Osteosarcoma MRI: Difference between revisions
Jump to navigation
Jump to search
(→MRI) |
|||
| (7 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{CMG}};{{AE}} | {{CMG}}; {{AE}}[[User:DrMars|Mohammadmain Rezazadehsaatlou[2]]]. | ||
{{Osteosarcoma}} | {{Osteosarcoma}} | ||
==Overview== | ==Overview== | ||
On MRI, osteosarcoma is characterized by intermediate intensity of soft tissue and low signal intensity of ossified components on T1. High signal intensity of soft tissue and low signal intensity of [[ossified]] components on T2. Considerable contrast enhancement of solid components on T1 contrast. | On [[Magnetic resonance imaging|MRI]], [[osteosarcoma]] is characterized by intermediate intensity of soft tissue and low signal intensity of ossified components on [[T1]]. High signal intensity of soft tissue and low signal intensity of [[ossified]] components on [[MRI|T2]]. Considerable contrast enhancement of solid components on [[T1]] contrast. | ||
==MRI== | ==MRI== | ||
*MRI is proving essential in accurate local staging and assessment for limb sparing resection, particularly for evaluation of [[intraosseous]] tumor extension and soft-tissue involvement. | *[[Magnetic resonance imaging|MRI]] is proving essential in accurate local staging and assessment for limb sparing resection, particularly for evaluation of [[intraosseous]] tumor extension and soft-tissue involvement. | ||
*Assessment of the [[growth plate]] is also essential as up to 75-88% of [[Metaphyseal dysplasia|metaphyseal tumors]] do cross the [[growth plate]] into the [[epiphysis]]. | *Assessment of the [[growth plate]] is also essential as up to 75-88% of [[Metaphyseal dysplasia|metaphyseal tumors]] do cross the [[growth plate]] into the [[epiphysis]]. | ||
*MRI is used to: | *[[Magnetic resonance imaging|MRI]] is used to:<ref name="pmid28808701">{{cite journal |vauthors=Sue M, Oda T, Sasaki Y, Kameta A, Okada Y, Ogura I |title=Osteosarcoma of the Mandible: a Case Report with CT, MRI and Scintigraphy |journal=Chin J Dent Res |volume=20 |issue=3 |pages=169–172 |date=2017 |pmid=28808701 |doi=10.3290/j.cjdr.a38772 |url=}}</ref><ref name="pmid27229874">{{cite journal |vauthors=Kubo T, Furuta T, Johan MP, Adachi N, Ochi M |title=Percent slope analysis of dynamic magnetic resonance imaging for assessment of chemotherapy response of osteosarcoma or Ewing sarcoma: systematic review and meta-analysis |journal=Skeletal Radiol. |volume=45 |issue=9 |pages=1235–42 |date=September 2016 |pmid=27229874 |doi=10.1007/s00256-016-2410-y |url=}}</ref><ref name="pmid29117758">{{cite journal |vauthors=Kasalak Ö, Overbosch J, Glaudemans AWJM, Boellaard R, Jutte PC, Kwee TC |title=Primary tumor volume measurements in Ewing sarcoma: MRI inter- and intraobserver variability and comparison with FDG-PET |journal=Acta Oncol |volume=57 |issue=4 |pages=534–540 |date=April 2018 |pmid=29117758 |doi=10.1080/0284186X.2017.1398411 |url=}}</ref><ref name="pmid28806574">{{cite journal |vauthors=Degnan AJ, Chung CY, Shah AJ |title=Quantitative diffusion-weighted magnetic resonance imaging assessment of chemotherapy treatment response of pediatric osteosarcoma and Ewing sarcoma malignant bone tumors |journal=Clin Imaging |volume=47 |issue= |pages=9–13 |date=2018 |pmid=28806574 |doi=10.1016/j.clinimag.2017.08.003 |url=}}</ref><ref name="pmid24247589">{{cite journal |vauthors=Uchiyama Y, Matsumoto K, Murakami S, Kanesaki T, Matsumoto A, Kishino M, Furukawa S |title=MRI in a case of osteosarcoma in the temporomandibular joint |journal=Dentomaxillofac Radiol |volume=43 |issue=2 |pages=20130280 |date=2014 |pmid=24247589 |pmc=4064616 |doi=10.1259/dmfr.20130280 |url=}}</ref><ref name="pmid26385785">{{cite journal |vauthors=Wakabayashi H, Saito J, Taki J, Hashimoto N, Tsuchiya H, Gabata T, Kinuya S |title=Triple-phase contrast-enhanced MRI for the prediction of preoperative chemotherapeutic effect in patients with osteosarcoma: comparison with (99m)Tc-MIBI scintigraphy |journal=Skeletal Radiol. |volume=45 |issue=1 |pages=87–95 |date=January 2016 |pmid=26385785 |doi=10.1007/s00256-015-2250-1 |url=}}</ref> | ||
:*Show how far a bone [[tumor]] has grown inside a bone. | :*Show how far a bone [[tumor]] has grown inside a bone. | ||
:*Show how much a bone [[tumor]] has grown outside the bone. | :*Show how much a bone [[tumor]] has grown outside the bone. | ||
:*Observe if a [[tumor]] has grown into [[blood vessels]], [[nerves]], [[bone marrow]] or other nearby tissues or structures. | :*Observe if a [[tumor]] has grown into [[blood vessels]], [[nerves]], [[bone marrow]] or other nearby tissues or structures. | ||
:*Determine if the tumor has developed in one or more sites within the same bone (skip metastases). | :*Determine if the tumor has developed in one or more sites within the same bone (skip [[metastases]]). | ||
:*Plan for possible surgery. | :*Plan for possible surgery. | ||
On MRI, signal characteristics of osteosarcoma include: | On [[Magnetic resonance imaging|MRI]], signal characteristics of [[osteosarcoma]] include: | ||
*'''T1''': | *'''T1''': | ||
:*Soft tissue, non-mineralized component: intermediate signal intensity. | :*Soft tissue, non-mineralized component: intermediate signal intensity. | ||
:*Mineralized/[[ossified]] components: low signal intensity. | :*Mineralized/[[ossified]] components: low signal intensity. | ||
:* | :*Peritumoral edema: intermediate signal intensity. | ||
:*Scattered regions of [[hemorrhage]] will have variable signal. | :*Scattered regions of [[hemorrhage]] will have variable signal. | ||
*'''T2''': | *'''T2''': | ||
| Line 32: | Line 34: | ||
<gallery perrow="3"> | <gallery perrow="3"> | ||
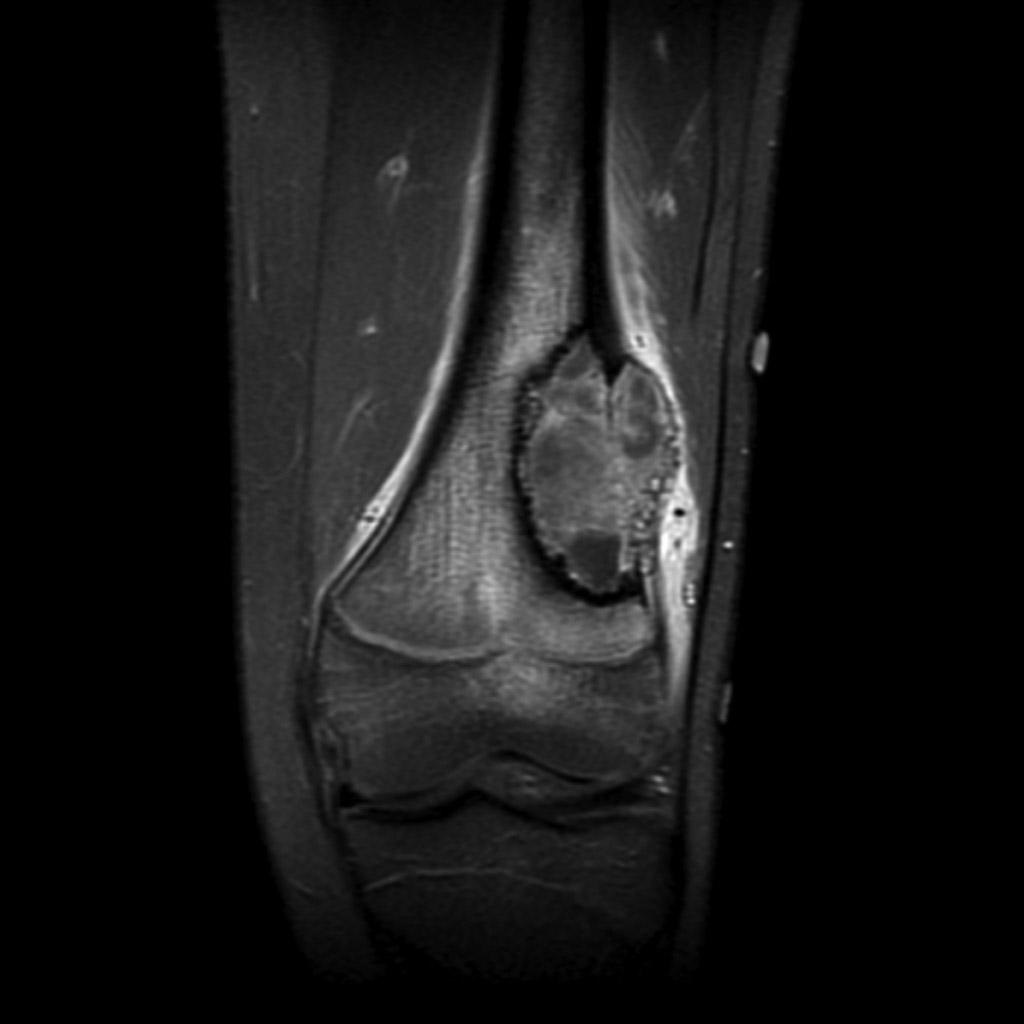
File:Osteosarcoma-distal-femur | File:Osteosarcoma-distal-femur (1).jpg|Coronal T1 | ||
File:Osteosarcoma | File:Osteosarcoma-distal-femur (2).jpg|Coronal T1 C+ fat sat | ||
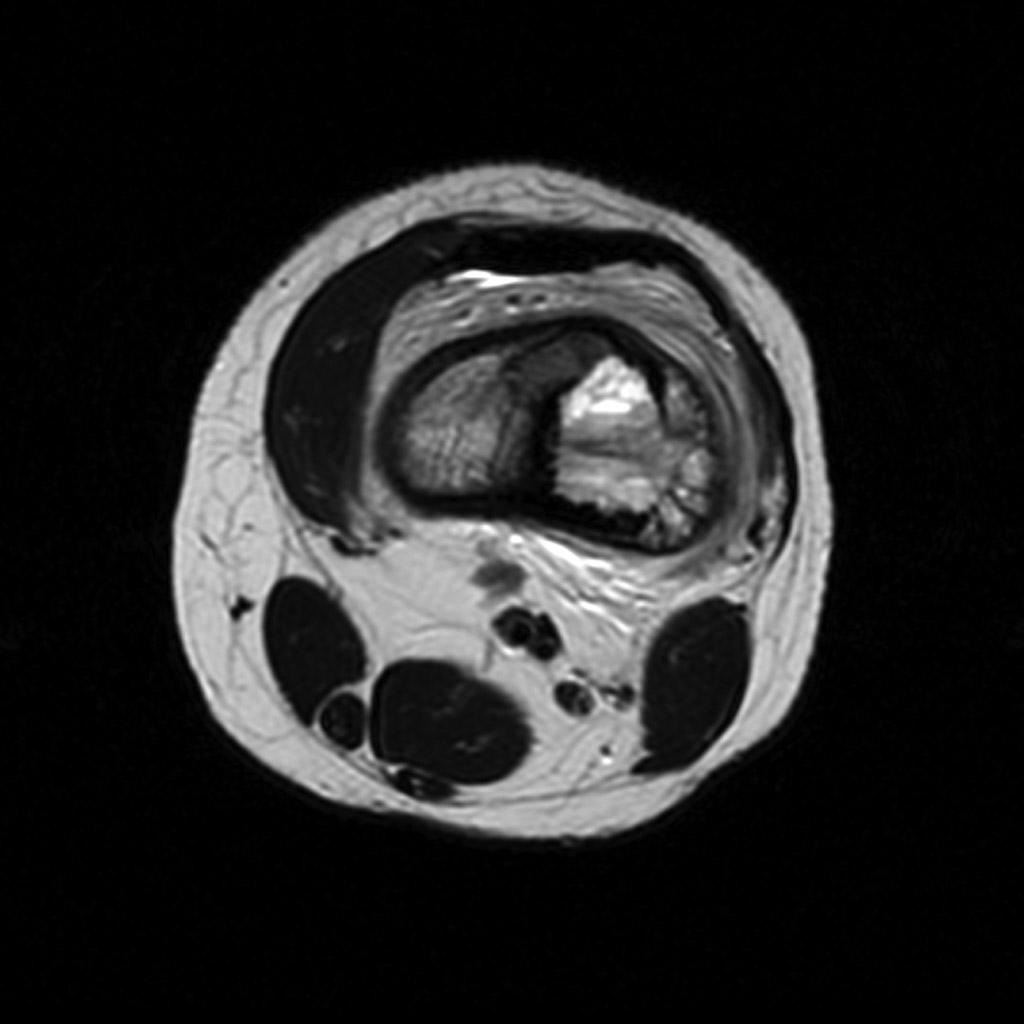
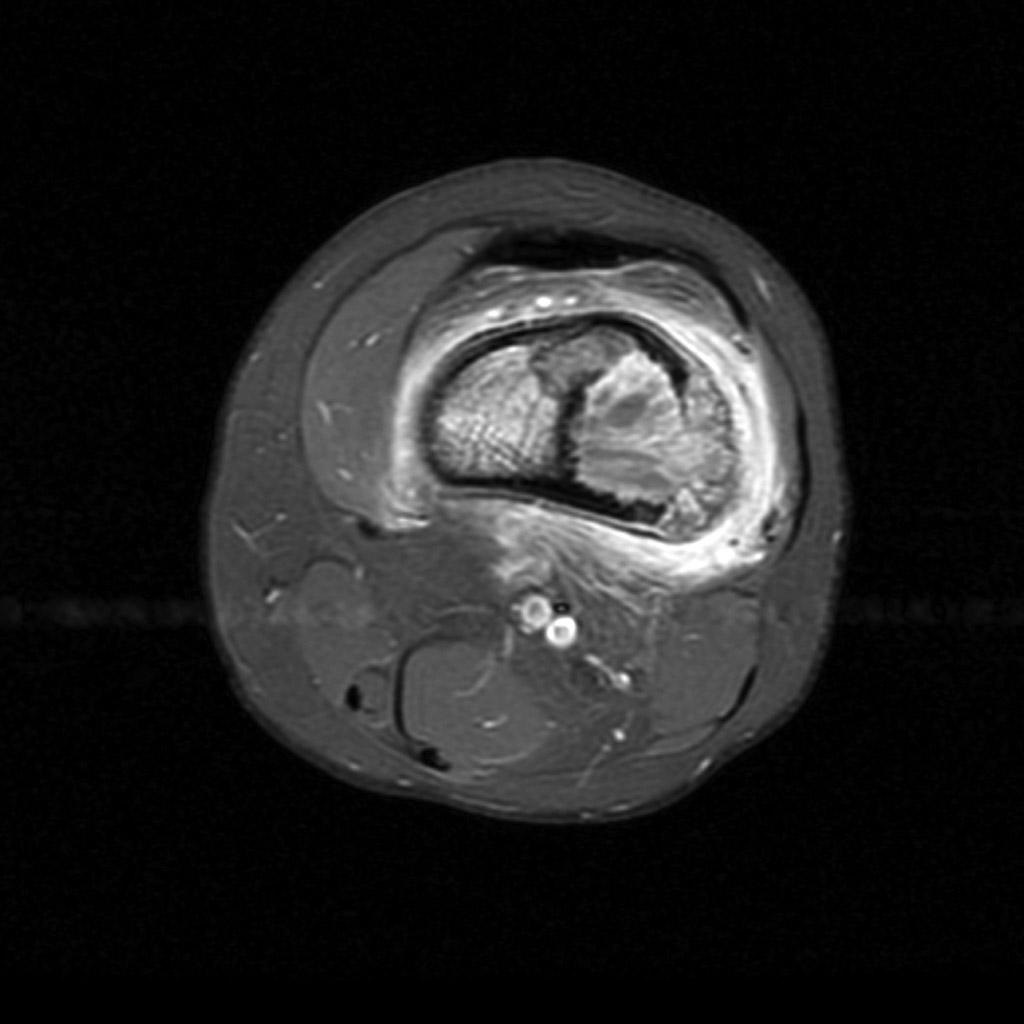
File:Osteosarcoma-distal-femur | File:Osteosarcoma-distal-femur (3).jpg|Axial T2 | ||
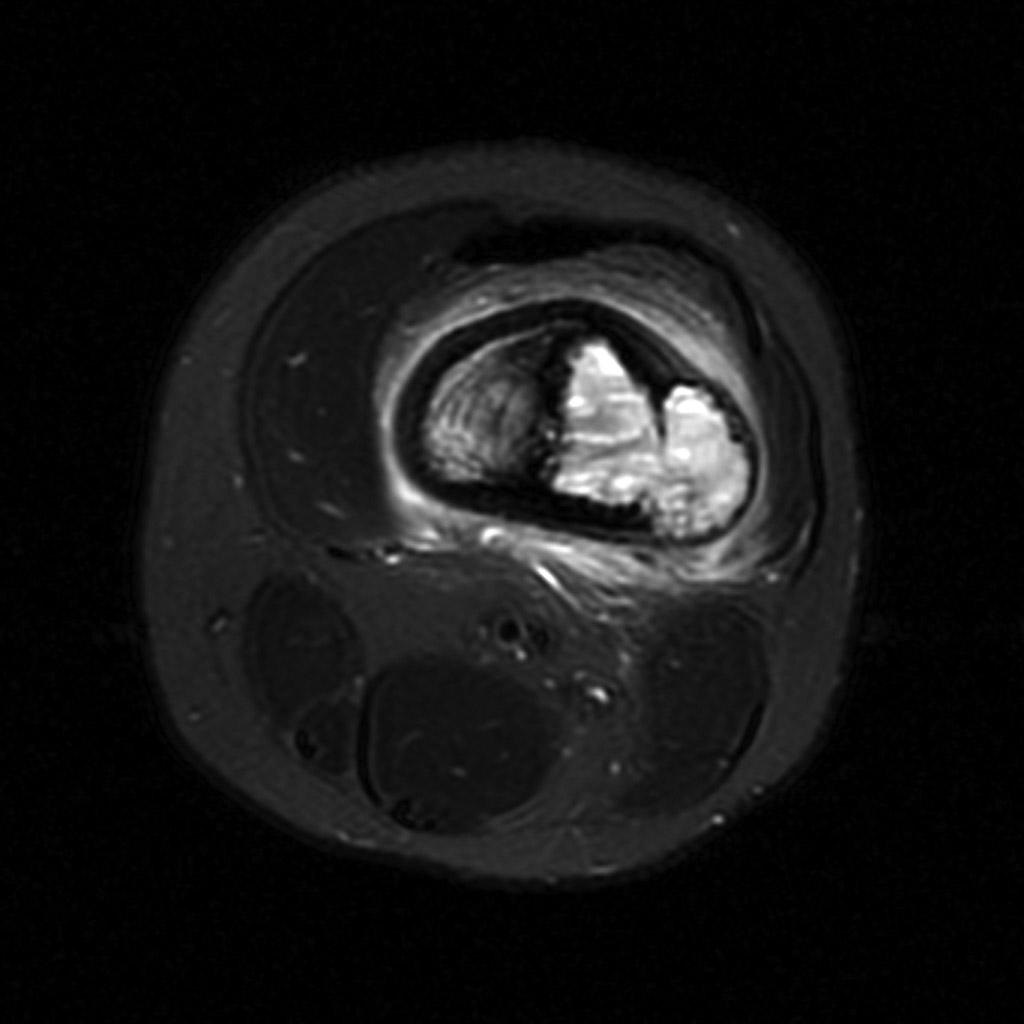
File:Osteosarcoma-distal-femur (4).jpg|Axial T2 fat sat | |||
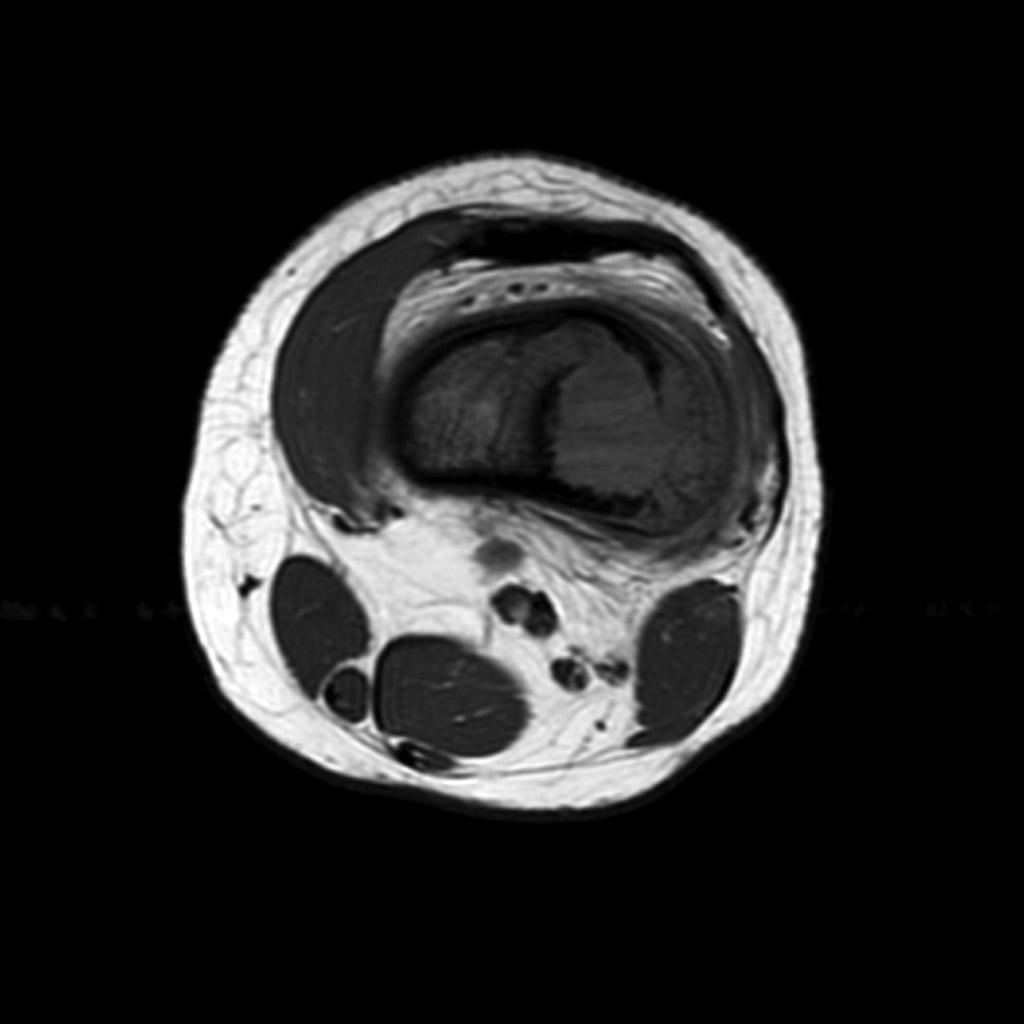
File:Osteosarcoma-distal-femur (5).jpg|Axial T1 | |||
File:Osteosarcoma-distal-femur (6).jpg|Axial T1 C+ fat sat | |||
</gallery> | </gallery> | ||
*The following table illustrates the findings on MRI for the subtypes of osteosarcoma: | *The following table illustrates the findings on MRI for the subtypes of osteosarcoma: | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px; width: 1000px" align="center" | ||
| valign="top" | | | valign="top" | | ||
Latest revision as of 13:33, 17 October 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mohammadmain Rezazadehsaatlou[2].
|
Osteosarcoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Osteosarcoma MRI On the Web |
|
American Roentgen Ray Society Images of Osteosarcoma MRI |
Overview
On MRI, osteosarcoma is characterized by intermediate intensity of soft tissue and low signal intensity of ossified components on T1. High signal intensity of soft tissue and low signal intensity of ossified components on T2. Considerable contrast enhancement of solid components on T1 contrast.
MRI
- MRI is proving essential in accurate local staging and assessment for limb sparing resection, particularly for evaluation of intraosseous tumor extension and soft-tissue involvement.
- Assessment of the growth plate is also essential as up to 75-88% of metaphyseal tumors do cross the growth plate into the epiphysis.
- MRI is used to:[1][2][3][4][5][6]
- Show how far a bone tumor has grown inside a bone.
- Show how much a bone tumor has grown outside the bone.
- Observe if a tumor has grown into blood vessels, nerves, bone marrow or other nearby tissues or structures.
- Determine if the tumor has developed in one or more sites within the same bone (skip metastases).
- Plan for possible surgery.
On MRI, signal characteristics of osteosarcoma include:
- T1:
- Soft tissue, non-mineralized component: intermediate signal intensity.
- Mineralized/ossified components: low signal intensity.
- Peritumoral edema: intermediate signal intensity.
- Scattered regions of hemorrhage will have variable signal.
- T2:
- T1 C+ (Gd):
- Solid components show considerable enhancement.
-
Coronal T1
-
Coronal T1 C+ fat sat
-
Axial T2
-
Axial T2 fat sat
-
Axial T1
-
Axial T1 C+ fat sat
- The following table illustrates the findings on MRI for the subtypes of osteosarcoma:
| Subtype | MRI findings |
|---|---|
|
|
|
|
|
|
|
|
|
|
References
- ↑ Sue M, Oda T, Sasaki Y, Kameta A, Okada Y, Ogura I (2017). "Osteosarcoma of the Mandible: a Case Report with CT, MRI and Scintigraphy". Chin J Dent Res. 20 (3): 169–172. doi:10.3290/j.cjdr.a38772. PMID 28808701.
- ↑ Kubo T, Furuta T, Johan MP, Adachi N, Ochi M (September 2016). "Percent slope analysis of dynamic magnetic resonance imaging for assessment of chemotherapy response of osteosarcoma or Ewing sarcoma: systematic review and meta-analysis". Skeletal Radiol. 45 (9): 1235–42. doi:10.1007/s00256-016-2410-y. PMID 27229874.
- ↑ Kasalak Ö, Overbosch J, Glaudemans A, Boellaard R, Jutte PC, Kwee TC (April 2018). "Primary tumor volume measurements in Ewing sarcoma: MRI inter- and intraobserver variability and comparison with FDG-PET". Acta Oncol. 57 (4): 534–540. doi:10.1080/0284186X.2017.1398411. PMID 29117758. Vancouver style error: initials (help)
- ↑ Degnan AJ, Chung CY, Shah AJ (2018). "Quantitative diffusion-weighted magnetic resonance imaging assessment of chemotherapy treatment response of pediatric osteosarcoma and Ewing sarcoma malignant bone tumors". Clin Imaging. 47: 9–13. doi:10.1016/j.clinimag.2017.08.003. PMID 28806574.
- ↑ Uchiyama Y, Matsumoto K, Murakami S, Kanesaki T, Matsumoto A, Kishino M, Furukawa S (2014). "MRI in a case of osteosarcoma in the temporomandibular joint". Dentomaxillofac Radiol. 43 (2): 20130280. doi:10.1259/dmfr.20130280. PMC 4064616. PMID 24247589.
- ↑ Wakabayashi H, Saito J, Taki J, Hashimoto N, Tsuchiya H, Gabata T, Kinuya S (January 2016). "Triple-phase contrast-enhanced MRI for the prediction of preoperative chemotherapeutic effect in patients with osteosarcoma: comparison with (99m)Tc-MIBI scintigraphy". Skeletal Radiol. 45 (1): 87–95. doi:10.1007/s00256-015-2250-1. PMID 26385785.