Parkes Weber syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 13: | Line 13: | ||
This syndrome was described by the same F. Parkes Weber (1863-1962) whose name is also attached to hereditary hemorrhagic telangiectasia, Sturge-Weber syndrome, Weber-Christian disease, and Klippel-Trenaunay-Weber syndrome. | This syndrome was described by the same F. Parkes Weber (1863-1962) whose name is also attached to hereditary hemorrhagic telangiectasia, Sturge-Weber syndrome, Weber-Christian disease, and Klippel-Trenaunay-Weber syndrome. | ||
== | <br /> | ||
==Historical Perspective== | |||
*[Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event]. | *[Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event]. | ||
*In [year], [gene] mutations were first identified in the pathogenesis of [disease name]. | *In [year], [gene] mutations were first identified in the pathogenesis of [disease name]. | ||
| Line 61: | Line 21: | ||
==Classification== | ==Classification== | ||
*[Disease name] may be classified according to [classification method] into [number] subtypes/groups: | *[Disease name] may be classified according to [classification method] into [number] subtypes/groups: | ||
:*[group1] | :*[group1] | ||
:*[group2] | :*[group2] | ||
:*[group3] | :*[group3] | ||
*Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3]. | *Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
Gene map locus is 5q13.3. | |||
Six families reported by Eerola et al. in 2003, manifested atypical capillary malformations associated with either arteriovenous malformation, arteriovenous fistula, or Parkes Weber syndrome. They named this association CM-AVM for 'capillary malformation-arteriovenous malformation' and found mutation in the RASA1 gene in affected members of these families. | |||
*The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3]. | *The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3]. | ||
*The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway. | *The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway. | ||
| Line 114: | Line 81: | ||
== Diagnosis == | == Diagnosis == | ||
<br /> | |||
===Clinical Presentation=== | |||
* Enlarged arteries and veins | |||
* Capillary or venous malformations | |||
* Cutaneous blush | |||
* Arteriovenous fistulas | |||
* Enlargement of a limb | |||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
*The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: | *The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met: | ||
| Line 179: | Line 155: | ||
*Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | *Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3]. | ||
===Multi Sliced CT=== | |||
<div align="center"> | |||
<gallery heights="175" widths="225"> | |||
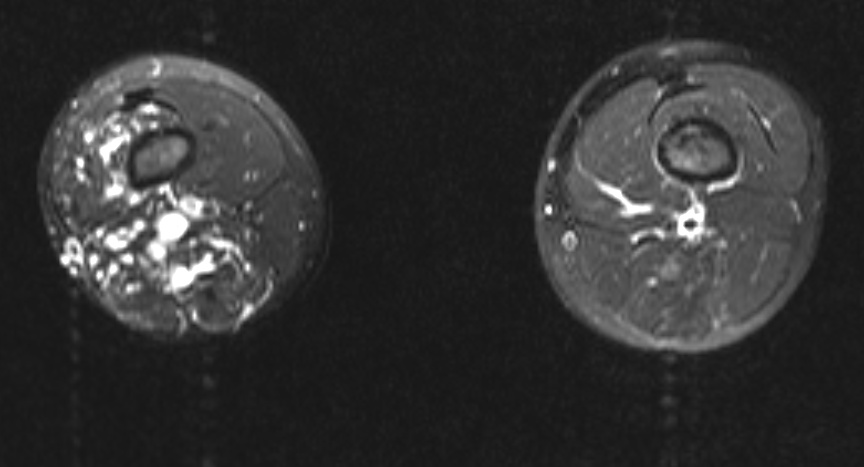
Image:Parkes_weber_t2_fs_ax.jpg|Multi Sliced CT - Lower extremities: A 10 year old boy presented for assessment of leg length discrepancy and cutaneous “capillary” vascular malformation. The provisional diagnosis was Klippel-Trenaunay syndrome. The axial fat-saturated T2 weighted MRI above shows dilated vascular structures in the right lower limb involving subcutaneous and multiple muscle compartments. Flow voids and pulsation artefact (particularly laterally) suggest a high flow component consistent with arteriovenous malformation. These findings favour Parkes Weber syndrome over Klippel-Trenaunay syndrome. There was no high output cardiac failure in this case. (Image courtesy of Dr Laughlin Dawes) | |||
</gallery> | |||
</div> | |||
==See Also== | |||
*[[Klippel-Trenaunay-Weber syndrome]] | |||
==References== | |||
{{Reflist}} | |||
* | |||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
Revision as of 19:25, 4 February 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Parkes Weber Syndrome also known as (PKWS) is a vascular abnormality and characterized by a cutaneous flush with underlying multiple micro-AVFs (arteriovenous fistulas), in association with soft tissue and skeletal hypertrophy of the affected limb. [1] [2]
This syndrome was described by the same F. Parkes Weber (1863-1962) whose name is also attached to hereditary hemorrhagic telangiectasia, Sturge-Weber syndrome, Weber-Christian disease, and Klippel-Trenaunay-Weber syndrome.
Historical Perspective
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification
- [Disease name] may be classified according to [classification method] into [number] subtypes/groups:
- [group1]
- [group2]
- [group3]
- Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3].
Pathophysiology
Gene map locus is 5q13.3.
Six families reported by Eerola et al. in 2003, manifested atypical capillary malformations associated with either arteriovenous malformation, arteriovenous fistula, or Parkes Weber syndrome. They named this association CM-AVM for 'capillary malformation-arteriovenous malformation' and found mutation in the RASA1 gene in affected members of these families.
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Clinical Features
Differentiating [disease name] from other Diseases
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location].
Age
- Patients of all age groups may develop [disease name].
- [Disease name] is more commonly observed among patients aged [age range] years old.
- [Disease name] is more commonly observed among [elderly patients/young patients/children].
Gender
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected with [disease name] than [gender 2].
- The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1.
Race
- There is no racial predilection for [disease name].
- [Disease name] usually affects individuals of the [race 1] race.
- [Race 2] individuals are less likely to develop [disease name].
Risk Factors
- Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
Natural History, Complications and Prognosis
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis
Clinical Presentation
- Enlarged arteries and veins
- Capillary or venous malformations
- Cutaneous blush
- Arteriovenous fistulas
- Enlargement of a limb
Diagnostic Criteria
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met:
- [criterion 1]
- [criterion 2]
- [criterion 3]
- [criterion 4]
Symptoms
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings
- There are no [imaging study] findings associated with [disease name].
- [Imaging study 1] is the imaging modality of choice for [disease name].
- On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3].
- [Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment
Medical Therapy
- There is no treatment for [disease name]; the mainstay of therapy is supportive care.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
Multi Sliced CT
-
Multi Sliced CT - Lower extremities: A 10 year old boy presented for assessment of leg length discrepancy and cutaneous “capillary” vascular malformation. The provisional diagnosis was Klippel-Trenaunay syndrome. The axial fat-saturated T2 weighted MRI above shows dilated vascular structures in the right lower limb involving subcutaneous and multiple muscle compartments. Flow voids and pulsation artefact (particularly laterally) suggest a high flow component consistent with arteriovenous malformation. These findings favour Parkes Weber syndrome over Klippel-Trenaunay syndrome. There was no high output cardiac failure in this case. (Image courtesy of Dr Laughlin Dawes)
See Also
References
- ↑ Eerola, I.; Boon, L. M.; Mulliken, J. B.; Burrows, P. E.; Dompmartin, A.; Watanabe, S.; Vanwijck, R.; Vikkula, M. Capillary malformation-arteriovenous malformation, a new clinical and genetic disorder caused by RASA1 mutations. Am. J. Hum. Genet. 73: 1240-1249, 2003. PMID 14639529
- ↑ Mulliken, J. B.; Young, A. E. (eds.): Vascular Birthmarks: Hemangiomas and Vascular Malformations. Philadelphia: W. B. Saunders Co., 1988