Osteosarcoma pathophysiology: Difference between revisions
(Mahshid) |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}};{{AE}} {{PSK}} | {{CMG}};{{AE}} {{PSK}} | ||
{{Osteosarcoma}} | {{Osteosarcoma}} | ||
==Overview== | ==Overview== | ||
The osteosarcomas may be localized at the end of the long bones (commonly in the [[metaphysis]]). Most often osteosarcoma affects the upper end of the [[tibia]], [[humerus]], or lower end of the [[femur]]. On gross pathology, areas of bone formation, hemorrhage, fibrosis, and cystic degeneration on cut surface are characteristic findings of osteosarcoma. On microscopic histopathological analysis, presence of [[osteoid]] within the tumor, [[pleomorphic]] cells, [[anaplastic]] cells, and atypical [[mitoses]] are characteristic findings of osteosarcoma. Osteosarcoma may be associated with hereditary syndromes such as [[Li-Fraumeni syndrome]] and [[Rothmund-Thomson Syndrome]]. | The osteosarcomas may be localized at the end of the [[Long bone|long bones]] (commonly in the [[metaphysis]]). Most often osteosarcoma affects the upper end of the [[tibia]], [[humerus]], or lower end of the [[femur]]. On [[gross pathology]], areas of bone formation, [[hemorrhage]], [[fibrosis]], and cystic [[degeneration]] on cut surface are characteristic findings of osteosarcoma. On microscopic [[histopathological]] analysis, presence of [[osteoid]] within the [[tumor]], [[pleomorphic]] cells, [[anaplastic]] cells, and atypical [[mitoses]] are characteristic findings of osteosarcoma. Osteosarcoma may be associated with hereditary syndromes such as [[Li-Fraumeni syndrome]] and [[Rothmund-Thomson Syndrome]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
The osteosarcomas may be localized at the end of the long bones (commonly in the [[metaphysis]]). Most often osteosarcoma affects the upper end of the [[tibia]], [[humerus]], or lower end of the [[femur]]. Osteosarcomas tend to occur at the sites of bone growth, presumably because proliferation makes osteoblastic cells in this region prone to acquire mutations that could lead to transformation of cells (the ''RB'' gene and ''p53'' gene are commonly involved). | The osteosarcomas may be localized at the end of the [[long bones]] (commonly in the [[metaphysis]]). Most often osteosarcoma affects the upper end of the [[tibia]], [[humerus]], or lower end of the [[femur]]. Osteosarcomas tend to occur at the sites of bone growth, presumably because proliferation makes [[Osteoblastic osteosarcoma|osteoblastic cells]] in this region prone to acquire mutations that could lead to transformation of cells (the ''RB'' gene and [[P53 gene|''p53'' gene]] are commonly involved). | ||
==Gross Pathology== | ==Gross Pathology== | ||
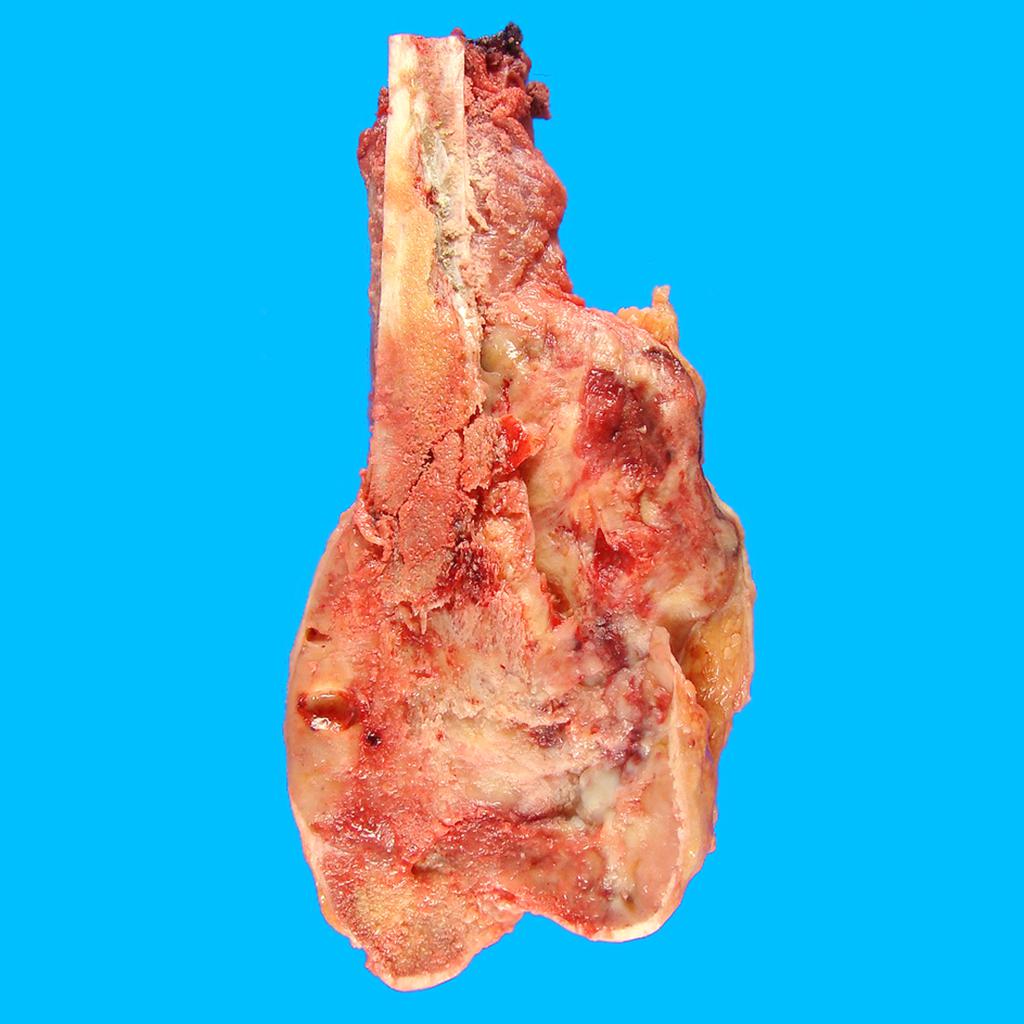
*Macroscopically, osteosarcomas are solid, hard, and bulky tumors. | *Macroscopically, osteosarcomas are [[solid]], hard, and bulky tumors. | ||
*Heterogeneous cut surface demonstrates areas of [[hemorrhage]], [[fibrosis]] and cystic degeneration. | *[[Heterogeneous]] cut surface demonstrates areas of [[hemorrhage]], [[fibrosis]] and cystic [[degeneration]]. | ||
*Areas of bone formation are characteristic of osteosarcomas, with the degree of bone formation varying widely. | *Areas of bone formation are characteristic of osteosarcomas, with the degree of bone formation varying widely. | ||
*The tumor is irregular ("fir-tree" or "sun-burst" appearance on X-ray examination) due to the tumor spicules of calcified bone radiating in right angles. These right angles form what is known as [[Codman's triangle]], which is characteristic but not diagnostic of osteosarcoma. Surrounding tissues are infiltrated. | *The tumor is irregular ("fir-tree" or "sun-burst" appearance on X-ray examination) due to the tumor spicules of calcified bone radiating in right angles. These right angles form what is known as [[Codman's triangle]], which is characteristic but not diagnostic of osteosarcoma. Surrounding tissues are infiltrated. | ||
{| align | {| align="" | ||
|-valign="top" | |- valign="top" | ||
| [[Image:Osteosarcoma (2).jpg|thumb|350px|Osteosarcoma-distal femur-pathology<ref name=radio>Image courtesy of Dr Frank Gaillard. [http://www.radiopaedia.org Radiopaedia] (original file [http://radiopaedia.org/cases/osteosarcoma-distal-femur-pathology]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC</ref>]] | | [[Image:Osteosarcoma (2).jpg|thumb|350px|Osteosarcoma-distal femur-pathology<ref name="radio">Image courtesy of Dr Frank Gaillard. [http://www.radiopaedia.org Radiopaedia] (original file [http://radiopaedia.org/cases/osteosarcoma-distal-femur-pathology]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC</ref>]] | ||
|} | |} | ||
==Microscopic Pathology== | ==Microscopic Pathology== | ||
*On microscopic histopathological analysis, | *On microscopic [[histopathological]] analysis, a characteristic feature of osteosarcoma is presence of [[osteoid]] (bone formation) within the tumor. | ||
*Tumor cells are [[pleomorphic]], [[anaplastic]], giant, and display numerous atypical [[mitoses]]. | *[[Tumor cell|Tumor cells]] are [[pleomorphic]], [[anaplastic]], giant, and display numerous atypical [[mitoses]]. | ||
*These cells produce [[osteoid]] describing irregular [[trabeculae]] (amorphous, [[eosinophilic]]/pink) with or without central [[calcification]] ([[hematoxylinophilic]]/blue, granular) - tumor bone. | *These cells produce [[osteoid]] describing irregular [[trabeculae]] ([[amorphous]], [[eosinophilic]]/pink) with or without central [[calcification]] ([[hematoxylinophilic]]/blue, granular) - tumor bone. | ||
*Tumor cells are included in the [[osteoid]] matrix. Depending on the features of the tumor cells present (whether they resemble bone cells, cartilage cells or fibroblast cells), the tumor can be | *[[Tumor cell|Tumor cells]] are included in the [[osteoid]] matrix. Depending on the features of the [[Tumor cell|tumor cells]] present (whether they resemble [[bone cells]], [[cartilage]] cells or [[fibroblast]] cells), the tumor can be sub classified. The presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors bloodstream metastasis. | ||
<gallery> | <gallery> | ||
| Line 33: | Line 34: | ||
*Characteristic features on microscopic analysis are variable depending on the osteosarcoma subtype: | *Characteristic features on microscopic analysis are variable depending on the osteosarcoma subtype: | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align=center | {| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | ||
|valign=top| | | valign="top" | | ||
|+ | |+ | ||
! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Subtype}} | ! style="background: #4479BA; width: 200px;" | {{fontcolor|#FFF|Subtype}} | ||
| Line 42: | Line 43: | ||
:Telangiectatic osteosarcoma | :Telangiectatic osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Most osteosarcomas have a small telangiectatic component but in order to be classified as a telangiectatic osteosarcoma the telangiectatic component should comprise more than 90%.<ref name=radio2> Osteosarcoma. Dr Yuranga Weerakkody◉ et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/telangiectatic-osteosarcoma</ref> | *Most osteosarcomas have a small telangiectatic component but in order to be classified as a telangiectatic osteosarcoma the telangiectatic component should comprise more than 90%.<ref name="radio2">Osteosarcoma. Dr Yuranga Weerakkody◉ et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/telangiectatic-osteosarcoma</ref> | ||
*Most of the tumor comprises of large blood filled spaces separated by thin bony septations. | *Most of the tumor comprises of large blood filled spaces separated by thin bony septations. | ||
*Microscopically, the tumor consists of vascular sinusoids surrounded by thin septae, osteoid matrix and cells with significant pleomorphism and high mitotic rate. | *Microscopically, the tumor consists of vascular sinusoids surrounded by thin septae, osteoid matrix and cells with significant pleomorphism and high mitotic rate. | ||
| Line 49: | Line 50: | ||
:Low grade osteosarcoma | :Low grade osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Histologically it is a low grade tumor which occurs in the medullary canal of long bones.<ref name=radio2> Osteosarcoma.Dr Yuranga Weerakkody◉ and Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/low-grade-osteosarcoma</ref> | *Histologically it is a low grade tumor which occurs in the medullary canal of long bones.<ref name="radio2">Osteosarcoma.Dr Yuranga Weerakkody◉ and Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/low-grade-osteosarcoma</ref> | ||
*It contains osseous matrix with fibrous stroma and there is variable amount of bone production. | *It contains osseous matrix with fibrous stroma and there is variable amount of bone production. | ||
*Histologic pattern is similar to [[fibrous dysplasia]] and low grade parosteal osteosarcoma. | *Histologic pattern is similar to [[fibrous dysplasia]] and low grade parosteal osteosarcoma. | ||
| Line 56: | Line 57: | ||
:Periosteal osteosarcoma | :Periosteal osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Periosteal osteosarcoma arise from the inner germinative layer of [[periosteum]].<ref name=radio2> Osteosarcoma. Dr Henry Knipe◉ and Dr Sam Kyle et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/periosteal-osteosarcoma</ref> | *Periosteal osteosarcoma arise from the inner germinative layer of [[periosteum]].<ref name="radio2">Osteosarcoma. Dr Henry Knipe◉ and Dr Sam Kyle et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/periosteal-osteosarcoma</ref> | ||
*The cytologic grade of this tumor is higher than parosteal osteosarcoma and lower than conventional osteosarcomas. | *The cytologic grade of this tumor is higher than parosteal osteosarcoma and lower than conventional osteosarcomas. | ||
*Periosteal osteosarcoma is considered as intermediate grade osteosarcoma (grade 2). | *Periosteal osteosarcoma is considered as intermediate grade osteosarcoma (grade 2). | ||
| Line 64: | Line 65: | ||
:Intracortical osteosarcoma | :Intracortical osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Intracortical osteosarcoma is a low grade tumor of cortical bones and it typically does not extend into [[medullary canal]] and surrounding soft tissue until late stage of the disease.<ref name=radio2> Osteosarcoma. Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/intracortical-osteosarcoma</ref> | *Intracortical osteosarcoma is a low grade tumor of cortical bones and it typically does not extend into [[medullary canal]] and surrounding soft tissue until late stage of the disease.<ref name="radio2">Osteosarcoma. Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/intracortical-osteosarcoma</ref> | ||
*Histologically characterazied as a sclerosing variant of the osteosarcoma. | *Histologically characterazied as a sclerosing variant of the osteosarcoma. | ||
*Intracortical osteosarcoma contains [[osteoid]] matrix with few fibroblastic foci within and mild degree of cellular atypia. | *Intracortical osteosarcoma contains [[osteoid]] matrix with few fibroblastic foci within and mild degree of cellular atypia. | ||
| Line 71: | Line 72: | ||
:Parosteal osteosarcoma | :Parosteal osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Parosteal osteosarcoma originates from the outer fibrous layer of [[periosteum]].<ref name=radio2> Osteosarcoma.Dr Frank Gaillard◉ et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/parosteal-osteosarcoma-1</ref> | *Parosteal osteosarcoma originates from the outer fibrous layer of [[periosteum]].<ref name="radio2">Osteosarcoma.Dr Frank Gaillard◉ et al.Radiopaedia.org 2015. http://radiopaedia.org/articles/parosteal-osteosarcoma-1</ref> | ||
*They are composed of a dense osteoid component attached to the outer cortex over a narrow zone. | *They are composed of a dense osteoid component attached to the outer cortex over a narrow zone. | ||
*It exhibits extensive bone matrix and minimal fibroblastic cellular atypia, and as such is considered to be a low grade tumor. | *It exhibits extensive bone matrix and minimal fibroblastic cellular atypia, and as such is considered to be a low grade tumor. | ||
| Line 78: | Line 79: | ||
:Extraskeletal osteosarcoma | :Extraskeletal osteosarcoma | ||
| style="padding: 5px 5px; background: #F5F5F5;" | | | style="padding: 5px 5px; background: #F5F5F5;" | | ||
*Microscopically, it is typically a high grade [[spindle cell]] malignancy with [[osteoid]] and chondroid matrix.<ref name=radio2> Osteosarcoma.Dr Amir Rezaee◉ and Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/extra-skeletal-osteosarcoma-1</ref> | *Microscopically, it is typically a high grade [[spindle cell]] malignancy with [[osteoid]] and chondroid matrix.<ref name="radio2">Osteosarcoma.Dr Amir Rezaee◉ and Dr Prashant Mudgal et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/extra-skeletal-osteosarcoma-1</ref> | ||
*The histologic appearance of extraskeletal osteosarcoma resembles malignant [[fibrous histiocytoma]], osteoblastic osteosarcoma and chondroblastic osteosarcoma. | *The histologic appearance of extraskeletal osteosarcoma resembles malignant [[fibrous histiocytoma]], osteoblastic osteosarcoma and chondroblastic osteosarcoma. | ||
|- | |- | ||
| Line 91: | Line 92: | ||
These syndromes are extremely rare within the osteosarcoma diagnosis and probably represent less than 0.5% of those diagnosed. | These syndromes are extremely rare within the osteosarcoma diagnosis and probably represent less than 0.5% of those diagnosed. | ||
<gallery | <gallery perrow="3"> | ||
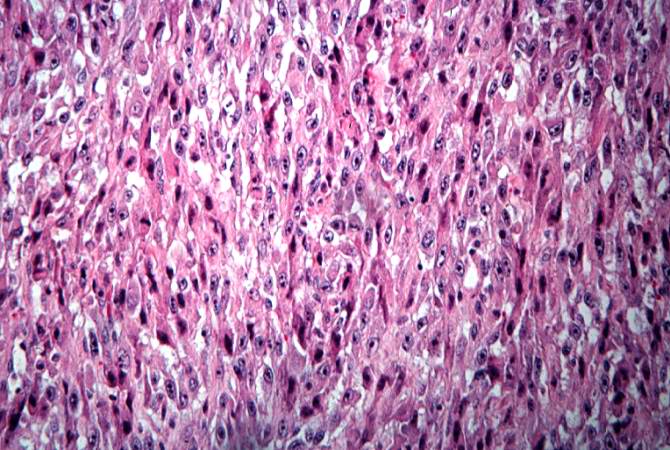
Image:Osteosarcoma case 009.jpg|This high-power photomicrograph demonstrates the cellular growth pattern. Note that the cells are fusiform and they grow in sheets.<ref name=UAB Pathology education instructional resource> Osteosarcoma.peir.path.uab.edu/wiki.http://peir.path.uab.edu/wiki/IPLab:Lab_7:Osteosarcoma</ref> | Image:Osteosarcoma case 009.jpg|This high-power photomicrograph demonstrates the cellular growth pattern. Note that the cells are fusiform and they grow in sheets.<ref name=UAB Pathology education instructional resource> Osteosarcoma.peir.path.uab.edu/wiki.http://peir.path.uab.edu/wiki/IPLab:Lab_7:Osteosarcoma</ref> | ||
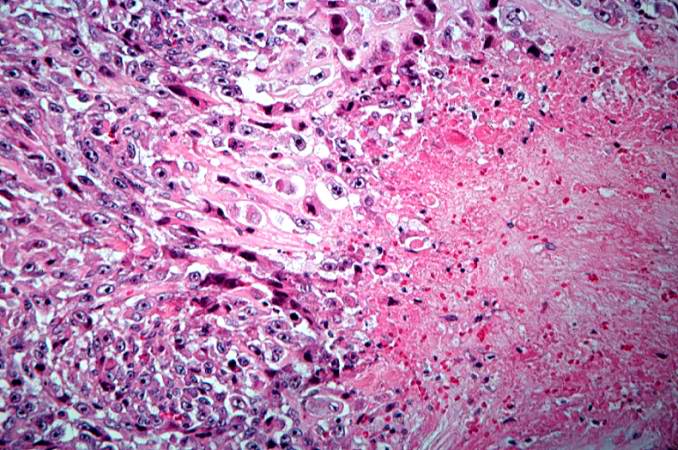
Image:Osteosarcoma case 010.jpg|This high-power photomicrograph demonstrates the growth pattern and the cell morphology.<ref name=UAB Pathology education instructional resource> Osteosarcoma.peir.path.uab.edu/wiki.http://peir.path.uab.edu/wiki/IPLab:Lab_7:Osteosarcoma</ref> | Image:Osteosarcoma case 010.jpg|This high-power photomicrograph demonstrates the growth pattern and the cell morphology.<ref name=UAB Pathology education instructional resource> Osteosarcoma.peir.path.uab.edu/wiki.http://peir.path.uab.edu/wiki/IPLab:Lab_7:Osteosarcoma</ref> | ||
Revision as of 14:32, 29 May 2018
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2];Associate Editor(s)-in-Chief: Suveenkrishna Pothuru, M.B,B.S. [3]
|
Osteosarcoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteosarcoma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Osteosarcoma pathophysiology |
|
Risk calculators and risk factors for Osteosarcoma pathophysiology |
Overview
The osteosarcomas may be localized at the end of the long bones (commonly in the metaphysis). Most often osteosarcoma affects the upper end of the tibia, humerus, or lower end of the femur. On gross pathology, areas of bone formation, hemorrhage, fibrosis, and cystic degeneration on cut surface are characteristic findings of osteosarcoma. On microscopic histopathological analysis, presence of osteoid within the tumor, pleomorphic cells, anaplastic cells, and atypical mitoses are characteristic findings of osteosarcoma. Osteosarcoma may be associated with hereditary syndromes such as Li-Fraumeni syndrome and Rothmund-Thomson Syndrome.
Pathophysiology
The osteosarcomas may be localized at the end of the long bones (commonly in the metaphysis). Most often osteosarcoma affects the upper end of the tibia, humerus, or lower end of the femur. Osteosarcomas tend to occur at the sites of bone growth, presumably because proliferation makes osteoblastic cells in this region prone to acquire mutations that could lead to transformation of cells (the RB gene and p53 gene are commonly involved).
Gross Pathology
- Macroscopically, osteosarcomas are solid, hard, and bulky tumors.
- Heterogeneous cut surface demonstrates areas of hemorrhage, fibrosis and cystic degeneration.
- Areas of bone formation are characteristic of osteosarcomas, with the degree of bone formation varying widely.
- The tumor is irregular ("fir-tree" or "sun-burst" appearance on X-ray examination) due to the tumor spicules of calcified bone radiating in right angles. These right angles form what is known as Codman's triangle, which is characteristic but not diagnostic of osteosarcoma. Surrounding tissues are infiltrated.
 |
Microscopic Pathology
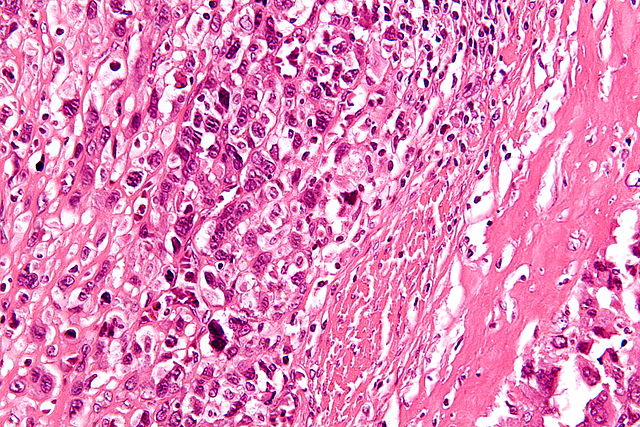
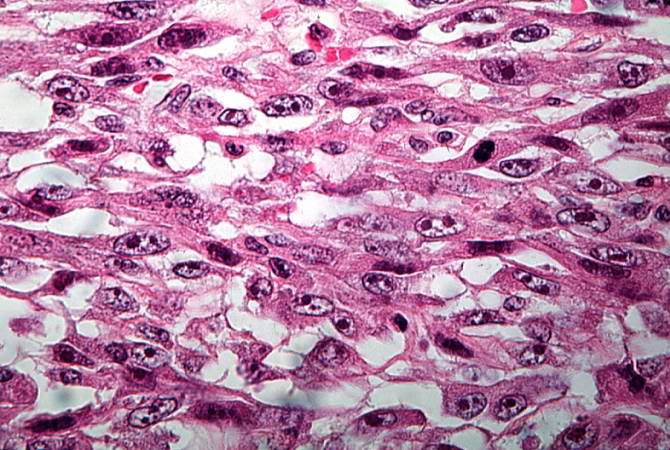
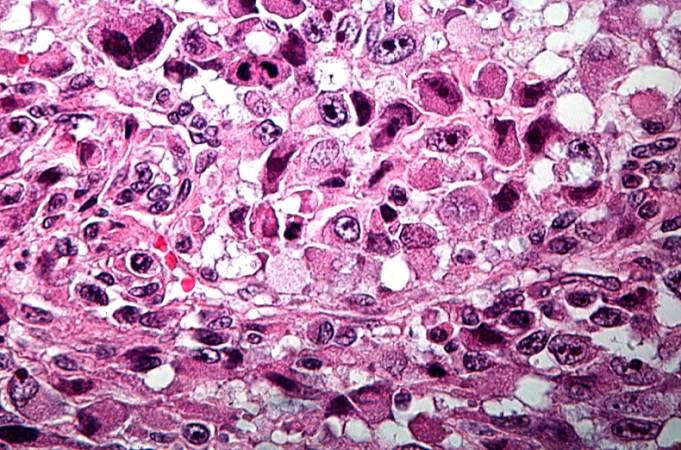
- On microscopic histopathological analysis, a characteristic feature of osteosarcoma is presence of osteoid (bone formation) within the tumor.
- Tumor cells are pleomorphic, anaplastic, giant, and display numerous atypical mitoses.
- These cells produce osteoid describing irregular trabeculae (amorphous, eosinophilic/pink) with or without central calcification (hematoxylinophilic/blue, granular) - tumor bone.
- Tumor cells are included in the osteoid matrix. Depending on the features of the tumor cells present (whether they resemble bone cells, cartilage cells or fibroblast cells), the tumor can be sub classified. The presence of immature blood vessels (sarcomatous vessels lacking endothelial cells) favors bloodstream metastasis.
-
Histology of conventional osteosarcoma[1]
-
High-magnification micrograph showing osteoid formation in an osteosarcoma H&E stain
- Characteristic features on microscopic analysis are variable depending on the osteosarcoma subtype:
| Subtype | Features on Histopathological Microscopic Analysis |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
Genetics
Hereditary syndromes of osteosarcoma include:[3]
- RECQL4 gene mutations
- RB1 gene mutations (also implicated in retinoblastoma)
- Li-Fraumeni syndrome
- Rothmund-Thomson Syndrome
These syndromes are extremely rare within the osteosarcoma diagnosis and probably represent less than 0.5% of those diagnosed.
-
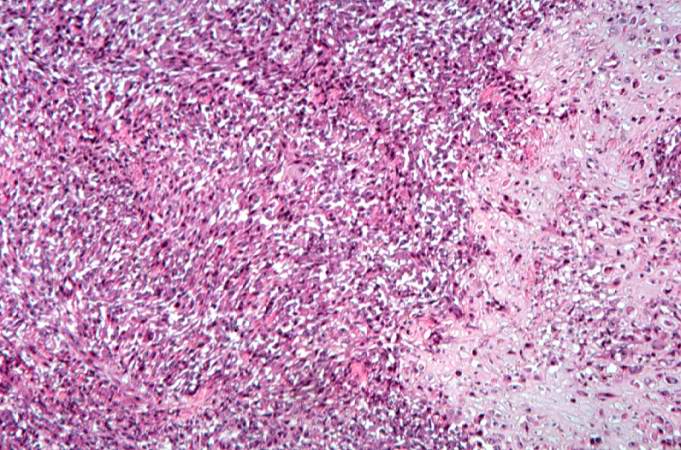
This high-power photomicrograph demonstrates the cellular growth pattern. Note that the cells are fusiform and they grow in sheets.
-
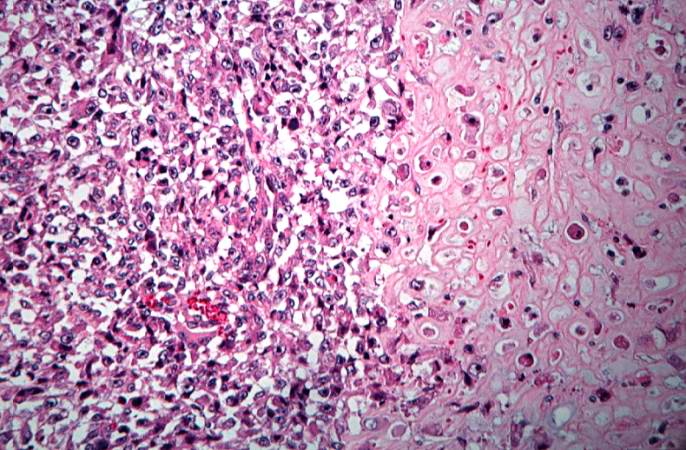
This high-power photomicrograph demonstrates the growth pattern and the cell morphology.
-
This is a high-power photomicrograph of the tumor cell morphology and the periosteum (arrow).
-
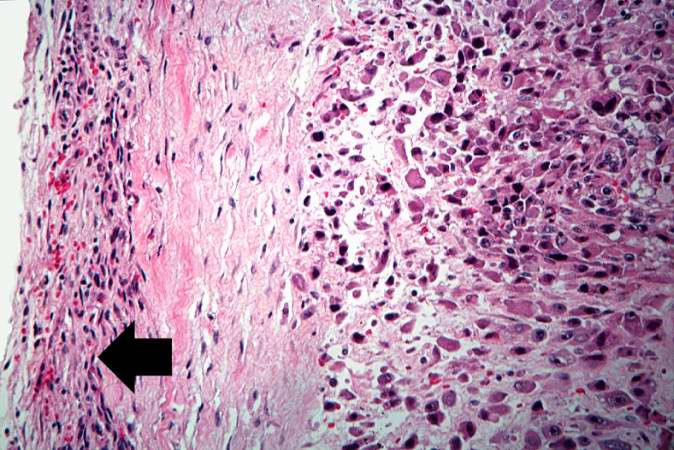
This high-power photomicrograph of the tumor demonstrates the fusiform morphology of the cells. Note the marked variability in size and staining intensity of the nuclei.
-
This is a high-power photomicrograph of the tumor demonstrating the anaplastic cell morphology.
-
This is a high-power photomicrograph of the tumor demonstrating the anaplastic cell morphology.
-
This is a high-power photomicrograph of the tumor demonstrating the anaplastic cell morphology and multiple mitotic figures (arrows).
References
- ↑ 1.0 1.1 Image courtesy of Dr Frank Gaillard. Radiopaedia (original file [1]). [http://radiopaedia.org/licence Creative Commons BY-SA-NC
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Osteosarcoma. Dr Yuranga Weerakkody◉ et al. Radiopaedia.org 2015. http://radiopaedia.org/articles/telangiectatic-osteosarcoma
- ↑ Wang LL. Biology of osteogenic sarcoma. Cancer J 11:294-305, 2005.
![Histology of conventional osteosarcoma[1]](/images/5/51/Osteosarcoma-conventional-histology_%281%29.jpg)