Nutcracker esophagus other diagnostic studies
|
Nutcracker esophagus Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Nutcracker esophagus other diagnostic studies On the Web |
|
American Roentgen Ray Society Images of Nutcracker esophagus other diagnostic studies |
|
Risk calculators and risk factors for Nutcracker esophagus other diagnostic studies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Other Diagnostic Studies
Esophageal Motility Studies
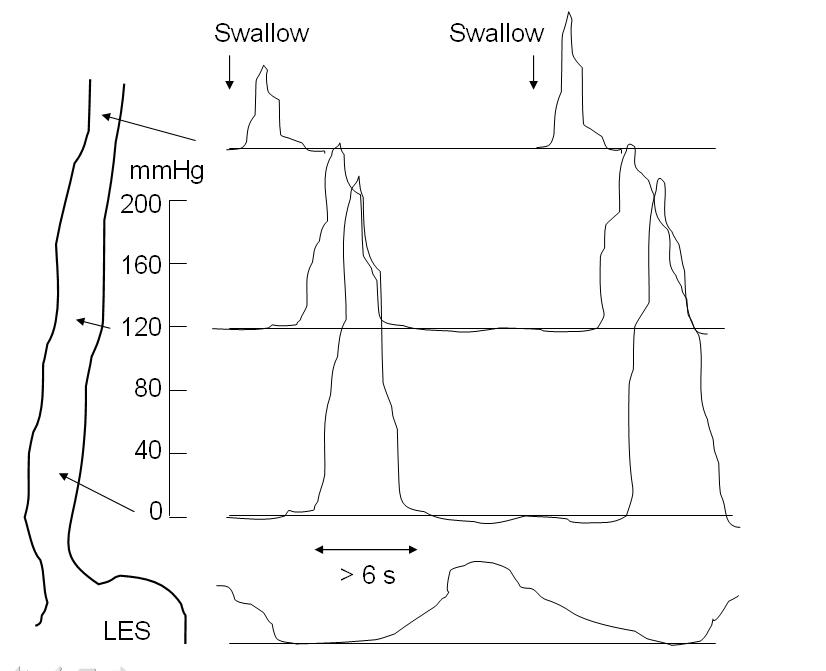
The diagnosis of nutcracker esophagus is typically made with an esophageal motility study, which shows characteristic features of the disorder. Esophageal motility studies involve pressure measurements of the esophagus after a patient takes a wet (fluid-containing) or dry (food-containing) swallow. Measurements are usually taken at various points in the esophagus.[1]
Nutcracker esophagus is characterized by a number of criteria described in the literature. The most commonly used criteria are the Castell criteria, named after American gastroenterologist D.O. Castell. The Castell criteria include one major criterion: a mean peristaltic amplitude in the distal esophagus of more than 180 mm Hg. The minor criterion is the presence of repetitive contractions (meaning 2 or more) that are greater than six seconds in duration. Castell also noted that the lower esophageal sphincter relaxes normally in nutcracker esophagus, but has an elevated pressure of greater than 40 mm Hg at baseline.[2] [1] [3][4]
Three other criteria for definition of the nutcracker esophagus have been defined. The Gothenburg criterion consists of the presence of peristaltic contractions, with an amplitude of 180 mm Hg at any place in the esophagus.[5][4] The Richter criterion involves the presence of peristaltic contractions with an amplitude of greater than 180 mmHg from an average of measurements taken 3 and 8 centimeters above the lower esophageal sphincter.[6] It has been incorporated into a number of clinical guidelines for the evaluation of dysphagia.[4] The Achem criteria are more stringent criteria that are an extension of the study of 93 patients used by Richter and Castell in the development of their criteria, and require amplitudes of greater than 199 mm Hg at 3 cm above the lower esophageal sphincter (LES), greater than 172 mm Hg at 8 cm above the LES, or greater than 102 mm Hg at 13 cm above the LES.[4][7]
References
- ↑ 1.0 1.1 Cockeram A (1998). "Canadian Association of Gastroenterology Practice Guidelines: evaluation of dysphagia". Can J Gastroenterol. 12 (6): 409–13. PMID 9784896.
- ↑ Tutuian R, Castell D (2006). "Esophageal motility disorders (distal esophageal spasm, nutcracker esophagus, and hypertensive lower esophageal sphincter): modern management". Curr Treat Options Gastroenterol. 9 (4): 283–94. PMID 16836947.
- ↑ Ott D (1994). "Motility disorders of the esophagus". Radiol Clin North Am. 32 (6): 1117–34. PMID 7972703.
- ↑ 4.0 4.1 4.2 4.3 Pilhall M, Börjesson M, Rolny P, Mannheimer C (2002). "Diagnosis of nutcracker esophagus, segmental or diffuse hypertensive patterns, and clinical characteristics". Dig Dis Sci. 47 (6): 1381–8. PMID 12064816.
- ↑ Fang J, Bjorkman D (2002). "Nutcracker esophagus: GERD or an esophageal motility disorder". Am J Gastroenterol. 97 (6): 1556–7. PMID 12094884.
- ↑ Richter J, Wu W, Johns D, Blackwell J, Nelson J, Castell J, Castell D (1987). "Esophageal manometry in 95 healthy adult volunteers. Variability of pressures with age and frequency of "abnormal" contractions". Dig Dis Sci. 32 (6): 583–92. PMID 3568945.
- ↑ Achem S, Kolts B, Burton L (1993). "Segmental versus diffuse nutcracker esophagus: an intermittent motility pattern". Am J Gastroenterol. 88 (6): 847–51. PMID 8503378.