Paroxysmal AV block Implantable Loop Recorder: Difference between revisions
Jump to navigation
Jump to search
(Created page with "==Implantable Loop Recorder== *Implantable loop recorders are useful tools as they help correlate electrical tracings with the patients symptoms during an acute event. **By gi...") |
|||
| Line 15: | Line 15: | ||
*'''The ISSUE 2 study''' (characterized by a frequently injured elderly population with a history of recurrent syncope) demonstrated the importance of implantable loop recorders (ILR) as a diagnostic modality by showing that '''the recurrence rate in syncope patients treated with ILR based therapy was much lower than those treated with no-specific therapy'''. | *'''The ISSUE 2 study''' (characterized by a frequently injured elderly population with a history of recurrent syncope) demonstrated the importance of implantable loop recorders (ILR) as a diagnostic modality by showing that '''the recurrence rate in syncope patients treated with ILR based therapy was much lower than those treated with no-specific therapy'''. | ||
**In addition, a recurrence rate of 5% was noted in those treated with cardiac pacing.<ref name="pmid16569653">{{cite journal| author=Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W | display-authors=etal| title=Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope. | journal=Eur Heart J | year= 2006 | volume= 27 | issue= 9 | pages= 1085-92 | pmid=16569653 | doi=10.1093/eurheartj/ehi842 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16569653 }} </ref> | **In addition, a recurrence rate of 5% was noted in those treated with cardiac pacing.<ref name="pmid16569653">{{cite journal| author=Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W | display-authors=etal| title=Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope. | journal=Eur Heart J | year= 2006 | volume= 27 | issue= 9 | pages= 1085-92 | pmid=16569653 | doi=10.1093/eurheartj/ehi842 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16569653 }} </ref> | ||
=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay:Recommendation for Implantable Cardiac Monitor= | |||
{|class="wikitable" | |||
|- | |||
| colspan="1" style="text-align:center; background: Pink"|[[2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay| Recommendation for Implantable Cardiac Monitor]] | |||
|- | |||
| bgcolor="Pink"|<nowiki>"</nowiki>'''1.''' In patients with infrequent symptoms (>30 days between symptoms) suspected to be caused by bradycardia, longterm ambulatory monitoring with an implantable cardiac monitor (ICM) is reasonable if initial noninvasive evaluation is nondiagnostic.''([[ACC AHA Guidelines Classification Scheme#Level of Evidence|Level of Evidence: C-LD]])<ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref>'' <nowiki>"</nowiki> | |||
|} | |||
*One of the most debilitating symptoms of bradycardia is syncope resulting in trauma. | |||
The suddenness and unpredictability of such events make the Implantable Cardiac Monitor (ICM) an ideal diagnostic tool given its capacity for prolonged monitoring (up to 3 years) and its freedom of reliance on active patient participation. | |||
*Early work as well as subsequent randomized and nonrandomized studies evaluating the diagnostic efficacy of ICM were almost exclusively performed in patients presenting with unexplained syncope and/or presyncope and not specifically for identification of bradycardia. | |||
*In patients with ongoing or frequent symptoms of bradycardia, the 12- lead ECG or external ambulatory electrocardiographic monitoring can usually document sinus node dysfunction (SND) or atrioventricular conduction disease. | |||
*However, when patients present with infrequent paroxysmal or infrequent symptoms, culprit bradycardias can evade the detection by standard external monitoring modalities. Longer duration of ambulatory monitoring with ICM may then be necessary to obtain correlation between bradycardia and symptoms. | |||
*Compared with investigation by conventional testing modalities such as 24-hour ambulatory electrocardiographic monitoring, 12-lead ECG, and treadmill stress test, the strategy of long-term rhythm monitoring with ICM was more effective in obtaining a clinical diagnosis. | |||
*Many of the conditions diagnosed by ICM were found to be bradycardia-mediated (ie, high-grade atrioventricular block, SND, neurocardiogenic syncope with predominant cardio-inhibitory component) and were successfully treated with permanent cardiac pacing. | |||
*External monitors will generally be the first-line choice of diagnostic tools in an effort to obtain potential correlation between bradycardia and symptoms but, for patients with very infrequent symptoms, initial ICM implantation may be the best and most cost-effective initial strategy. <ref name="pmid30412710">{{cite journal| author=Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR | display-authors=etal| title=2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society. | journal=J Am Coll Cardiol | year= 2019 | volume= 74 | issue= 7 | pages= 932-987 | pmid=30412710 | doi=10.1016/j.jacc.2018.10.043 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30412710 }} </ref> | |||
Revision as of 21:22, 25 June 2020
Implantable Loop Recorder
- Implantable loop recorders are useful tools as they help correlate electrical tracings with the patients symptoms during an acute event.
- By giving an inkling of the etiology of the syncope, it helps guide therapy strategies, such as adopting permanent stimulation devices in patients with paroxysmal AV block.[1]
- According to the European Society of Cardiology, the indication for implantable loop recorders are as follows :
- In the early phase of evaluation in patients with recurrent syncope of uncertain origin, absence of high risk criteria and a high likelihood od recurrence within the battery life of the device/
- In patients with suspected or certain reflex syncope presenting with frequent or severe syncopal episodes
- In patients whom epilepsy was suspected but the treatment has proven ineffective.
- In patients with unexplained falls. "ESC Guidelines on Syncope (Diagnosis and Management of)".
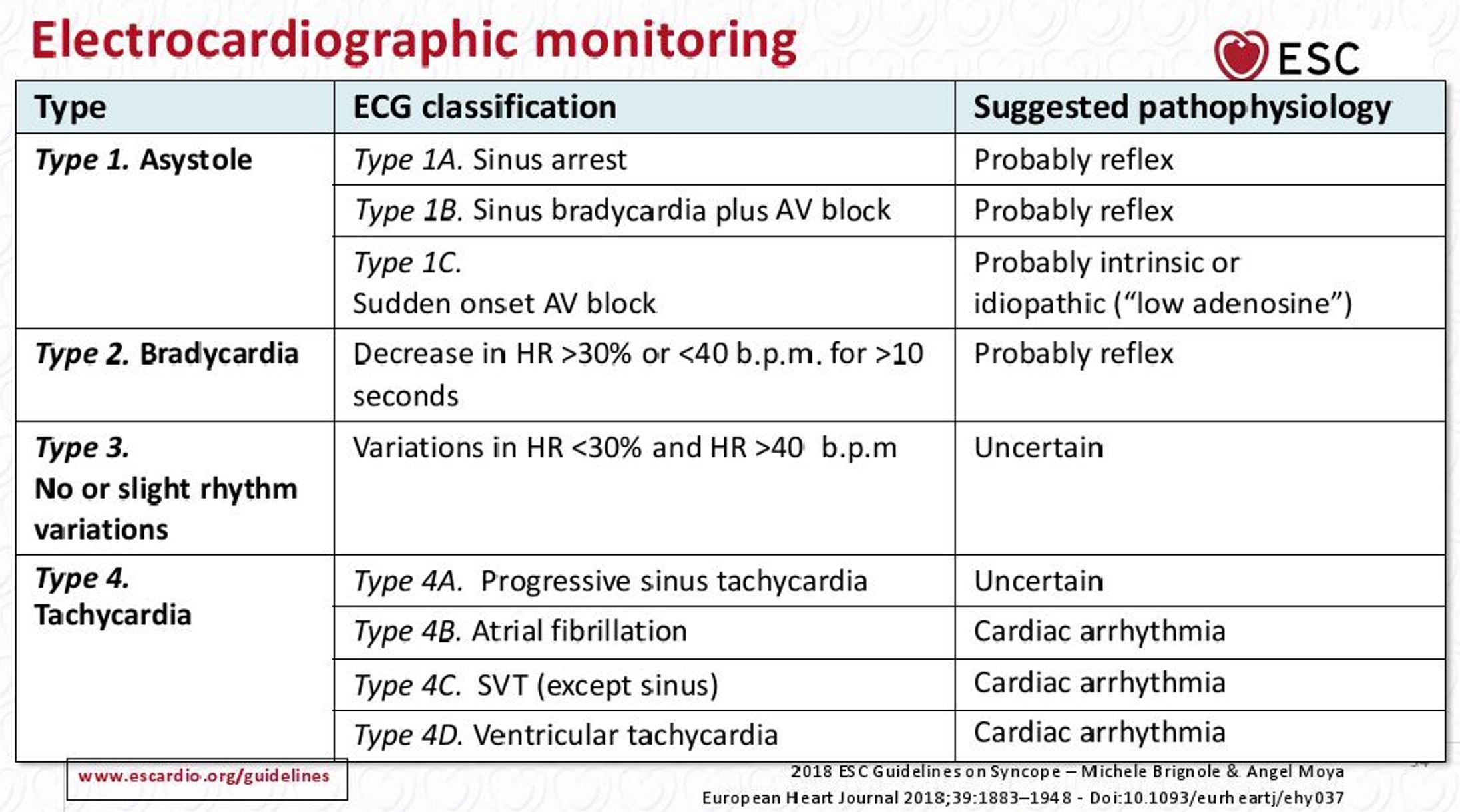
- The ISSUE (International Study on Syncope of Unknown Etiology) study conducted by Brignole et al monitored 198 patients with an implantable loop recorder and classified the first syncope event following implantation.
- The ISSUE classification has pathophysiological implications in terms of the event being neutrally mediated (type 1A or type 1B or type 2), due to an intrinsic conduction defect (type 1C), secondary to orthostatic hypotension (type 4A) or a primary cardiac arrhythmia (types 4B, 4C or 4D).[2]
- The ISSUE 2 study (characterized by a frequently injured elderly population with a history of recurrent syncope) demonstrated the importance of implantable loop recorders (ILR) as a diagnostic modality by showing that the recurrence rate in syncope patients treated with ILR based therapy was much lower than those treated with no-specific therapy.
- In addition, a recurrence rate of 5% was noted in those treated with cardiac pacing.[3]
2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay:Recommendation for Implantable Cardiac Monitor
| Recommendation for Implantable Cardiac Monitor |
| "1. In patients with infrequent symptoms (>30 days between symptoms) suspected to be caused by bradycardia, longterm ambulatory monitoring with an implantable cardiac monitor (ICM) is reasonable if initial noninvasive evaluation is nondiagnostic.(Level of Evidence: C-LD)[4] " |
- One of the most debilitating symptoms of bradycardia is syncope resulting in trauma.
The suddenness and unpredictability of such events make the Implantable Cardiac Monitor (ICM) an ideal diagnostic tool given its capacity for prolonged monitoring (up to 3 years) and its freedom of reliance on active patient participation.
- Early work as well as subsequent randomized and nonrandomized studies evaluating the diagnostic efficacy of ICM were almost exclusively performed in patients presenting with unexplained syncope and/or presyncope and not specifically for identification of bradycardia.
- In patients with ongoing or frequent symptoms of bradycardia, the 12- lead ECG or external ambulatory electrocardiographic monitoring can usually document sinus node dysfunction (SND) or atrioventricular conduction disease.
- However, when patients present with infrequent paroxysmal or infrequent symptoms, culprit bradycardias can evade the detection by standard external monitoring modalities. Longer duration of ambulatory monitoring with ICM may then be necessary to obtain correlation between bradycardia and symptoms.
- Compared with investigation by conventional testing modalities such as 24-hour ambulatory electrocardiographic monitoring, 12-lead ECG, and treadmill stress test, the strategy of long-term rhythm monitoring with ICM was more effective in obtaining a clinical diagnosis.
- Many of the conditions diagnosed by ICM were found to be bradycardia-mediated (ie, high-grade atrioventricular block, SND, neurocardiogenic syncope with predominant cardio-inhibitory component) and were successfully treated with permanent cardiac pacing.
- External monitors will generally be the first-line choice of diagnostic tools in an effort to obtain potential correlation between bradycardia and symptoms but, for patients with very infrequent symptoms, initial ICM implantation may be the best and most cost-effective initial strategy. [4]
- ↑ Guerrero-Márquez FJ, Arana-Rueda E, Pedrote A (2016). "Idiopathic Paroxysmal Atrio-Ventricular Block. What is The Mechanism?". J Atr Fibrillation. 9 (3): 1449. doi:10.4022/jafib.1449. PMC 5368548. PMID 28496928.
- ↑ Brignole M, Moya A, Menozzi C, Garcia-Civera R, Sutton R (2005). "Proposed electrocardiographic classification of spontaneous syncope documented by an implantable loop recorder". Europace. 7 (1): 14–8. doi:10.1016/j.eupc.2004.11.001. PMID 15670961.
- ↑ Brignole M, Sutton R, Menozzi C, Garcia-Civera R, Moya A, Wieling W; et al. (2006). "Early application of an implantable loop recorder allows effective specific therapy in patients with recurrent suspected neurally mediated syncope". Eur Heart J. 27 (9): 1085–92. doi:10.1093/eurheartj/ehi842. PMID 16569653.
- ↑ 4.0 4.1 Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR; et al. (2019). "2018 ACC/AHA/HRS Guideline on the Evaluation and Management of Patients With Bradycardia and Cardiac Conduction Delay: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines, and the Heart Rhythm Society". J Am Coll Cardiol. 74 (7): 932–987. doi:10.1016/j.jacc.2018.10.043. PMID 30412710.