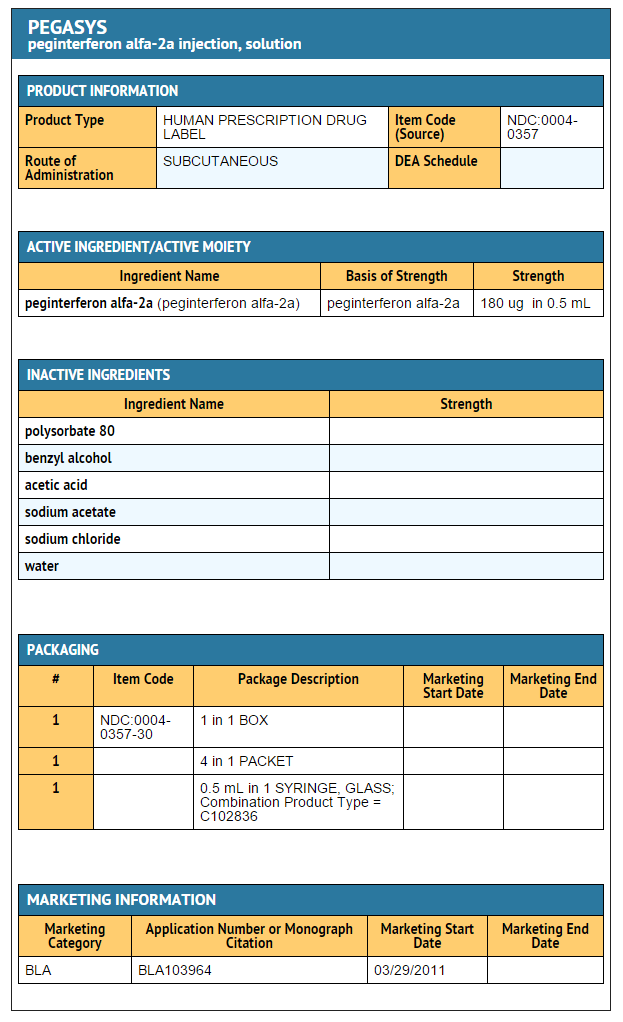
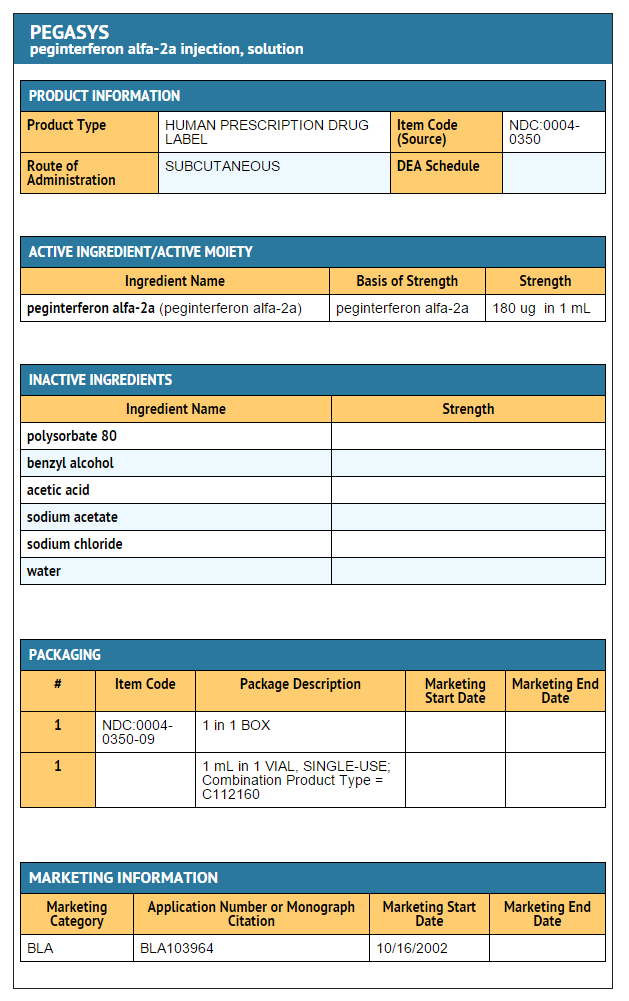
{{#ask: Label Page::Pegylated interferon alfa-2a |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patients receiving Pegylated interferon alfa-2a alone or in combination with an approved HCV antiviral drug should be directed in its appropriate use, informed of the benefits and risks associated with treatment, and referred FDA- approved patient labeling.
Pregnancy
Patients must be informed that ribavirin must not be used by women who are pregnant or by men whose female partners are pregnant. Ribavirin therapy should not be initiated until a report of a negative pregnancy test has been obtained immediately before starting therapy. Female patients of childbearing potential and male patients with female partners of childbearing potential must be advised of the teratogenic/embryocidal risks and must be instructed to practice effective contraception during ribavirin therapy and for 6 months post-therapy. Patients should be advised to notify the healthcare provider immediately in the event of a pregnancy.
Women of childbearing potential and men must use two forms of effective contraception during treatment and during the 6 months after treatment has been stopped; routine monthly pregnancy tests must be performed during this time.
Laboratory Evaluations and Hydration
Patients should be advised that laboratory evaluations are required before starting therapy and periodically thereafter. Patients should be instructed to remain well hydrated, especially during the initial stages of treatment.
General Information
Patients should be questioned about prior history of drug abuse before initiating Pegylated interferon alfa-2a; as relapse of drug addiction and drug overdoses have been reported in patients treated with interferons.
Patients should be informed that it is not known if therapy with Pegylated interferon alfa-2a will prevent transmission of HBV infection to others or prevent cirrhosis, liver failure or liver cancer that might result from HBV infection.
Patients should be informed that the effect of treatment of hepatitis C infection on transmission is not known, and that appropriate precautions to prevent transmission of the hepatitis C virus during treatment or in the event of treatment failure should be taken.
Patients who develop dizziness, confusion, somnolence, and fatigue should be cautioned to avoid driving or operating machinery.
Patients should be advised to avoid drinking alcohol to reduce the chance of further injury to the liver.
Patients should not switch to another brand of interferon without consulting their healthcare provider.
Dosing Instructions
Patients should be advised to take their prescribed dose of Pegylated interferon alfa-2a on the same day and approximately same time each week. Patients should also be advised that if they miss a dose, but remember within 2 days, to take their missed dose as soon as they remember and then to take their next dose on the day they normally do. If they remember when more than 2 days have passed, patients should be advised to consult their healthcare provider. Patients should also be advised to consult their healthcare provider if the full dose is not received (e.g., leakage around the injection site).
Patients must be instructed on the use of aseptic techniques when administering Pegylated interferon alfa-2a.
Patients should be instructed to allow the vial, prefilled syringe or autoinjector to come to room temperature and for condensation on the outside of the prefilled syringe or autoinjector to disappear before use. The following instructions should be given:
- Vial: warm the refrigerated medicine by gently rolling in the palms of the hands for about one minute.
- Pre-filled syringe: lay the syringe on a flat clean surface and wait a few minutes until it reaches room temperature. If condensation water is observed on the outside of the syringe, wait another few minutes until it disappears.
- Disposable autoinjector: place the autoinjector on a clean flat surface. Do not remove the cap at this time. Allow the autoinjector to come to room temperature for about 20 minutes to warm up. Do not warm up the autoinjector in any other way.
Patients should be advised not to shake the vial, prefilled syringe or autoinjector as foaming may occur.
Patients should be advised to choose a different place on either the thigh or abdomen each time an injection is made.
Precautions with Alcohol
Alcohol-Pegylated interferon alfa-2a interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Pegasys [2]
- Pegasys Proclick
Look-Alike Drug Names
There is limited information regarding Pegylated interferon alfa-2a Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
{{#subobject:
|Label Page=Pegylated interferon alfa-2a |Label Name=Peginterferon alfa-2a 135 ug-0.5 ml.png
}}
{{#subobject:
|Label Page=Pegylated interferon alfa-2a |Label Name=Peginterferon alfa-2a 180 ug-0.5 ml.png
}}
{{#subobject:
|Label Page=Pegylated interferon alfa-2a |Label Name=Peginterferon alfa-2a 180 ug-1 ml.png
}}