Normal pressure hydrocephalus
| Normal pressure hydrocephalus | |
| ICD-10 | G91.2 |
|---|---|
| ICD-9 | 331.9 |
| DiseasesDB | 9089 |
| MedlinePlus | 000752 |
| eMedicine | neuro/277 radio/479 |
| MeSH | D006850 |
Normal pressure hydrocephalus (NPH) is a chronic type of communicating hydrocephalus whereby the increase in intracranial pressure (ICP) due to accumulation of cerebrospinal fluid (CSF) becomes stable and that the formation of CSF equilibrates with absorption. The ICP gradually falls but still maintains a slightly elevated level and the CSF pressure reaches a high normal level of 150 to 200 mmH2O. Because of this equilibration, patients do not exhibit the classic signs of increased intracranial pressure such as headache, nausea, vomiting, or altered consciousness. It is often misdiagnosed as Parkinson's disease, Alzheimer's disease, and senility due to its chronic nature and its presenting symptoms [see below].
Clinical manifestations
NPH may exhibit the classic triad of urinary incontinence, wide-based ataxic gait, and dementia(commonly referred to as "wet, wobbly and wacky").
- Gait disturbance and Ataxia is the first symptom of the triad and may be progressive, due to expansion of the ventricular system, particularly at the level of the lateral ventricles, leading to traction on the lumbosacral motor fibers that run in this region. Often, this takes on the form of unsteadiness and impaired balance, especially on stairs and curbs. Weakness and tiredness may also be part of the complaint, although this is very vague. NPH gait disturbance is often characterized as a "magnetic gait," in which feet appear to be stuck to the walking surface until wrested upward and forward at each step. The gait may mimic a Parkinsonian gait, with short shuffling steps and stooped, forward-leaning posture, but there is no rigidity or tremor. A broad-based gait may be employed by the patient in order to compensate for the ataxia.
- Dementia is predominantly frontal lobe in nature, with apathy, dullness in thinking, and slight inattention. Memory problems are usually the main problem, which can lead to the misdiagnosis of Alzheimer's disease. However, in NPH there may be an obvious discrepancy between (often severely) impaired recall and intact or much less impaired recognition. The dementia is thought to result from traction on frontal and limbic fibers that also run in the periventricular region.
- Urinary incontinence appears late in the illness, consisting of increased frequency and urgency. Ultimately, the patient may exhibit "frontal lobe incontinence," where he becomes indifferent to his recurrent urinary symptoms.
Diagnosis
Diagnosis of NPH is usually first led by a lumbar puncture, followed by the evaluation of clinical response to removal of CSF. This can be followed by a CT, MRI, and continuous external lumbar CSF drainage during 3 or 4 days.
- Lumbar puncture is usually the first step in diagnosis and the opening pressure measured carefully. In most cases, CSF pressure is usually above 155 mmH2O. Clinical improvement after removal of CSF (30 mL or more) has a high predictive value for subsequent success with shunting. This is called the "lumbar tap test" or "Fisher test". A "negative" test has a very low predictive accuracy, as many patients may improve after a shunt in spite of lack of improvement after CSF removal.
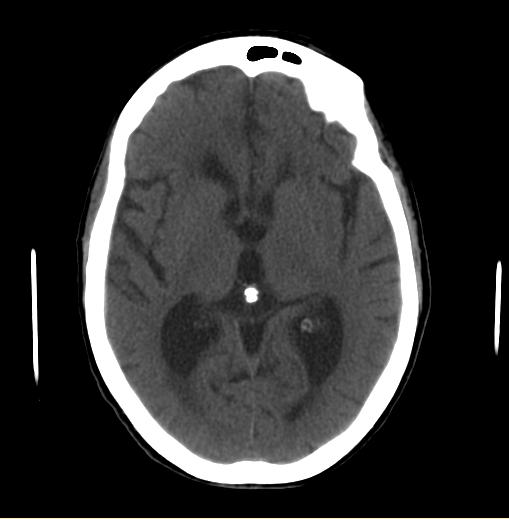
- CT scan may show enlarged ventricles without convolutional atrophy.
- MRI may show some degree of transependymal egress of water surrounding the ventricles.
CT and MRI displace communicating hydrocephalus.
Treatment
NPH may be relieved by surgically implanting a ventriculoperitoneal shunt to drain excess cerebrospinal fluid to the abdomen where it is absorbed. Once the shunt is in place, the ventricles diminish in size in 3 to 4 days, regardless of the duration of the hydrocephalus. Most patients who have continued success with such shunts usually only have two of the three triads (excluding incontinence).