Osteosarcoma x ray: Difference between revisions
No edit summary |
No edit summary |
||
| Line 24: | Line 24: | ||
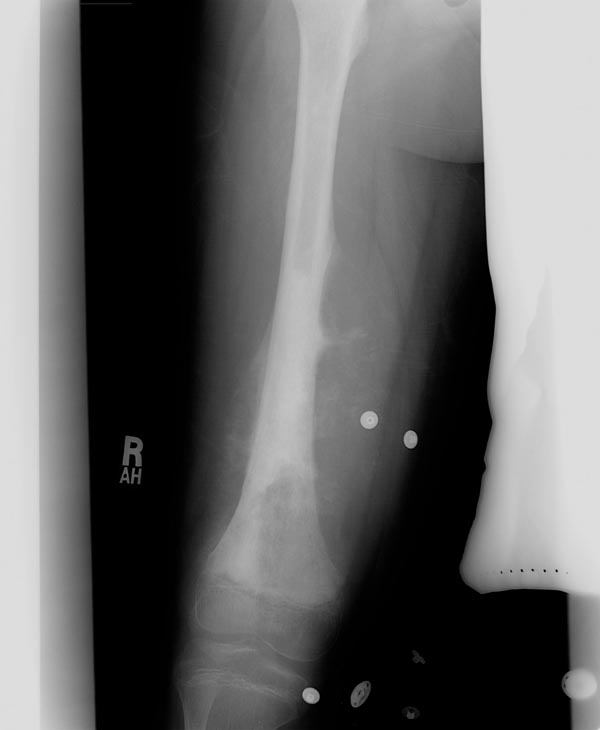
Image:Osteosarcoma-002.jpg|Plain film: Osteosarcoma | Image:Osteosarcoma-002.jpg|Plain film: Osteosarcoma | ||
</gallery> | </gallery> | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 600px" align=center | |||
|valign=top| | |||
|+ | |||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Subtype}} | |||
! style="background: #4479BA; width: 400px;" | {{fontcolor|#FFF|X-Ray findings}} | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; font-weight: bold" | | |||
:Intracortical osteosarcoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Presents as an oval intracortical geographic osteolytic lesion in the diaphysis with surrounding sclerosis | |||
*Measures approximately 4 cm in length | |||
*Multiple calcific foci can be seen within the lytic region, suggesting osteoid matrix. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:Parosteal osteosarcoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Large lobulated exophytic, 'cauliflower-like' mass with central dense ossification adjacent to the bone. | |||
*String sign: Thin radiolucent line separating the tumor from cortex, observed in 30% of cases. | |||
*Tumor stalk: Grows within tumor in late stages and obliterates the radiolucent cleavage plane. | |||
*+/- soft tissue mass. | |||
*Cortical thickening without aggressive periosteal reaction is often seen. | |||
*Tumor extension into medullary cavity is frequently observed. | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
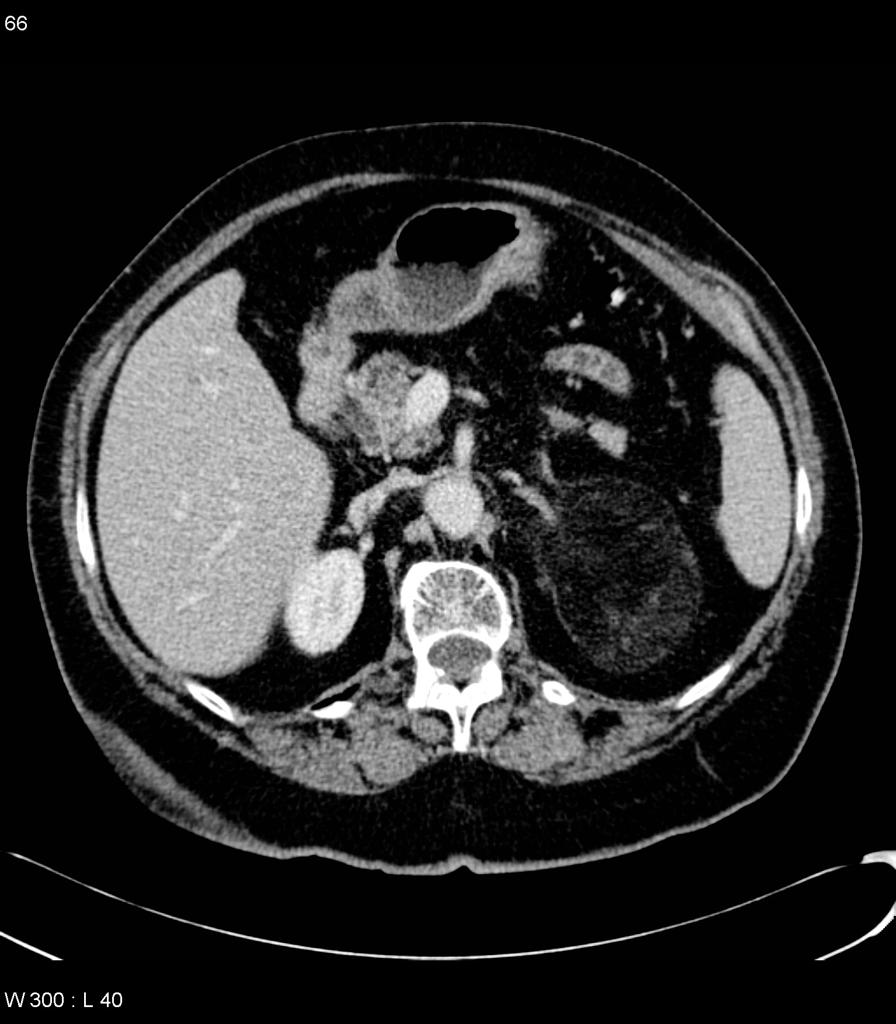
:[[Oncocytoma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*May contain fat | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:[[Wilm's tumor]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*May contain fat | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:Retroperitoneal [[sarcoma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*[[Liposarcoma]] | |||
*[[Leiomyosarcoma]] | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:[[Renal cell carcinoma]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Sarcomatoid differentiation | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:Renal leiomyoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Very rare | |||
*Desmin +ve | |||
*HMB-45 -ve | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:Perirenal fat entrapment | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Renal junctional parenchymal defect | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC;font-weight: bold" | | |||
:Adrenal myelolipoma | |||
| style="padding: 5px 5px; background: #F5F5F5;" | | |||
*Fat in renal parenchyma | |||
[[file:Adrenal-myelolipoma.jpg | 200px]] | |||
|- | |||
|} | |||
===Extra skeletal osteosarcoma=== | ===Extra skeletal osteosarcoma=== | ||
Revision as of 13:15, 29 September 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
|
Osteosarcoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteosarcoma x ray On the Web |
|
American Roentgen Ray Society Images of Osteosarcoma x ray |
Overview
On x-ray, osteosarcoma is characterized by medullary and cortical bone destruction, periosteal reaction, tumor matrix calcification and soft tissue mass.[1]
X Ray
Conventional radiography continues to play an important role in diagnosis of osteosarcoma. Typical appearances of conventional high grade osteosarcoma include:[1]
- Medullary and cortical bone destruction.
- Wide zone of transition, permeative or moth-eaten appearance.
- Aggressive periosteal reaction characterized by:
- Sunburst appearance
- Codman triangle
- Lamellated (onion skin) reaction: less frequently seen
- Soft-tissue mass.
- Tumor matrix ossification/calcification.
- Variable: reflects a combination of the amount of tumor bone production, calcified matrix, and osteoid.
- Ill-defined fluffy or cloud-like cf. to the rings and arcs of chondroid lesions.
-
Plain film: Osteosarcoma
-
Plain film: Osteosarcoma
| Subtype | X-Ray findings |
|---|---|
|
|
|
|
| |
| |
|
|
| |
|
|
|
|
|
|
Extra skeletal osteosarcoma
On X-ray, extra skeletal osteosarcoma appears as soft tissue density with variable amount of calcification which represents osteoid matrix formation, and is seen in approximately 50% of cases.
Parosteal osteosarcoma
- Large lobulated exophytic, 'cauliflower-like' mass with central dense ossification adjacent to the bone.
- String sign: Thin radiolucent line separating the tumor from cortex, observed in 30% of cases.
- Tumor stalk: Grows within tumor in late stages and obliterates the radiolucent cleavage plane.
- +/- soft tissue mass.
- Cortical thickening without aggressive periosteal reaction is often seen.
- Tumor extension into medullary cavity is frequently observed.
Intracortical osteosarcoma
- It typically presents as an oval intracortical geographic osteolytic lesion in the diaphysis with surrounding sclerosis and usually measures about 4 cm in length. *Multiple calcific foci can be seen within the lytic region, suggesting osteoid matrix.
Periosteal osteosarcoma
- Typically seen as a broad-based surface soft-tissue mass causing extrinsic erosion of thickened underlying diaphyseal cortex and perpendicular periosteal reaction extending into the soft-tissue component.
Low grade osteosarcoma
- Because the fibrous dysplasia and central low-grade osteosarcoma are so similar histologically, the radiographic features are an extremely important part of the diagnosis.
- Radiographic features of low grade osteosarcomas are variable.
- Most common pattern is as a large intracompartmental expansile lytic fibro-osseous lesion with coarsely thick or thin incomplete trabeculations. Another less common pattern is as a dense sclerotic lesion.
- Cortical erosion and soft tissue extension is also a common feature.
Telangiectatic osteosarcoma
- Typically seen as an expansile lytic metaphyseal bony lesion.
- Geographic bony destruction with wide zone of transition tends to be more common than permeative bony destruction.
- Less osteoid matrix compared from conventional type.
References
- ↑ 1.0 1.1 Osteosarcoma. Dr Amir Rezaee ◉ and Dr Frank Gaillard ◉ et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/osteosarcoma