Ornithine transcarbamylase deficiency
[[For patient information, click here
| Ornithine transcarbamylase deficiency | |
 | |
|---|---|
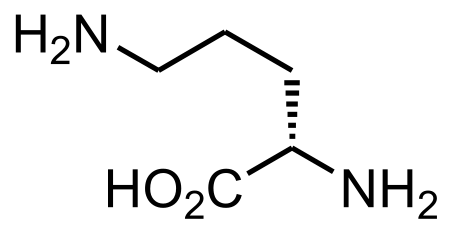
| Ornithine | |
| ICD-9 | 270.6 |
| OMIM | 311250 |
| DiseasesDB | 9286 |
| MedlinePlus | 000372 |
| eMedicine | ped/2744 |
| MeSH | D020163 |
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Ornithine transcarbamylase deficiency (OTCD), the most common of the urea cycle disorders, is a rare metabolic disorder, occurring in one out of every 80,000 births. OTC is a genetic disorder resulting in a mutated and ineffective form of the enzyme ornithine transcarbamylase.
Symptoms
Like other urea cycle disorders, OTC affects the body's ability to get rid of ammonia, a toxic breakdown product of the body's use of protein. As a result, ammonia accumulates in the blood causing hyperammonemia. This ammonia travels to the various organs of the body including the brain, causing coma, brain damage and death.
Another symptom of OTC is a buildup of orotic acid in the blood. This is due to an anaplerism that occurs with carbamoyl phosphate entering the pyrimidine synthesis pathway.
Ornithine transcarbamylase deficiency often becomes evident in the first few days of life. An infant with ornithine transcarbamylase deficiency may be lacking in energy (lethargic) or unwilling to eat, and have poorly-controlled breathing rate or body temperature. Some babies with this disorder may experience seizures or unusual body movements, or go into a coma. Complications from ornithine transcarbamylase deficiency may include developmental delay and mental retardation. Progressive liver damage, skin lesions, and brittle hair may also be seen. Other symptoms include irrational behavior (caused by encephalitis), mood swings, and poor performance in school.
In some affected individuals, signs and symptoms of ornithine transcarbamylase may be less severe, and may not appear until later in life. Some female carriers become symptomatic later in life. This can happen as a result of anorexia, starvation, malnutrition, or even (in at least one case) as a result of gastric bypass surgery. It is also possible for symptoms to be exacerbated by extreme trauma of many sorts, including, (at least in one case) adolescent pregnancy coupled with severe stomach flu.
Genetics
Mutations in the OTC gene cause ornithine transcarbamylase deficiency. Ornithine transcarbamylase deficiency belongs to a class of genetic diseases called urea cycle disorders. The urea cycle is a sequence of reactions that occurs in liver cells. It processes excess nitrogen, generated when protein is used by the body, to make a compound called urea that is excreted by the kidneys.
In ornithine transcarbamylase deficiency, the enzyme that starts a specific reaction within the urea cycle is damaged or missing. The urea cycle cannot proceed normally, and nitrogen accumulates in the bloodstream in the form of ammonia. Ammonia is especially damaging to the nervous system, so ornithine transcarbamylase deficiency causes neurological problems as well as eventual damage to the liver.
Ornithine transcarbamylase deficiency is an X-linked disorder caused by a number of different mutations. Since the gene is on the X chromosome, females are primarily carriers while males with nonconservative mutations rarely survive past 72 hours of birth. Half of those survivors die in the first month, and half of the remaining by age 5.
Treatment
Treatment includes a low-protein formula called keto-acid and sodium benzoate, a preservative, and another type of sodium, which binds to ammonia and helps eliminate it from the body. Some treatment includes a protein limited diet combined with a dietary supplement including arginine.
In cases of OTC where enzyme production is low or non-existent, treatment consisting of low-protein diet and dietary supplementation are inadequate. In these cases, liver transplant is a treatment option.
Reference
- National Library of Medicine Ornithine transcarbamylase deficiency