Palpitation electrocardiogram: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 3: | Line 3: | ||
{{CMG}}; {{AE}}{{Akash}} | {{CMG}}; {{AE}}{{Akash}} | ||
==Overview== | ==Overview== | ||
A 12 lead ECG is an important diagnostic tool used in the initial evaluation of patients presenting with palpitations. Based on the presence or absence of positive ECG findings physicians can determine the need for ambulatory ECG monitoring, echocardiograpy, lab investigations or electrophysiology study. | |||
==Electrocardiogram== | ==Electrocardiogram== | ||
Revision as of 14:31, 7 August 2020
|
Palpitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Palpitation electrocardiogram On the Web |
|
American Roentgen Ray Society Images of Palpitation electrocardiogram |
|
Risk calculators and risk factors for Palpitation electrocardiogram |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
A 12 lead ECG is an important diagnostic tool used in the initial evaluation of patients presenting with palpitations. Based on the presence or absence of positive ECG findings physicians can determine the need for ambulatory ECG monitoring, echocardiograpy, lab investigations or electrophysiology study.
Electrocardiogram
- A 12 lead ECG along with a detailed history and thorough physical examination form the cornerstone trio in initially approaching a patient presenting with palpitations.
- It should be noted that a patient is rarely symptomatic at the time of presentation as palpitations are frequently a transitory symptom.
- However, this should not take away from an ECG’s importance as an initial diagnostic procedure.
- Nicolas Clementy et al at found that prehospital ECGs and ECGs at admission had the highest positivity rate. [1]
- Based on the presence or absence of ECG findings, a decision should then be made whether the underlying condition is cardiac or not and what further investigative modalities may be required.
- Several studies have suggested that an aggressive diagnostic approach should be employed in patients who are :
- At a high risk of developing arrhythmias (presence of ECG changes on initial evaluation, H/O myocardial and structural heart disease, positive family history) [2]
- Those who remain anxious to have a specific explanation regarding their symptoms. [3]
- Patients with a history of warning symptoms such as presyncope, syncope, dizziness, dyspnea.
- Patients with a history of increase of palpitations on exertion.
- Patients with impaired hemodynamic function.
- Patients with an impaired quality of life attributable to palpitations. [4]
Findings to be wary of on initial 12 Lead ECG Evalutation [5][6]
| Epidemiology | Rate | Rhythm | P waves | PR Interval | QRS complex | Response to maneuvers | Example (Lead 2) | |
|---|---|---|---|---|---|---|---|---|
| Sinus Tachycardia | More common in children and elderly. | Greater than 100 bpm | Regular | Upright, consistent, and normal in morphology | 0.12–0.20 sec and shortens with high heart rate | Less than 0.12 seconds, consistent, and normal in morphology | May break with vagal maneuvers | |
| Atrial Fibrillation | More common in the elderly, following bypass surgery, in mitral valve disease, hyperthyroidism | 110 to 180 bpm | Irregularly irregular | Absent, fibrillatory waves | Absent | Less than 0.12 seconds, consistent, and normal in morphology in the absence of aberrant conduction | Does not break with adenosine or vagal maneuvers | |
| Atrial Flutter | More common in the elderly, after alcohol | 75 (4:1 block), 100 (3:1 block) and 150 (2:1 block) bpm, but 150 is more common | Regular | Sawtooth pattern of P waves at 250 to 350 beats per minute | Varies depending upon the magnitude of the block, but is short | Less than 0.12 seconds, consistent, and normal in morphology | Conduction may vary in response to drugs and maneuvers dropping the rate from 150 to 100 or to 75 bpm | |
| AV Nodal Reentry Tachycardia (AVNRT) | Accounts for 60%-70% of all SVTs. 80% to 90% of cases are due to antegrade conduction down a slow pathway and retrograde up a fast pathway. | In adults the range is 140-250 bpm, but in children the rate can exceed 250 bpm | Regular | The P wave is usually superimposed on or buried within the QRS complex | Cannot be calculated as the P wave is generally obscured by the QRS complex | Less than 0.12 seconds, consistent, and normal in morphology | May break with adenosine or vagal maneuvers | |
| AV Reciprocating Tachycardia (AVRT) | More common in males, whereas AVNRT is more common in females, occurs at a younger age. | More rapid than AVNRT | Regular | A retrograde P wave is seen either at the end of the QRS complex or at the beginning of the ST segment | Less than 0.12 seconds | Less than 0.12 seconds, consistent, and normal in morphology | May break with adenosine or vagal maneuvers | |
| Inappropriate Sinus Tachycardia | The disorder is uncommon. Most patients are in their late 20s to early 30s. More common in women. | > 95 beats per minute. A nocturnal reduction in heart rate is present. There is an inappropriate heart rate response on exertion. | Regular | Normal morphology and precede the QRS complex | Normal and < 0.20 seconds | Less than 0.12 seconds, consistent, and normal in morphology | Does not break with adenosine or vagal maneuvers | |
| Junctional Tachycardia | Common after heart surgery, digitalis toxicity, as an escape rhythm in AV block | > 60 beats per minute | Regular | Usually inverted, may be burried in the QRS complex | The P wave is usually buried in the QRS complex | Less than 0.12 seconds, consistent, and normal in morphology | Does not break with adenosine or vagal maneuvers | |
| Multifocal Atrial Tachycardia (MAT) | High incidence in the elderly and in those with COPD | Atrial rate is > 100 beats per minute (bpm) | Irregular | P waves of varying morphology from at least three different foci | Variable PR intervals, RR intervals, and PP intervals | Less than 0.12 seconds, consistent, and normal in morphology | Does not terminate with adenosine or vagal maneuvers | 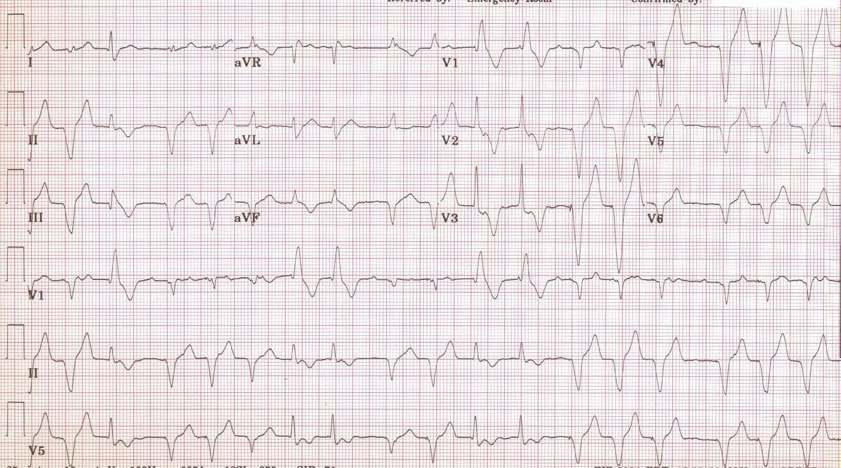
|
| Sinus Node Reentry Tachycardia | Between 2% and 17% among individuals undergoing EKG for SVTs | 100 to 150 bpm | Regular | Upright P waves precede each regular, narrow QRS complex | Short PR interval | Less than 0.12 seconds, consistent, and normal in morphology | Does often terminate with vagal maneuvers unlike sinus tachycardia. | |
| Wolff-Parkinson-White syndrome | Estimated prevalence of WPW syndrome is 100 - 300 per 100,000 in the entire world. | Atrial rate is nearly 300 bpm and ventricular rate is at 150 bpm. | Regular | P wave generally follows the QRS complex due to a bypass tract | Less than 0.12 seconds | Delta wave and evidence of ventricular pre-excitation if there is conduction to the ventricle via ante-grade conduction down an accessory pathway | May break in response to procainamide, adenosine, vagal maneuvers | 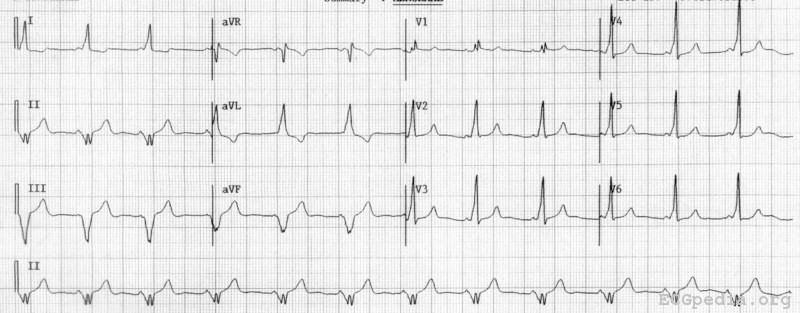
|
| Disease | ECG Findings | Example |
|---|---|---|
| Left Ventricular Hypertrophy | Increased R wave amplitude in the left-sided ECG leads (I, aVL and V4-6) and increased S wave depth in the right-sided leads (III, aVR, V1-3). | 
|
| Extrasystolic Palpitations/Ventricular Tachycardia | Frequent Premature ventricular contractions. | 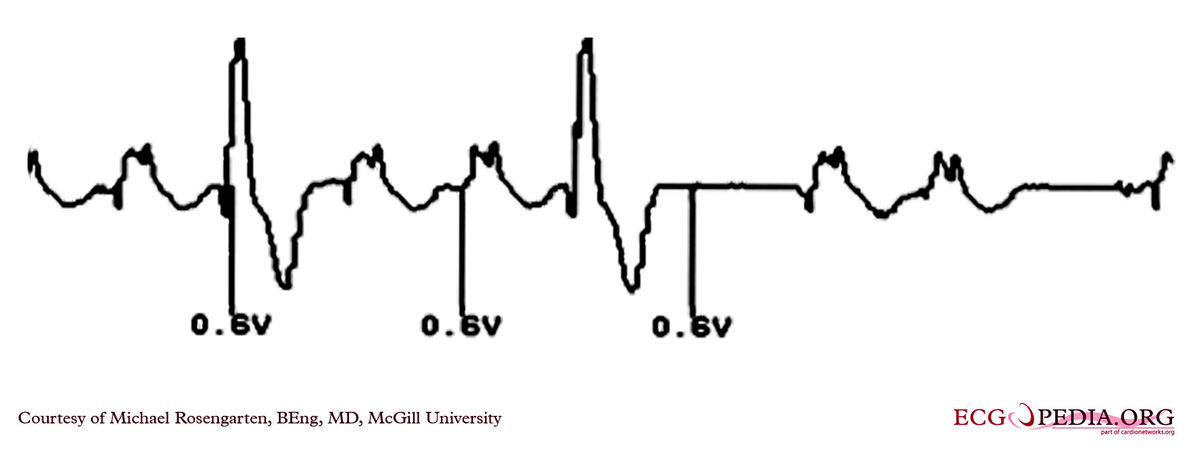
|
| Ischemic Heart Disease | Q waves, T wave inversions, ST segment elevations or depressions. | 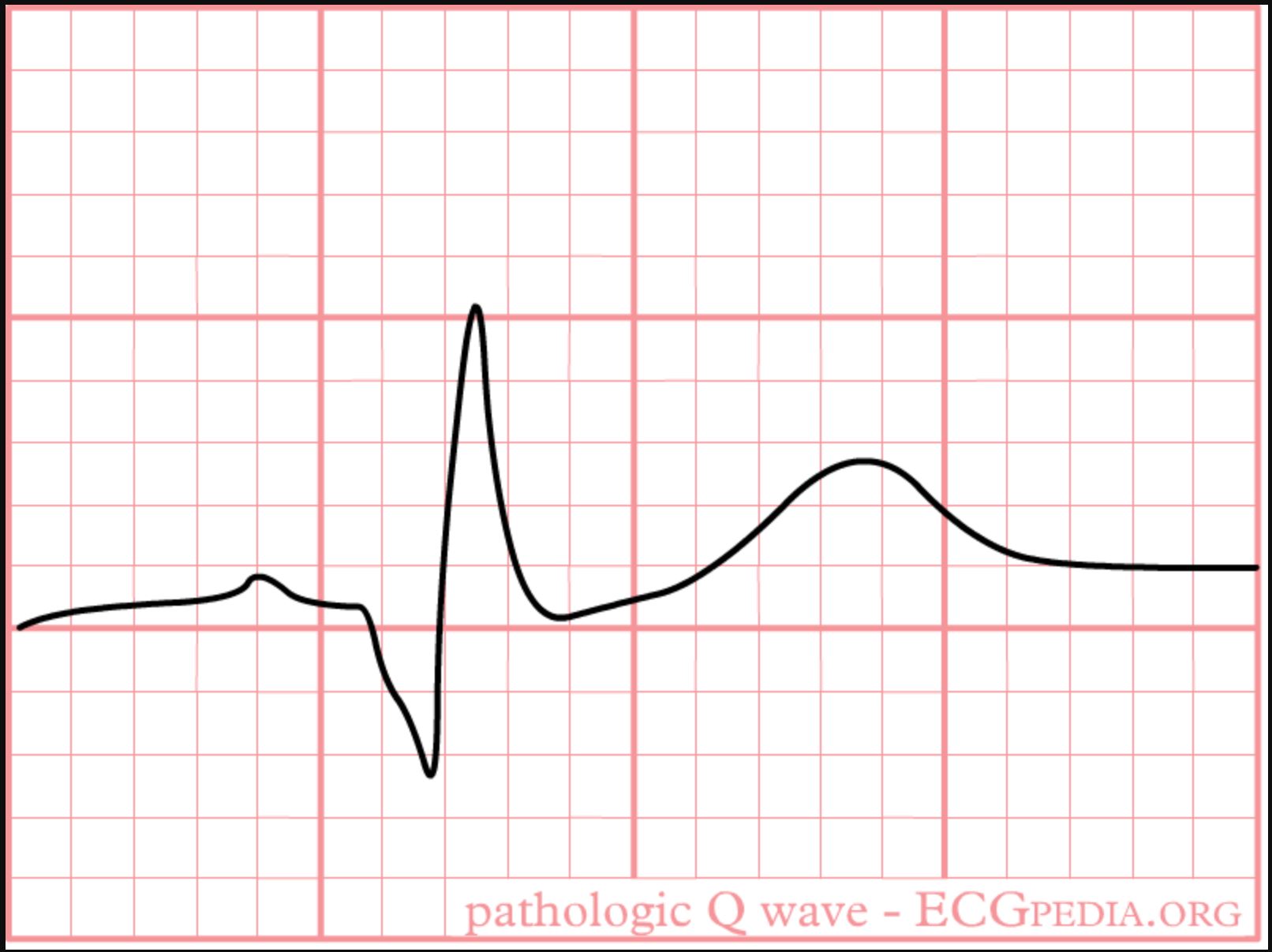
|
| Hypertrophic Cardiomyopathy | Tall R waves in aVL, deep S waves in V3 and T waves changes. | 
|
| Arrhythmogenic right ventricular cardiomyopathy | Inverted T waves or Epsilon waves across right precordial leads (V1-V3) | 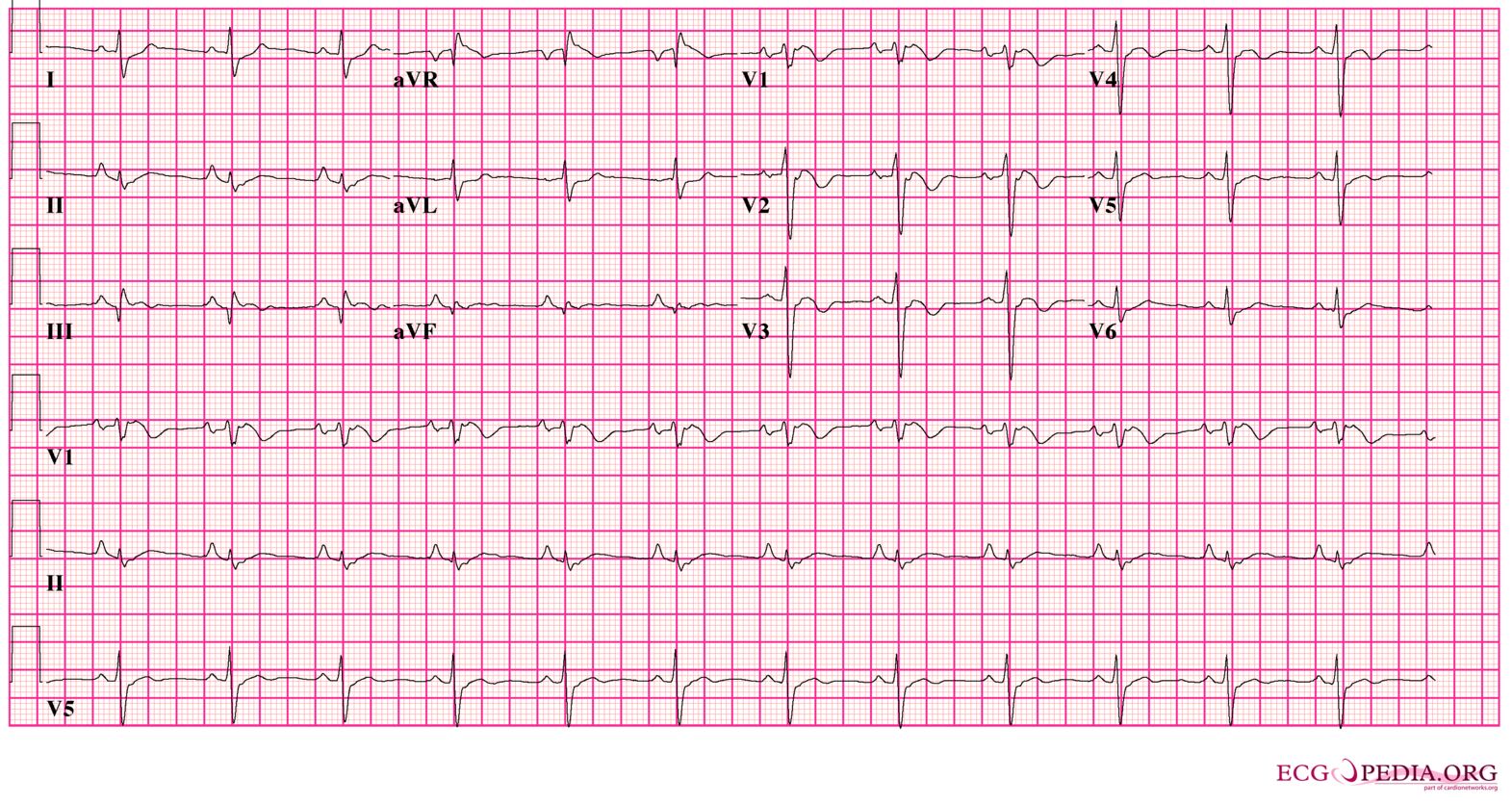
|
| Long QT syndrome | QT interval longer than 460 msec in women and 440 msec for men. | 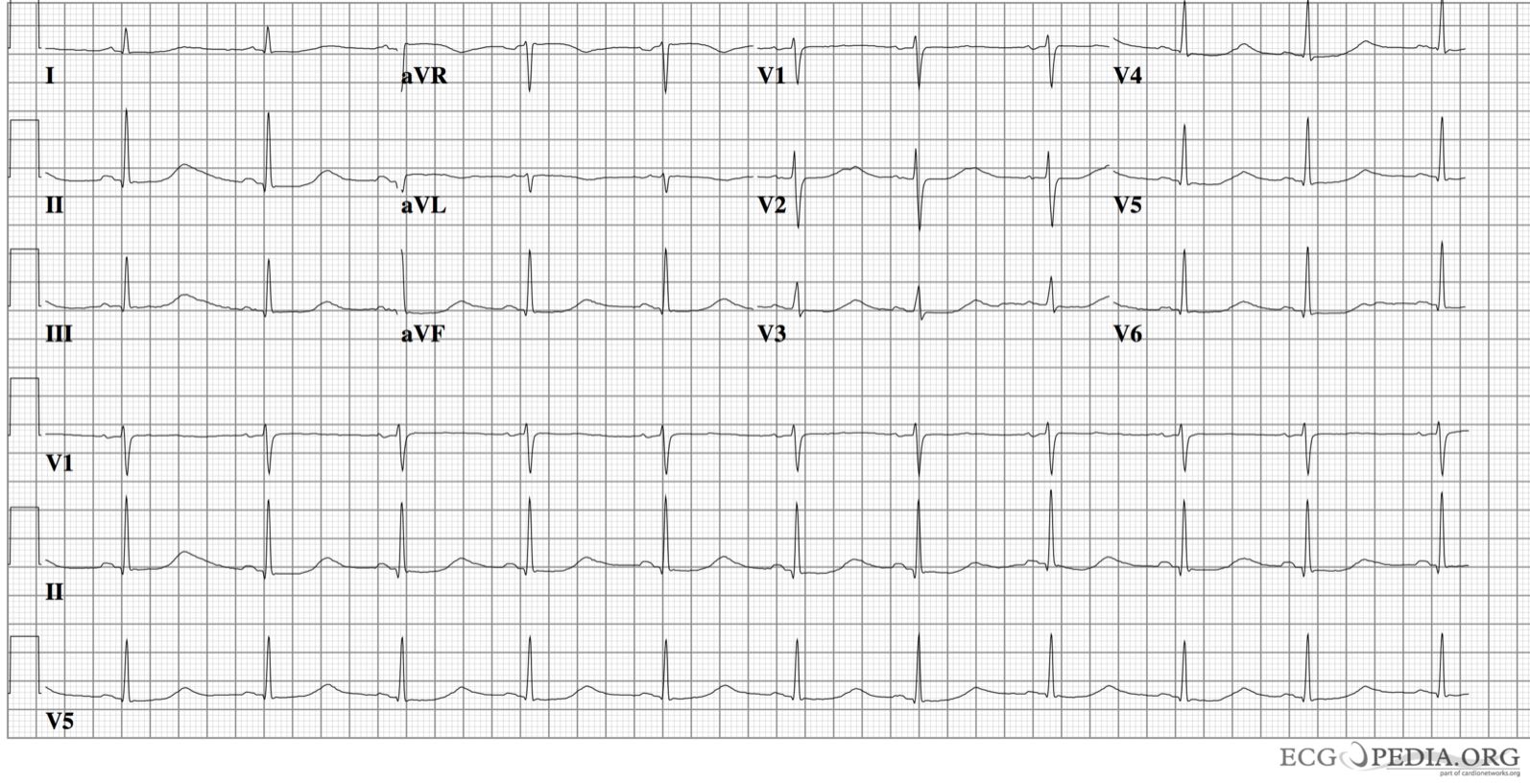
|
| Genetic Arrhythmia syndromes | Long or Short QT interval, Brugada pattern, early repolarisation pattern. | 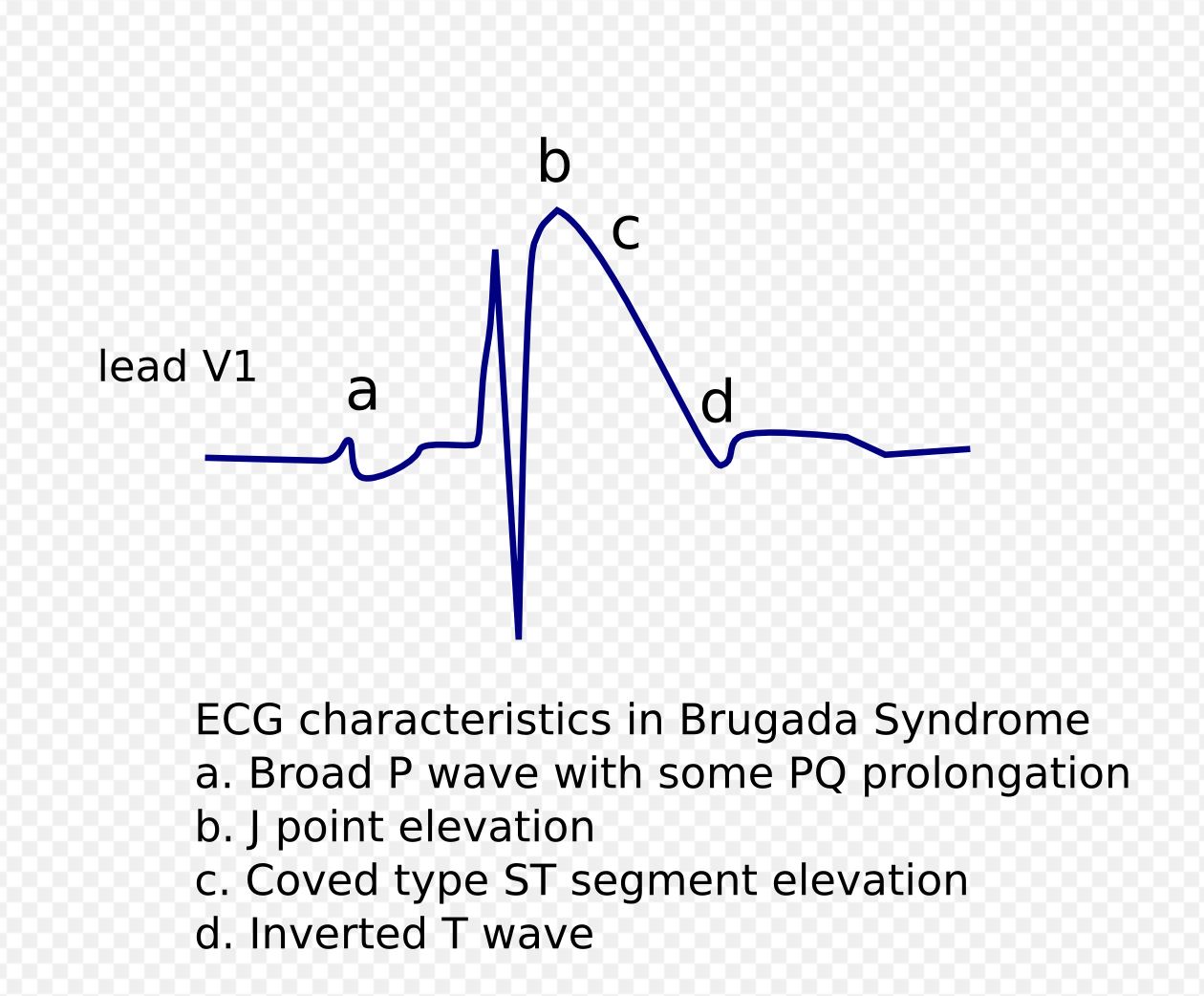
|
Ambulatory Electrocardiography
- Ambulatory ECG devices can be divided into internal and external monitoring devices.
- External Devices include Holter monitors, hospital telemetry devices, event recorders, external loop recorders and mobile cardiac outpatient telemetry.
- Internal devices include pacemakers, implantable cardioverter defibrillators equipped with diagnostic features and implantable loop recorders.
- In addition, modifications to monitoring devices have permitted automatic detection of arrythmia.
- Data is wirelessly transmitted to a central monitoring station which then triggers off an alarm in case of an event.
- This allows for prompt responses from the physician, facilitates early detection of episodes and provides information regarding the mechanism of the arrythmia.
- It is important to note that while the specificity of ambulatory ECG monitoring is high in terms of differentiating between arrhythmogenic and non-arrhythmogenic causes of palpitations, it’s sensitivity depends on the duration of monitoring, patient compliance and the frequency of episodes. [4]
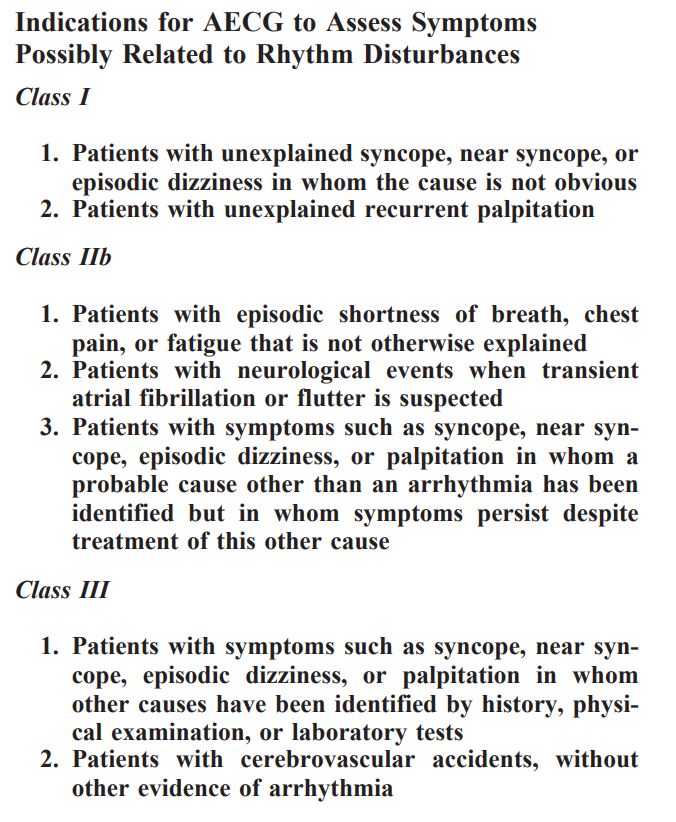
ACC/AHA Guidelines for Ambulatory Electrocardiography[7]
Different Ambulatory Electrocardiography Devices[2][8][6][4]
- Allan Abbott et al found that transtelephonic event monitors had a greater diagnostic yield and were more cost effective when compared to Holter monitors. [3]
References
- ↑ Clementy N, Fourquet A, Andre C, Bisson A, Pierre B, Fauchier L; et al. (2018). "Benefits of an early management of palpitations". Medicine (Baltimore). 97 (28): e11466. doi:10.1097/MD.0000000000011466. PMC 6076186. PMID 29995805.
- ↑ 2.0 2.1 "StatPearls". 2020. PMID 28613787.
- ↑ 3.0 3.1 Abbott AV (2005). "Diagnostic approach to palpitations". Am Fam Physician. 71 (4): 743–50. PMID 15742913.
- ↑ 4.0 4.1 4.2 Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L; et al. (2011). "Management of patients with palpitations: a position paper from the European Heart Rhythm Association". Europace. 13 (7): 920–34. doi:10.1093/europace/eur130. PMID 21697315.
- ↑ Gale CP, Camm AJ (2016). "Assessment of palpitations". BMJ. 352: h5649. doi:10.1136/bmj.h5649. PMID 26739319.
- ↑ 6.0 6.1 Wexler RK, Pleister A, Raman S (2011). "Outpatient approach to palpitations". Am Fam Physician. 84 (1): 63–9. PMID 21766757.
- ↑ Crawford MH, Bernstein SJ, Deedwania PC, DiMarco JP, Ferrick KJ, Garson A; et al. (1999). "ACC/AHA guidelines for ambulatory electrocardiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the guidelines for ambulatory electrocardiography)". Circulation. 100 (8): 886–93. doi:10.1161/01.cir.100.8.886. PMID 10458728.
- ↑ McLellan AJ, Kalman JM (2019). "Approach to palpitations". Aust J Gen Pract. 48 (4): 204–209. doi:10.31128/AJGP-12-17-4436. PMID 31256490.


