Patent ductus arteriosus pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 5: | Line 5: | ||
==Pathophysiology== | ==Pathophysiology== | ||
The pathophysiological consequences depend on the size of the defect and the pulmonary vascular resistance. <ref>Giuliani et al, Cardiology: Fundamentals and Practice, Second Edition, Mosby Year Book, Boston, 1991, pp. 1653-1663.</ref> | The pathophysiological consequences depend on the size of the defect and the pulmonary vascular resistance. <ref>Giuliani et al, Cardiology: Fundamentals and Practice, Second Edition, Mosby Year Book, Boston, 1991, pp. 1653-1663.</ref> | ||
==Small PDA== | ==Small PDA== | ||
#Small [[left-to-right shunt]] (Qp/Qs < 1.5). | #Small [[left-to-right shunt]] (Qp/Qs < 1.5). | ||
#Normal ratio of [[pulmonary artery]] (PA) to systemic pressure. | #Normal ratio of [[pulmonary artery]] (PA) to systemic pressure. | ||
#Shunt throughout the cardiac cycle, [[continuous murmur]]. | #Shunt throughout the cardiac cycle, [[continuous murmur]]. | ||
==Medium-sized PDA== | ==Medium-sized PDA== | ||
#Qp/Qs 1.5 to 2.0 yet small enough to offer some resistance to flow. | #Qp/Qs 1.5 to 2.0 yet small enough to offer some resistance to flow. | ||
| Line 16: | Line 14: | ||
#Unusual for this group to have markedly increased [[PVR]]. | #Unusual for this group to have markedly increased [[PVR]]. | ||
#Due to increased return to the left heart, there is volume overload of the [[left atrium]] ([[LA]]) and the [[left ventricle]] ([[LV]]). | #Due to increased return to the left heart, there is volume overload of the [[left atrium]] ([[LA]]) and the [[left ventricle]] ([[LV]]). | ||
==Large PDA== | |||
==Large PDA== | |||
#Defect does not restrict flow. | #Defect does not restrict flow. | ||
#There is [[pulmonary hypertension]] at near systemic pressures ([[PA]] systolic/systolic pressure is >0.5). | #There is [[pulmonary hypertension]] at near systemic pressures ([[PA]] systolic/systolic pressure is >0.5). | ||
Revision as of 01:41, 16 August 2011
|
Patent Ductus Arteriosus Microchapters |
|
Differentiating Patent Ductus Arteriosus from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Medical Therapy |
|
Case Studies |
|
Patent ductus arteriosus pathophysiology On the Web |
|
American Roentgen Ray Society Images of Patent ductus arteriosus pathophysiology |
|
Risk calculators and risk factors for Patent ductus arteriosus pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Priyamvada Singh, M.B.B.S. [2], Cafer Zorkun, M.D., Ph.D. [3], Assistant Editor-In-Chief: Kristin Feeney, B.S. [4]
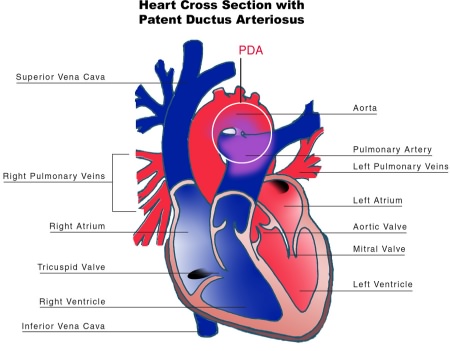
Overview
The pathophysiological findings depend on the size of defect and the pulmonary vascular resistance
Pathophysiology
The pathophysiological consequences depend on the size of the defect and the pulmonary vascular resistance. [1]
Small PDA
- Small left-to-right shunt (Qp/Qs < 1.5).
- Normal ratio of pulmonary artery (PA) to systemic pressure.
- Shunt throughout the cardiac cycle, continuous murmur.
Medium-sized PDA
- Qp/Qs 1.5 to 2.0 yet small enough to offer some resistance to flow.
- PA systolic to systemic pressures are < 0.5.
- Unusual for this group to have markedly increased PVR.
- Due to increased return to the left heart, there is volume overload of the left atrium (LA) and the left ventricle (LV).
==Large PDA==
- Defect does not restrict flow.
- There is pulmonary hypertension at near systemic pressures (PA systolic/systolic pressure is >0.5).
- Because of the physiologic decrease in the PVR over the first three months of life there is a large left-to-right shunt with Qp/Qs > 2.
- The large volume overload of the left ventricle may result in LV failure.
- There is pulmonary hypertension.
- There may be two courses:
- A decrease in the relative size of the ductus compared with other cardiovascular structures. This results in a medium-sized defect compared with the course expected for a medium-sized defect.
- The development of severe pulmonary vascular obstructive disease, can occur at any time from age 3 until early adulthood. The left-to-right shunt converts to a right-to-left shunt with cyanosis and disappearance of the continuous murmur.
Pathological Findings
References
- ↑ Giuliani et al, Cardiology: Fundamentals and Practice, Second Edition, Mosby Year Book, Boston, 1991, pp. 1653-1663.