Palpitation diagnostic study of choice
|
Palpitation Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Palpitation diagnostic study of choice On the Web |
|
American Roentgen Ray Society Images of Palpitation diagnostic study of choice |
|
Risk calculators and risk factors for Palpitation diagnostic study of choice |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Akash Daswaney, M.B.B.S[2]
Overview
There is no single diagnostic study of choice for palpitations.
Diagnostic Study of Choice
- There is no single diagnostic study of choice for the diagnosis of palpitations, but palpitations can be diagnosed based on a through initial evaluation (a detailed history, physical examination and 12 lead ECG).
- Following this, investigative modalities such as an echocardiography, electrophysiologic study, a different forms of ambulatory ECG monitoring and laboratory investigations such as a renal function test, thyroid function tests and serum drug levels may be employed.
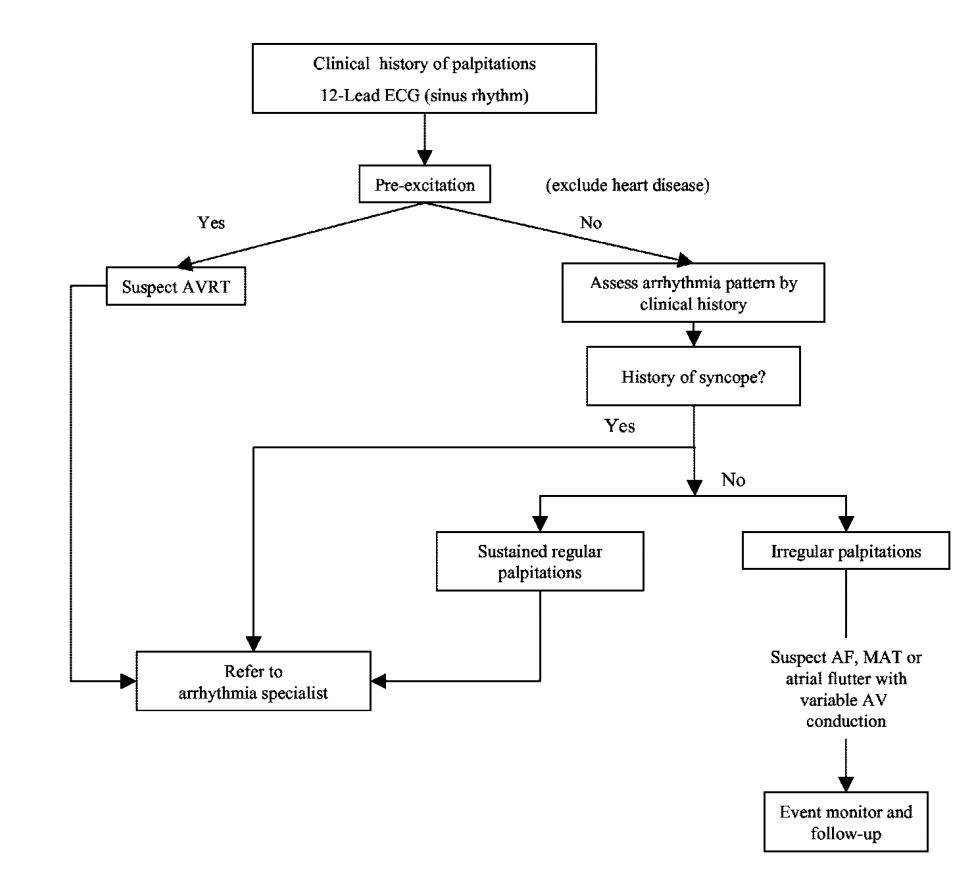
- The following algorithm can be employed when approaching a patient presenting with palpitations. [1][2][3][4] [5]
Different Ambulatory Electrocardiography Devices[6][2][7][3]
| Machine | Description | Indications | Advantages | Disadvantages | Picture |
|---|---|---|---|---|---|
| 12 Lead ECG | •Initial Step in the evaluation of patients of palpitations | •Inexpensive | •Rarely performed during the event | ||
| Handheld ECG | •Palpitations occurring for months to years | •High diagnostic yield
•Always present with the patient |
•Expensive
•Time period from patient activation to event recording is long |
||
| Exercise ECG Stress testing | •Palpitations aggravated by exertion | ||||
| Holter Monitoring | •Continuous beat to beat monitoring system via 12 leads (attached via skin electrodes).
•24-48 hour monitoring system. |
•Symptoms occurring daily or every second day. | •Readily available.
•Need not be activated during the event. •Low cost. •Provides information of asymptomatic episodes. |
•Low diagnostic yield
•Size may prevent trigger events •Clinical Diary completion (upon which symptom correlation depends upon) is a tedious process |
 |
| Continuous- loop event recorder | •Worn for a few days (typically 30 days)
•Older monitors are patient activated and store data once, whereas newer models continuously record data •Provides a one to three lead EKG tracing |
•Symptoms occurring weekly or monthly
•Short lasting palpitations associated with hemodynamic compromise |
•Can be worn for longer periods of time when compared to Holter monitors
•More cost effective •High diagnostic efficacy/yield as it is a patient activated process |
•Not diagnostic for asymptomatic arrythmias as it is a patient activated system (older models
•Devices are uncomfortable and require high maintenance •Requires patient to be compliant |
 |
| Mobile cardiac outpatient telemetry | •External Loop Recorder + Portable Receiver
•Data is wirelessly transmitted to a central monitoring station which then triggers off an alarm in case of an event |
•This allows for prompt responses from the physician, facilitates early detection of episodes and provides information regarding the mechanism of the arrythmia
•Provides information of asymptomatic episodes. |
|||
| Implantable Loop Recorder | •Placed subcutaneously through a small 2cm incision in the left precordial region
•Provides a one lead electrocardiographic tracing |
•Palpitations occurring for months to years
•Rare episodes of palpitations associated with syncope/ hemodynamic compromise •When all other methods of Ambulatory ECG monitoring prove to be inconclusive |
•High diagnostic yield
• Long term monitoring (3 years) •Automatically records arrythmias in addition to patient triggered episodes •Subcutaneous approach avoids long term problems associated with surface electrodes •Does not require patient to be compliant. |
•Invasive procedure may cause local complications
•Expensive •Not readily available |
|
| Pacemakers/Implantable Cardioverter Defibrillators | •Dual chamber Devices which are able to detect and store atrial and ventricular Intracardiac Electrograms. | •Conventional indications for pacemakers/ICDs | •Automatic Arrythmia recording
•Able to discriminate between ventricular and supraventricular arrythmias |
•Invasive
•Increased risk of early/long term local/systemic complications |
 |
- Allan Abbott et al found that transtelephonic event monitors had a greater diagnostic yield and were more cost effective when compared to Holter monitors. [1]
Ammerican Heart Association, Approach to Palpitations
References
- ↑ 1.0 1.1 Abbott AV (2005). "Diagnostic approach to palpitations". Am Fam Physician. 71 (4): 743–50. PMID 15742913.
- ↑ 2.0 2.1 McLellan AJ, Kalman JM (2019). "Approach to palpitations". Aust J Gen Pract. 48 (4): 204–209. doi:10.31128/AJGP-12-17-4436. PMID 31256490.
- ↑ 3.0 3.1 Raviele A, Giada F, Bergfeldt L, Blanc JJ, Blomstrom-Lundqvist C, Mont L; et al. (2011). "Management of patients with palpitations: a position paper from the European Heart Rhythm Association". Europace. 13 (7): 920–34. doi:10.1093/europace/eur130. PMID 21697315.
- ↑ Jamshed N, Dubin J, Eldadah Z (2013). "Emergency management of palpitations in the elderly: epidemiology, diagnostic approaches, and therapeutic options". Clin Geriatr Med. 29 (1): 205–30. doi:10.1016/j.cger.2012.10.003. PMID 23177608.
- ↑ "Palpitations: Evaluation in the Primary Care Setting - American Family Physician".
- ↑ "StatPearls". 2020. PMID 28613787.
- ↑ Wexler RK, Pleister A, Raman S (2011). "Outpatient approach to palpitations". Am Fam Physician. 84 (1): 63–9. PMID 21766757.
- ↑ Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ; et al. (2003). "ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Supraventricular Arrhythmias)". Circulation. 108 (15): 1871–909. doi:10.1161/01.CIR.0000091380.04100.84. PMID 14557344.