Patent ductus arteriosus pathophysiology
|
Patent Ductus Arteriosus Microchapters |
|
Differentiating Patent Ductus Arteriosus from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Patent ductus arteriosus pathophysiology On the Web |
|
American Roentgen Ray Society Images of Patent ductus arteriosus pathophysiology |
|
Risk calculators and risk factors for Patent ductus arteriosus pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Priyamvada Singh, M.B.B.S. [2], Cafer Zorkun, M.D., Ph.D. [3], Assistant Editor-In-Chief: Kristin Feeney, B.S. [4]
Overview
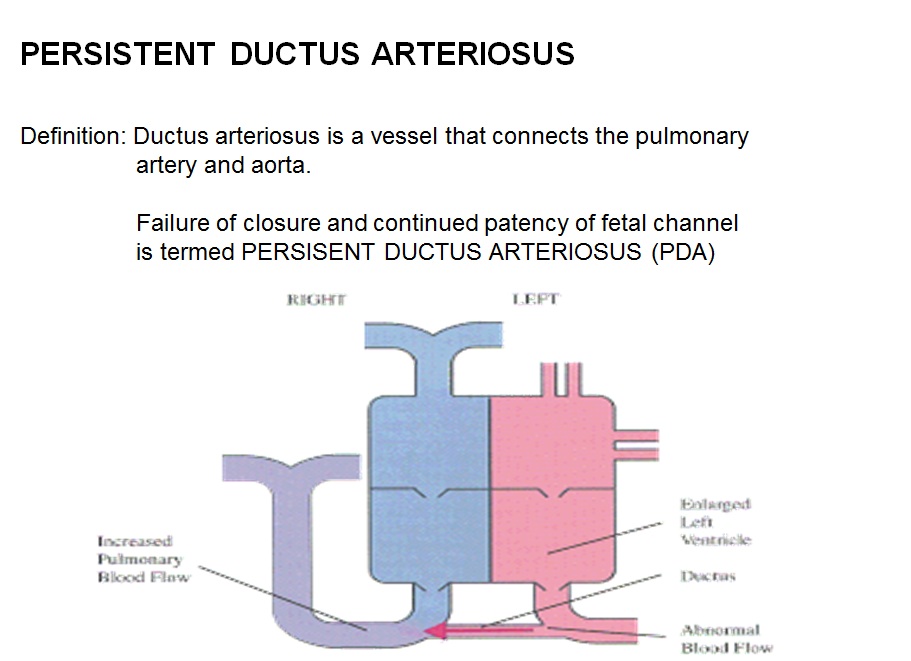
The pathophysiological consequences depend on the size of the defect and the pulmonary vascular resistance.[1]
Pathophysiology
Small-Sized PDA
- Small left-to-right shunt (Qp/Qs < 1.5)
- Normal ratio of pulmonary artery (PA) to systemic pressure.
- Shunt throughout the cardiac cycle, continuous murmur.
Medium-Sized PDA
- Qp/Qs 1.5 to 2.0 yet small enough to offer some resistance to flow.
- PA systolic to systemic pressures are < 0.5
- Unusual for this group to have markedly increased PVR.
- Due to increased return to the left heart, there is volume overload of the left atrium (LA) and the left ventricle (LV).
Large PDA
- Defect does not restrict flow.
- There is pulmonary hypertension at near systemic pressures (PA systolic/systolic pressure is >0.5).
- Because of the physiologic decrease in the PVR over the first three months of life there is a large left-to-right shunt with Qp/Qs > 2.
- The large volume overload of the left ventricle may result in LV failure.
- There is pulmonary hypertension.
- There may be two courses:
- A decrease in the relative size of the ductus compared with other cardiovascular structures. This results in a medium-sized defect compared with the course expected for a medium-sized defect.
- The development of severe pulmonary vascular obstructive disease, can occur at any time from age 3 until early adulthood. The left-to-right shunt converts to a right-to-left shunt with cyanosis and disappearance of the continuous murmur.
Gross Pathology
-
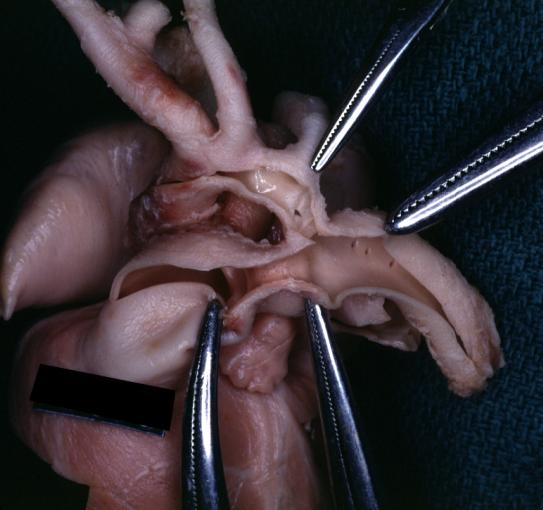
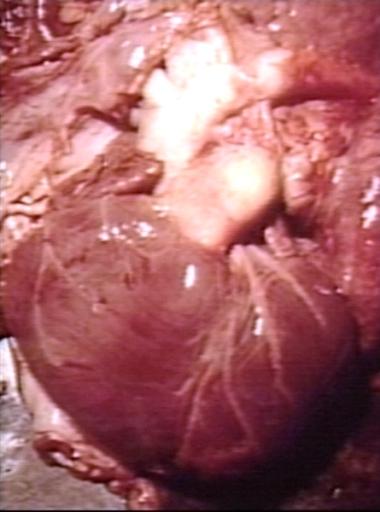
Patent Ductus Arteriosus: Gross example in an infant heart
-
Patent Ductus Arteriosus: Gross fixed tissue probe in ductus
-
Patent Ductus Arteriosus: Gross fixed tissue view of ductus opened from pulmonary artery into aorta with edematous appearing intimal surface
-
Patent Ductus Arteriosus: Gross natural color opened ductus in infant shows apparent intimal edema in ductus.
-
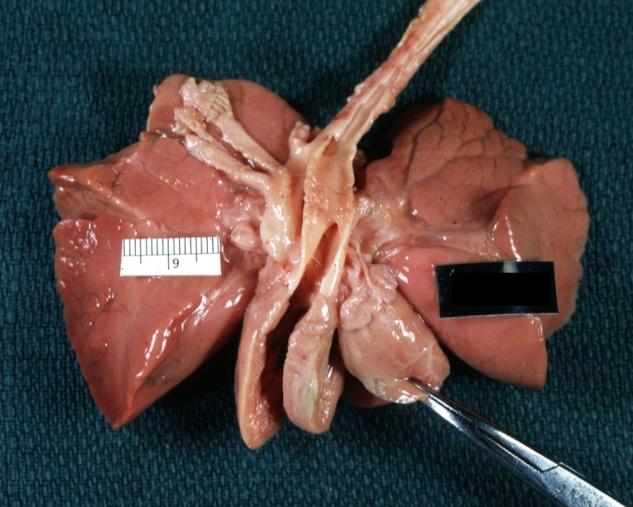
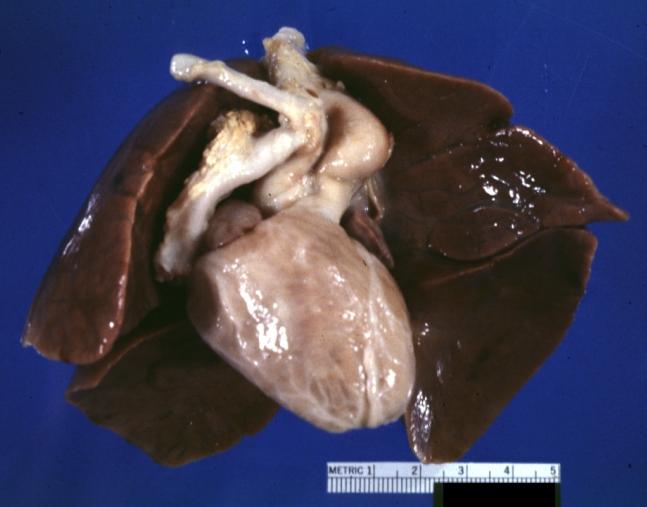
Patent Ductus Arteriosus with Aneurysmal Dilation: Gross fixed tissue external photo of heart shows the lesion
-
Patent Ductus Arteriosus with Aneurysmal Dilation: Gross fixed tissue aorta and ductus have been cross sectioned showing arch of aorta and huge ductus in a 5 day old infant
-
Patent Ductus Arteriosus with Aneurysmal Dilation: Gross fixed tissue opened aortic arch and descending thoracic showing very large opening of ductus into aorta
-
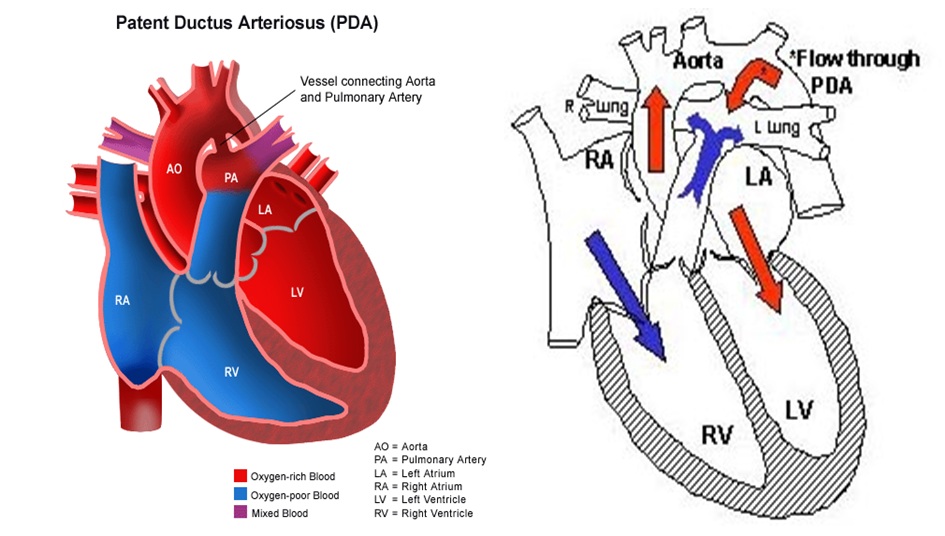
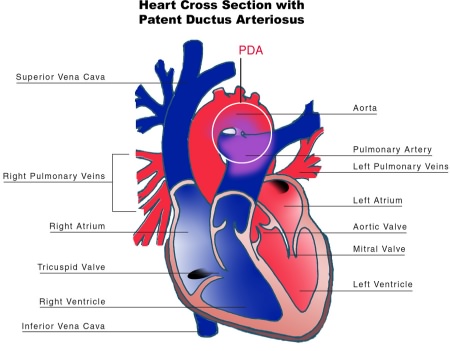
Patent Ductus Arteriosus
Shown below is the pictoral image of pathophysiology of patent ductus arteriosus
Shown below is the image of pathophysiology of patent ductus arteriosus in the cross-section of the heart
Videos
{{#ev:youtube|5_BNHYGUgG4}}
Diagram
Diagram of heart showing a patent ductus arteriosus
References
- ↑ Giuliani et al, Cardiology: Fundamentals and Practice, Second Edition, Mosby Year Book, Boston, 1991, pp. 1653-1663.