Optic nerve glioma differential diagnosis: Difference between revisions
Aditya Ganti (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| Line 39: | Line 39: | ||
<br /> | <br /> | ||
{| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align="center" | {| style="border: 0px; font-size: 90%; margin: 3px; width: 800px;" align="center" | ||
| valign="top" | | | valign="top" | | ||
Latest revision as of 04:23, 20 September 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Simrat Sarai, M.D. [2]
Overview
Optic nerve glioma must be differentiated from other diseases that cause optic nerve enlargement such as optic nerve sheath meningioma, orbital pseudotumor, optic neuritis, orbital lymphomas, metastasis, fibrous dysplasia, paranasal mucocele, rhabdomyosarcoma, neurofibromatosis, perioptic haemorrhage, Erdheim-Chester disease, juvenile xanthogranuloma, medulloepithelioma, retinoblastoma, Krabbe disease, optic nerve and chiasm glioma such as germinoma and sarcoidosis, and optic chiasm glioma extending into the hypothalamus such as pituitary adenoma, craniopharyngioma, malignant astrocytoma, dermoid cyst, chordoma, colloid cyst, histiocytosis X, tuberculous granuloma, and hemangloendothelioma.[1]
Differentiating Optic nerve glioma from other diseases
- The major differential diagnostic considerations when an enlarged optic nerve is identified on imaging are
- inflammatory (neuritis, infection, or pseudotumor)
- Neoplastic,
- Result of increased intracranial pressure.
- Distinguishing inflammatory from neoplastic processes of the nerves is difficult because both may demonstrate optic-nerve enlargement with or without contrast enhancement.
- Clinical history can then be used to determine the underlying cause.
- Unilateral involvement, no pain on extra-ocular movement, no systemic inflammatory signs at around the onset of visual loss, no additional white-matter abnormality or recurrent visual symptoms during follow-up period might support a diagnosis of optic-nerve glioma rather than optic neuritis in childhood.
- Other tumorous conditions such as lymphoma or inflammatory pseudo-tumor may be ruled in the absence of a history of painful ophthalmoplegia or a rapid deterioration of symptoms during follow-up.
| Differentiating Optic nerve glioma from other diseases | |
|---|---|
| Optic nerve glioma |
|
| Optic nerve and chiasm glioma |
|
| Optic chiasm glioma extending into the hypothalamus |
|
| Disease/Condition | Clinical presentation | Demographics/History | Diagnosis | Other notes |
|---|---|---|---|---|
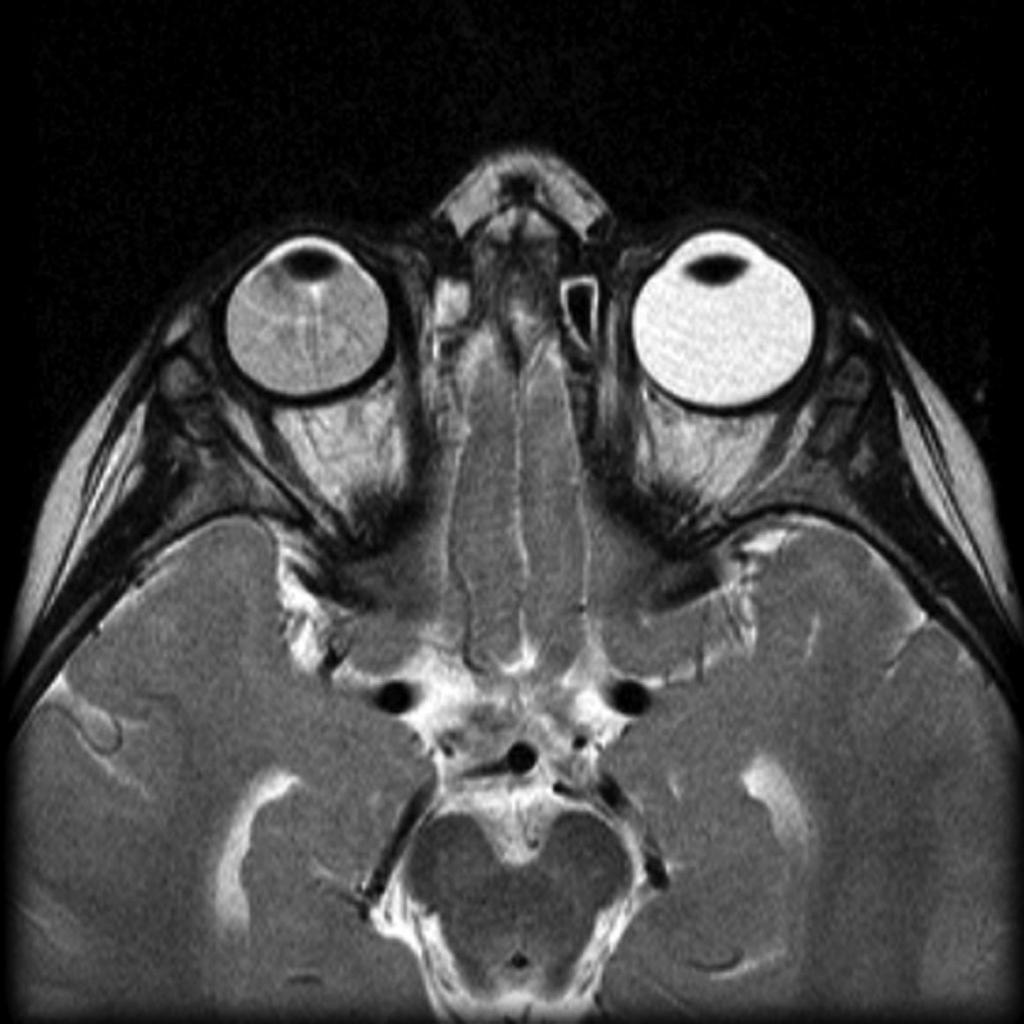
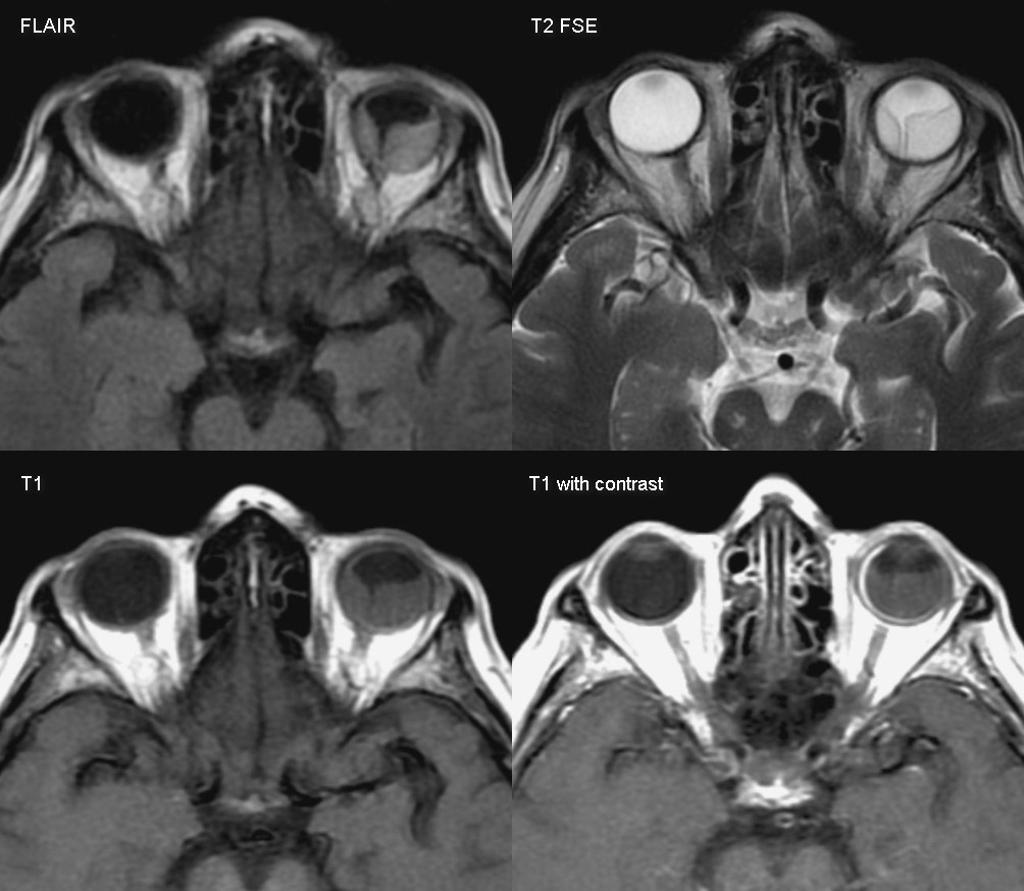
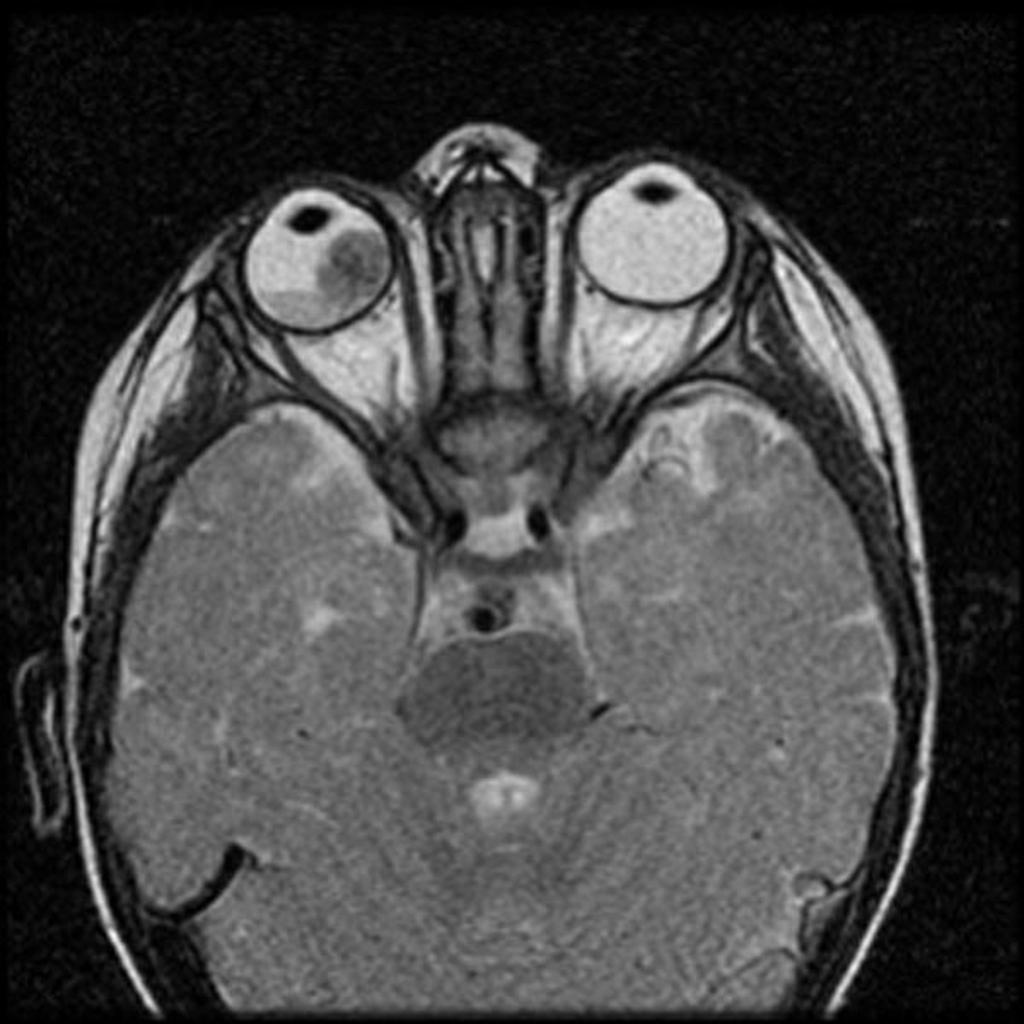
| Retinoblastoma[2][3] |
|
|
| |
| Coats'disease[4][5] |
|
|
| |
| Persistent fetal vasculature (formerly known as persistent hyperplastic primary vitreous)[5] |
|
|
|
|
| Astrocytic hamartoma[6] |
|
|
|
|
| Retinopathy of prematurity (ROP)[6] |
|
|
|
|
| Ocular toxocariasis [6] |
|
| ||
| Familial Exudative Vitreoretinopathy (FEVR)[7] |
|
|
|
|
| Norrie’s Disease[6][8] |
|
|
- | |
| Coloboma[6] |
|
|
|
 |
 |
 |
 |
|---|
References
- ↑ Optic nerve glioma. Radiopedia(2015) http://radiopaedia.org/articles/optic-nerve-glioma Accessed on October 2 2015
- ↑ Butros LJ, Abramson DH, Dunkel IJ (March 2002). "Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences". Pediatrics. 109 (3): E45. PMID 11875173.
- ↑ Sachdeva R, Schoenfield L, Marcotty A, Singh AD (June 2011). "Retinoblastoma with autoinfarction presenting as orbital cellulitis". J AAPOS. 15 (3): 302–4. doi:10.1016/j.jaapos.2011.02.013. PMID 21680213.
- ↑ Silva RA, Dubovy SR, Fernandes CE, Hess DJ, Murray TG (December 2011). "Retinoblastoma with Coats' response". Ophthalmic Surg Lasers Imaging. 42 Online: e139–43. doi:10.3928/15428877-20111208-04. PMID 22165951.
- ↑ 5.0 5.1 Gupta N, Beri S, D'souza P (June 2009). "Cholesterolosis Bulbi of the Anterior Chamber in Coats Disease". J Pediatr Ophthalmol Strabismus. doi:10.3928/01913913-20090616-04. PMID 19645389.
- ↑ 6.0 6.1 6.2 6.3 6.4 Singh, Arun (2015). Clinical ophthalmic oncology : retinoblastoma. Heidelberg: Springer. ISBN 978-3-662-43451-2.
- ↑ Gerstenblith, Adam (2012). The Wills eye manual : office and emergency room diagnosis and treatment of eye disease. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. ISBN 978-1451109382.
- ↑ Howard GM, Ellsworth RM (October 1965). "Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma". Am. J. Ophthalmol. 60 (4): 610–8. PMID 5897773.