Neuroma
|
WikiDoc Resources for Neuroma |
|
Articles |
|---|
|
Most recent articles on Neuroma |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Neuroma at Clinical Trials.gov Clinical Trials on Neuroma at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Neuroma
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Neuroma Risk calculators and risk factors for Neuroma
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Neuroma |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Synonyms and keywords: Traumatic neuroma; Morton neuroma; Joplin neuroma
Overview
Neuroma (Neuro- is from the Greek for nerve) is defined as a benign tumor of a nerve. However, neuroma commonly refers to any tumor of cells of the nervous system.[1] Neuromas form part of the peripheral nerve sheath tumors. Neuroma was first described by Thomas Morton in 1876. Neuromas may be classified according to histopathological features into 3 groups: Morton's neuroma, traumatic neuroma, and neoplasic neuromas. The pathogenesis of neuroma is characterized by neural degeneration with epineural and endoneural vascular hyalinization, and perineural fibrosis. Neuroma is more commonly observed among patients aged between 15 to 50 years old. Neuroma is more commonly observed among middle aged adults. Females are more commonly affected with neuroma than males. The female to male ratio is approximately 5:1. Common risk factors in the development of neuroma include improper footwear and high impact sports (e.g., rock-climbing, ballet dancing). A major complication of neuroma is chronic neuropathic pain. On ultrasound, neuroma is characterized as a well-defined, hypoechoic lesion located in the intermetatarsal space proximal to the metatarsal head. Patients with neuroma usually appear with antalgic posture. Physical examination may be remarkable for tenderness to palpation and dysesthetic pain. Surgical excision is the treatment of choice for patients with neuroma; this surgical intervention is associated with a relatively favorable success rate, approximately 80%. The recurrence rate after surgery is as high as 50%.
Historical Perspective
- Neuroma was first described by Thomas Morton in 1876.
Classification
- Neuroma may be classified according to histopathological features into 3 groups:[2]
- Morton neuroma
- Symptomatic perineural fibrosis around a plantar digital nerve of the foot
- Also known as Morton’s metatarsalgia
- Traumatic neuroma
- Arises from nerve injury (often as a result of surgery)
- They occur at the end of injured nerve fibers as a form of unregulated nerve regeneration
- Subtype of traumatic neuroma, called "Joplin neuroma" (a compression traumatic neuroma)
- Occurs most commonly near a scar
- Often very painful
- Neoplasic neuroma
- Solid nodular mass
- Usually, separate from nerve fibers
Pathophysiology
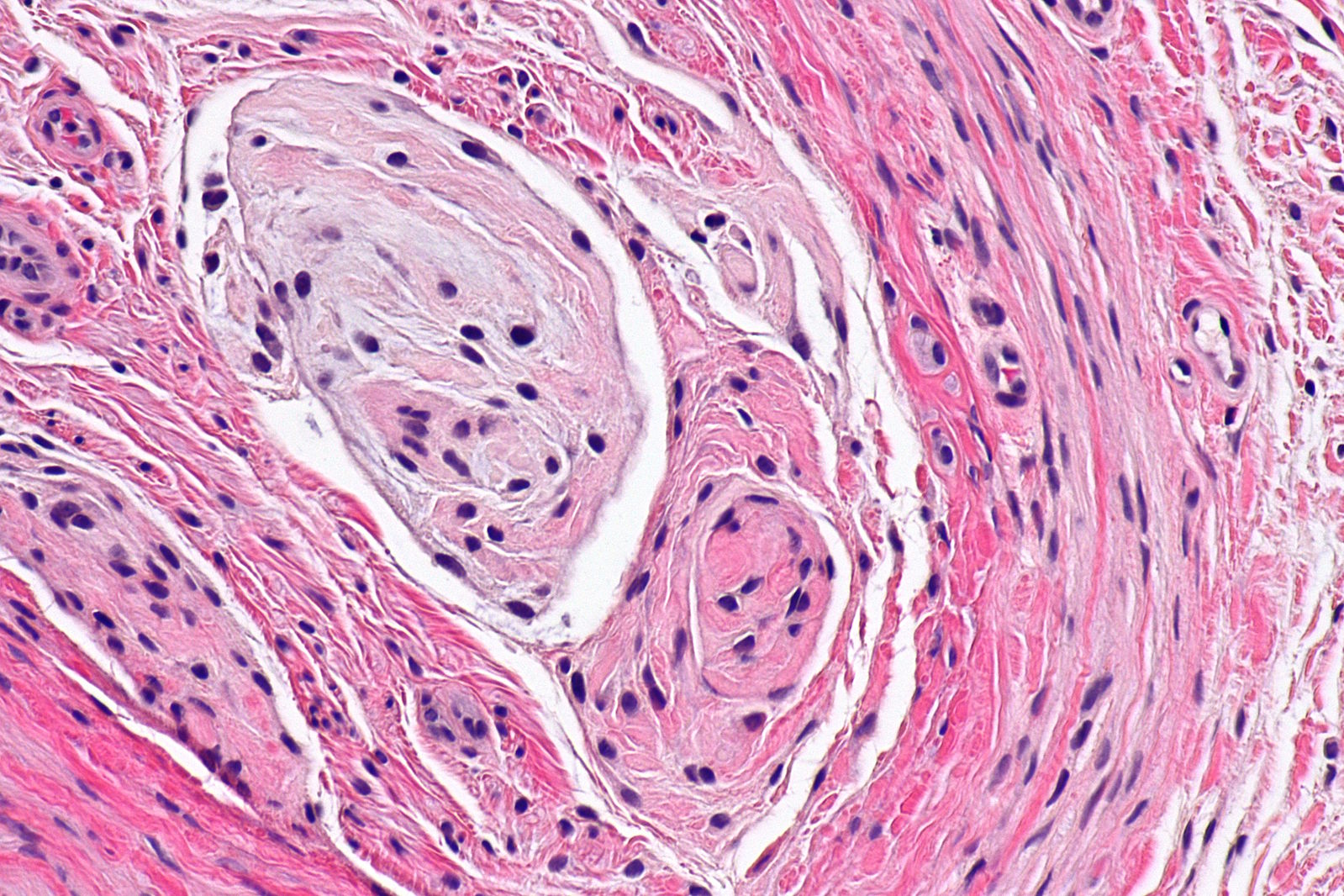
- The pathogenesis of neuroma is characterized by neural degeneration with epineural and endoneural vascular hyalinization, and perineural fibrosis.[2]
- The pathogenesis of traumatic neuroma is characterized by a chronic reactive fibroinflammatory disorganized regeneration around a nerve after an injury (such as traction injury or chronic repetitive stress).
- Morton neuroma is characterized by being located in the 3rd web-space, between 3rd and 4th metatarsal heads.
- Another subtype of traumatic neuroma is terminal neuroma (also known as "stump neuroma") which can occur after transection of the nerve (e.g. limb amputation).
- The are no genetic mutations associated with the development of neuroma.
- On gross pathology, characteristic findings of neuroma, include:[3][4]
- Adherent fibrofatty tissue
- Yellowish small mass
- Extensive fibrosis around and within the nerve
- Digital artery
- Thrombosis
- Arterial thickening
- The image below demonstrates microscopic histopathological analysis of traumatic neuroma:
-
Traumatic neuroma. Courtesy of Libre Pathology
Causes
- Indirect nerve trauma
- Traction injury
- Chronic repetitive stress
Differentiating Neuroma from other Diseases
- Neuroma must be differentiated from other diseases that cause forefoot pain and numbness such as:[2][4]
- Stress fracture (neck of the metatarsal)
- Rheumatoid arthritis
- Plexiform neurofibroma
- Hammertoe
Epidemiology and Demographics
- Neuroma is a uncommon disease.[4]
Age
- Neuroma is more commonly observed among patients aged between 15 to 50 years old.[4]
- Neuroma is more commonly observed among middle aged adults.
Gender
- Females are more commonly affected with neuroma than males.
- The female to male ratio is approximately 5:1.[4]
Race
- There is no racial predilection for neuroma.
Risk Factors
- Common risk factors in the development of neuroma include:[3]
- Improper footwear
- High-impact sports (e.g., rock-climbing, ballet dancing)
Natural History, Complications and Prognosis
- The majority of patients with neuroma are symptomatic at the time of diagnosis.[2]
- Early clinical features include neuropathic pain or local tenderness.
- If left untreated, the majority of patients with neuroma may progress to develop difficulty walking and limping.
- A significant complication of neuroma is chronic neuropathic pain.
- Prognosis is generally good, and the survival rate of patients with neuroma is 99%.
Diagnosis
Symptoms
- Neuroma is usually asymptomatic.
- Symptoms of neuroma may include:[2]
- Focal area of neuropathic pain
- No alleviating factors
- Aggravating with movement
Physical Examination
- Patients with neuroma usually appear with antalgic posture.[2]
- Physical examination may be remarkable for:
- Tenderness to palpation
- Limitation of range of motion
- Dysesthetic pain
Laboratory Findings
- There are no specific laboratory findings associated with neuroma.[3]
Imaging Findings
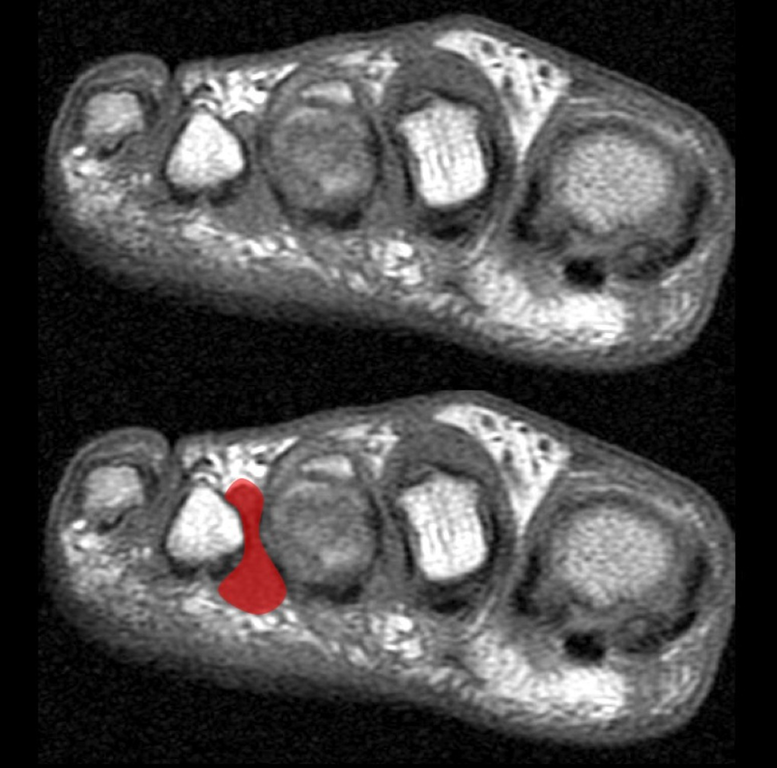
- On MRI, characteristic findings of neuroma include:
- Dumbbell/ovoid-shaped lesion at a similar position to that described on ultrasound
- T1: typically low-to-iso signal
- T2: typically low signal but can sometimes be intermediate in signal
- T1 C+ (Gd): tends to show intense enhancement
- On MRI, characteristic findings of traumatic neuroma include:[2]
- Fusiform swelling of a nerve or a bulbous mass at a nerve end
- The parent nerve of some small nerve may difficult or impossible to discern
- T2/STIR:inhomogeneous hyperintensity (may have a hypointense rim)
- T1 C+ (Gd): variable contrast enhancement
- The image below demonstrates MRI findings of traumatic neuroma.
-
Morton neuroma MRICourtesy of Radiopedia
- On ultrasound, neuroma is characterized by the following findings:[2]
- Round to ovoid
- Well-defined, hypoechoic lesion
- Located in the intermetatarsal space proximal to the metatarsal head
- On ultrasound, traumatic neuroma is characterized by the following findings:[2]
- Swollen nerve (mass-like)
- Hypoechoic
- Loss of normal fibrillar pattern
- Usually small, but may be as large as 5 cm.
Treatment
Medical Therapy
- Medical therapy for neuroma may include:[2]
- Tricyclic antidepressants
- Anticonvulsants (more effective)
- Serotonin-norepinephrine reuptake inhibitors
- Ultrasound-guided interdigital injection of steroid and local anaesthetic.
Surgery
- Surgery is the mainstay of therapy for neuroma.
- Surgical excision is the treatment of choice for patients with neuroma; this surgical intervention is associated with a relatively favorable success rate, approximately 80%.
- The recurrence rate after surgery is as high as 50%.
Prevention
- There are no primary preventive measures available for neuroma.[2]
- Secondary prevention measures include: personal hygiene measures, such as wearing ergonomic shoes.
References
- ↑ "Neuroma". Dorland's Illustrated Medical Dictionary (32nd ed.). Oxford University Press. 2011. p. 5287. ISBN 978-1-4557-0985-4. Retrieved 25 August 2013.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Neuroma. Radiopedia http://radiopaedia.org/cases/morton-neuroma-2 Accessed on April 21, 2016
- ↑ 3.0 3.1 3.2 3.3 3.4 Neuroma. Wikipedia. https://en.wikipedia.org/wiki/Neuroma Accessed on April 21, 2016
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Wu J, Chiu DT (1999). "Painful neuromas: a review of treatment modalities". Ann Plast Surg. 43 (6): 661–7. PMID 10597831.