Ovarian cancer pathophysiology: Difference between revisions
No edit summary |
No edit summary |
||
| Line 14: | Line 14: | ||
</gallery> | </gallery> | ||
</div> | </div> | ||
==Gross Patholgy== | |||
{| {{table}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Vulvar Carcinomas Subtype'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Gross Pathology'''}} | |||
|- | |||
| Squamous cell carcinoma of vulva|| | |||
* Most lesions originate in the labia, primarily the [[labia majora]]. Other areas affected are the [[clitoris]], [[fourchette]], and the local glands | |||
* Unifocal | |||
|- | |||
|Basal cell carcinoma of vulva|| | |||
* Pearly nodule with telangiectasias | |||
|- | |||
| Vulvar melanoma|| | |||
* Superficial spreading is the most common type | |||
* Brown/black color, but may include reddish brown or white | |||
* Hyperkeratotic, diffused borders with no distinct demarcation | |||
* Irregular and elevated | |||
|- | |||
|} | |||
==Microscopic Pathology== | |||
Histologic subtypes of vulvar cancer include:<ref>{{cite book | last = Hoffman | first = Barbara | title = Williams gynecology | publisher = McGraw-Hill Medical | location = New York | year = 2012 | isbn = 9780071716727 }}</ref><ref> Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015</ref><ref> Basal cell carcinoma | |||
. Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015</ref><ref> Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015</ref> | |||
*Vulvar carcinomas | |||
:* [[Squamous cell carcinoma]] | |||
:* [[Basal cell carcinoma]] | |||
:* Vulvar [[Paget disease]] | |||
:* Adenocarcinoma | |||
:* Transitional cell carcinoma | |||
:* Verrucous carcinoma | |||
:* Merkel cell tumors | |||
*Vulvar [[malignant melanoma]] | |||
*Vulvar [[sarcoma]] | |||
:* [[Leiomyosarcoma]] | |||
:* Malignant fibrous histiocytoma | |||
:* Epithelial sarcoma | |||
{| {{table}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|''' Vulvar Carcinomas Subtype'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Features on Histopathological Microscopic Analysis'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Image'''}} | |||
|- | |||
|- | |||
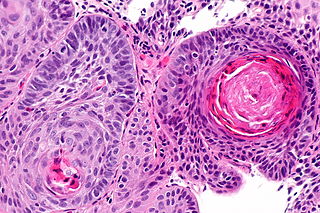
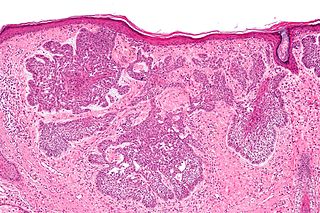
| Squamous cell carcinoma of vulva|| | |||
* Eosinophilia | |||
* Extra large nuclei/bizarre nuclei | |||
* Inflammation (lymphocytes, plasma cells) | |||
* Long rete ridges | |||
* Numerous beeds/blobs of epithelial cells that seem unlikely to be rete ridges | |||
| [[File:Scc.jpg|thumb|none|300px|Squamous cell carcinoma of vulva]] | |||
|- | |||
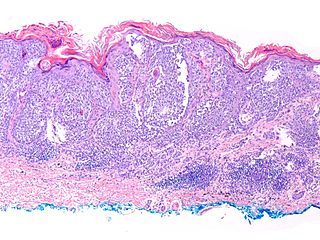
|Basal cell carcinoma of vulva|| | |||
* Basaloid cells - similar in appearance to basal cells | |||
* Moderate blue/grey cytoplasm. | |||
* Dark ovoid/ellipsoid nucleus with uniform chromatin | |||
* Palisading of cells at the edge of the cell nests | |||
* Artefactual separation of cells (forming the nests) from the underlying stroma - key feature | |||
* Surrounded by blue (myxoid) stroma - key feature | |||
| [[File:BCC.jpg|thumb|none|300px|Basal cell carcinoma of vulva]] | |||
|- | |||
| Vulvar melanoma|| | |||
* Presence of intraepidermal lateral spread (most characteristic feature) | |||
* Dermal invasion | |||
* Desmoplasia | |||
* Epidermal hyperplasia | |||
*Appearance of epithelioid cells with occasional spindle cells | |||
| [[File:Melanoma.JPG |thumb|none|300px| Vulvar melanoma]] | |||
|- | |||
|} | |||
==References== | ==References== | ||
Revision as of 16:56, 9 December 2015
|
Ovarian cancer Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Ovarian cancer pathophysiology On the Web |
|
American Roentgen Ray Society Images of Ovarian cancer pathophysiology |
|
Risk calculators and risk factors for Ovarian cancer pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Ovarian cancer is often diagnosed late resulting in a poor overall outcome for the patient. Pathological findings, therefore, often only occur in advanced symptomatic onset and tend to present more as severe pathologic outcomes.
Pathophysiology
-
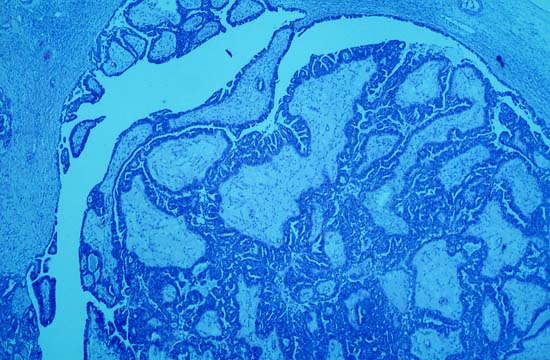
Photomicrograph is from the solid / papillary right ovarian tumor. As shown in this photo, much of the tumor had a papillary pattern with exuberant epithelial proliferation but no obvious stromal invasion. Other areas, such as the one depicted in the second photo, show extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy.
-
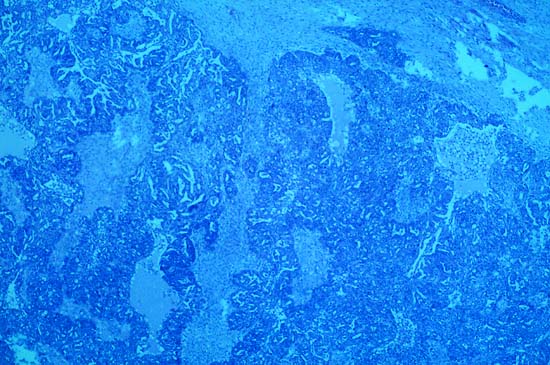
Extensive stromal invasion, the criterion upon which rests the diagnosis of frank malignancy
-
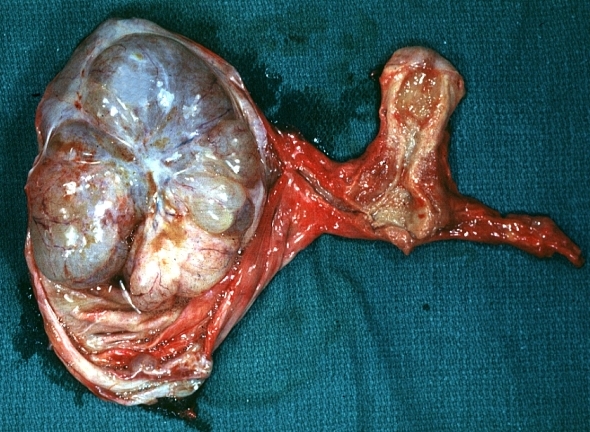
In this TAH-BSO specimen, the right ovary (on the left of the image) has been replaced by a solid serous carcinoma. The contralateral ovarian tumor is grossly cystic and could be termed a "cystadenocarcinoma." The patient had omental metastases and positive peritoneal fluid cytology. This cancer, which was discovered at exploratory laparotomy, apparently developed very rapidly; the patient had a normal pelvic ultrasound exam only 2 months before. (Courtesy of Ed Uthman, MD)
-
Ovary: Mucinous cystadenocarcinoma: Gross, an excellent image of uterus is in picture and thus illustrates the very large size of the ovarian tumor.
Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
Gross Patholgy
| Vulvar Carcinomas Subtype | Features on Gross Pathology |
| Squamous cell carcinoma of vulva |
|
| Basal cell carcinoma of vulva |
|
| Vulvar melanoma |
|
Microscopic Pathology
Histologic subtypes of vulvar cancer include:[1][2][3][4]
- Vulvar carcinomas
- Squamous cell carcinoma
- Basal cell carcinoma
- Vulvar Paget disease
- Adenocarcinoma
- Transitional cell carcinoma
- Verrucous carcinoma
- Merkel cell tumors
- Vulvar malignant melanoma
- Vulvar sarcoma
- Leiomyosarcoma
- Malignant fibrous histiocytoma
- Epithelial sarcoma
References
- ↑ Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.
- ↑ Malignant melanoma. Libre pathology. http://librepathology.org/wiki/index.php/Malignant_melanoma. URL Accessed on September 30, 2015
- ↑ Basal cell carcinoma . Libre pathology. http://librepathology.org/wiki/index.php/Basal_cell_carcinoma. URL Accessed on September 30, 2015
- ↑ Squamous cell carcinoma. Libre pathology. http://librepathology.org/wiki/index.php/Squamous_cell_carcinoma. URL Accessed on September 30, 2015