Myocardial rupture
| Myocardial rupture | |
 | |
|---|---|
| Ventricular septum rupture at posterior wall | |
| ICD-10 | I23.3-I23.5 |
| eMedicine | med/1571 |
| MeSH | D006341 |
For patient information click here
| Cardiology Network |
 Discuss Myocardial rupture further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Myocardial rupture is a laceration or tearing of the walls of the ventricles or atria of the heart, of the interatrial or interventricular septum, of the papillary muscles or chordae tendineae or of one of the valves of the heart. It is most commonly seen as a serious sequelae of an acute myocardial infarction (heart attack).
Incidence
The incidence of myocardial rupture has decreased in the era of urgent revascularization and aggressive pharmacological therapy for the treatment of an acute myocardial rupture. However, the decrease in the incidence of myocardial rupture is not uniform; there is a slight increase in the incidence of rupture if thrombolytic agents are used to abort a myocardial infarction.[1] On the other hand, if primary percutaneous coronary intervention is performed to abort the infarction, the incidence of rupture is significantly lowered.[2] The incidence of myocardial rupture if PCI is performed in the setting of an acute myocardial infarction is about 1 percent.[3]
Relative Contribution of Myocardial Rupture, Cardiac Arrest Versus and Recurrent MI as a Cause of Sudden Death Following STEMI
Despite implantation of AICDs, there remains a high incidence of sudden death following ST elevation MI. This is due to the fact that not all sudden death is due to arrythmias in the period following ST elevation MI. Based upon autopsy findings, the relative frequency of various pathophysiologic events among 105 cases was as follows[4]:
- 3 Index MIs in the first 7 days (2.9%)
- 28 Recurrent MIs (26.6%)
- 13 Cardiac ruptures (12.4%)
- 4 Pump failures (3.8%)
- 2 Other cardiovascular causes (stroke or pulmonary embolism; 1.9%)
- 1 Noncardiovascular cause (1%)
- 54 cases (51.4%) had no acute specific autopsy evidence other than the index MI and were thus presumed arrhythmic.
The relative contribution of arrhythmic death was lowest in the first month, while the relative contribution of recurrent MI or cardiac rupture was highest in the first month following ST elevation MI. After three months, however, the relative contribution shifted so that the proportion of cases attributable to arrhythmias was significantly higher than recurrent MI or rupture (P<0.0001).
Pathophysiology
The most common cause of myocardial rupture is a recent myocardial infarction, with the rupture typically occurring three to five days after infarction. Other causes of rupture include cardiac trauma, endocarditis (infection of the heart),[5][6] cardiac tumors, infiltrative diseases of the heart,[5] and aortic dissection.
Risk Factors for Myocardial Rupture
Risk factors for rupture after an acute myocardial infarction include female gender,[3][2] advanced age of the individual,[3][2] and a low body mass index.[3] Other presenting signs associated with myocardial rupture include a pericardial friction rub, sluggish flow in the coronary artery after it is opened, the left anterior descending artery being the cause of the acute MI,[3][2][7] and delay of revascularization greater than 2 hours.[2]
Classification
Myocardial ruptures can be classified as one of three types.
Type I
An abrupt slit-like tear that generally occurs within 24 hours of an acute myocardial infarction.
Type II
An erosion of the infarcted myocardium, which is suggestive of a slow tear of the dead myocardium. Type II ruptures typically occur more than 24 hours after the infarction occurred.
Type III
These ruptures are characterized by early aneurysm formation and subsequent rupture of the aneurysm.[8]
Alternate classification scheme
Another method for classifying myocardial ruptures is by the anatomical portion of the heart that has ruptured. By far the most dramatic is rupture of the free wall of the left of right ventricles, as this is associated with immediate hemodynamic collapse and death secondary to acute pericardial tamponade. Rupture of the interventricular septum will cause a ventricular septal defect. Rupture of a papillary muscle will cause acute mitral regurgitation.
Diagnosis
Due to the acute hemodynamic deterioration associated with myocardial rupture, the diagnosis is generally made based on physical examination, changes in the vital signs, and clinical suspicion. The diagnosis can be confirmed with echocardiography.
Signs and symptoms
Symptoms of myocardial rupture are recurrent or persistent chest pain, syncope, and distension of jugular veins.
Pathological Findings
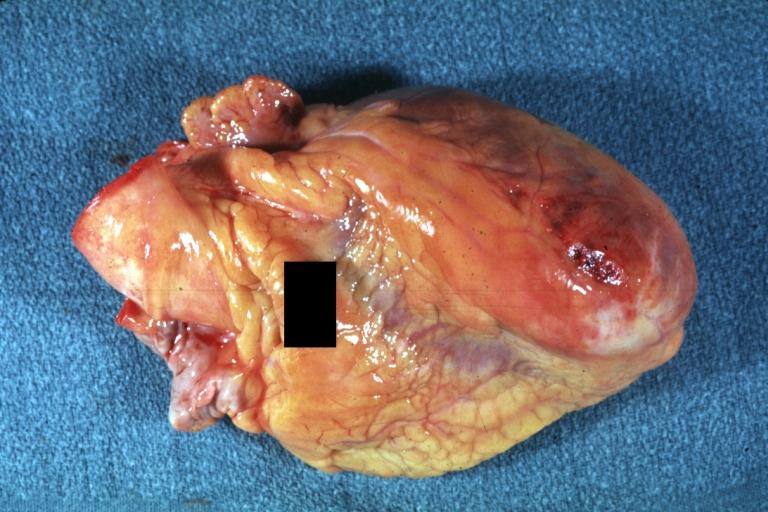
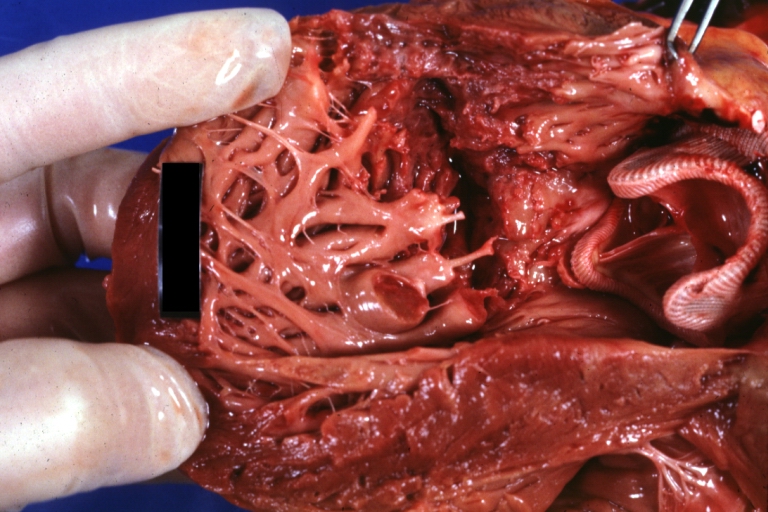
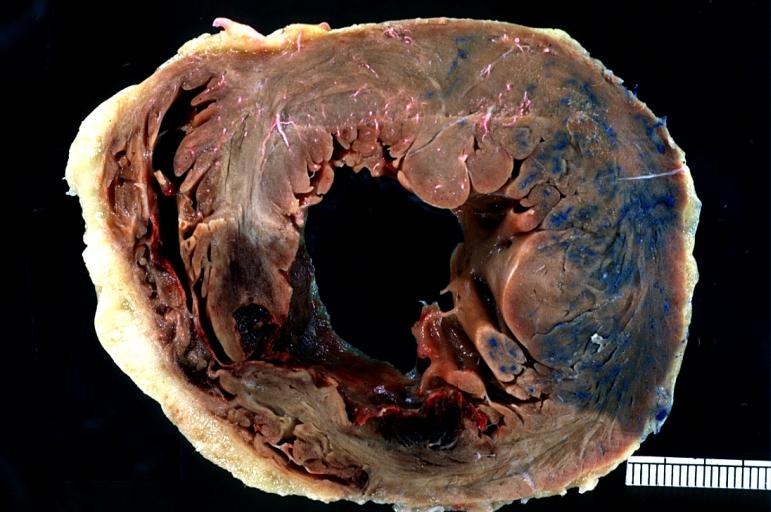
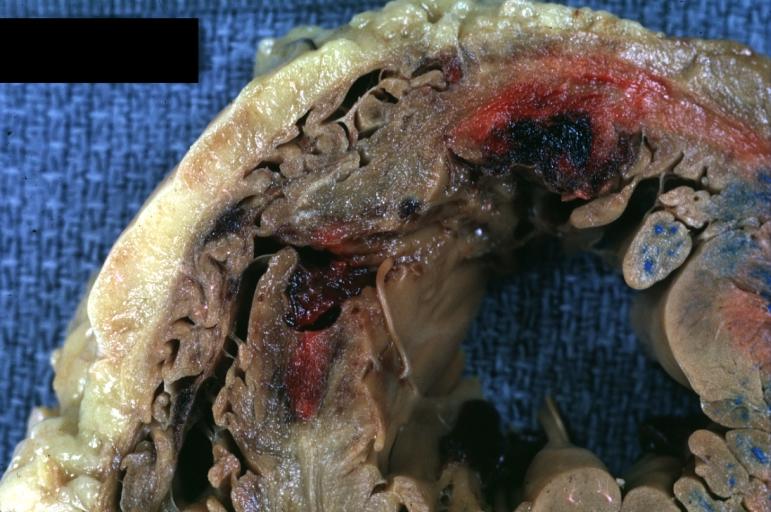
Myocardial Rupture of the Free Wall
-
Gross horizontal section of ruptured anterolateral infarct
-
Gross, Acute MI, external view of ruptured myocardial infarction near apex
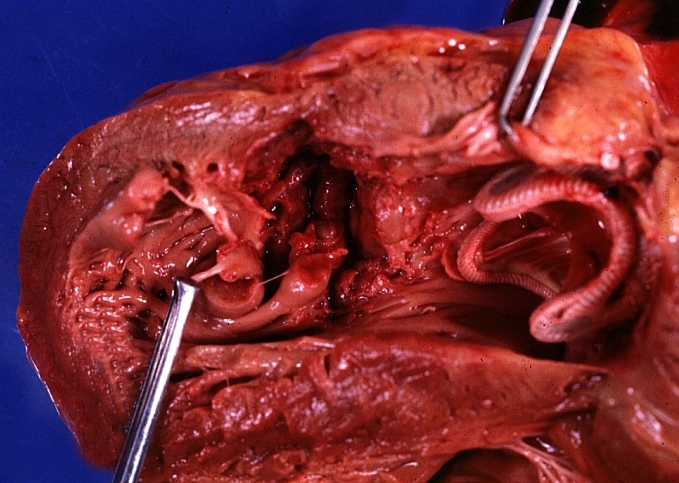
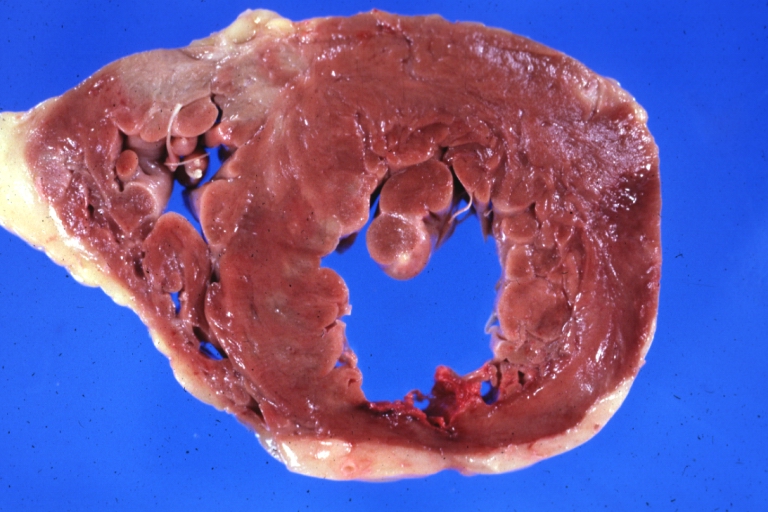
Ventricular Septal Rupture
Treatment
The treatment for myocardial rupture is supportive in the immediate setting and surgical correction of the rupture, if feasible. A certain small percentage of individuals do not seek medical attention in the acute setting survive. In this setting, it may be reasonable to treat the rupture medically and delay or avoid surgery completely, depending on the individual's comorbid medical issues.
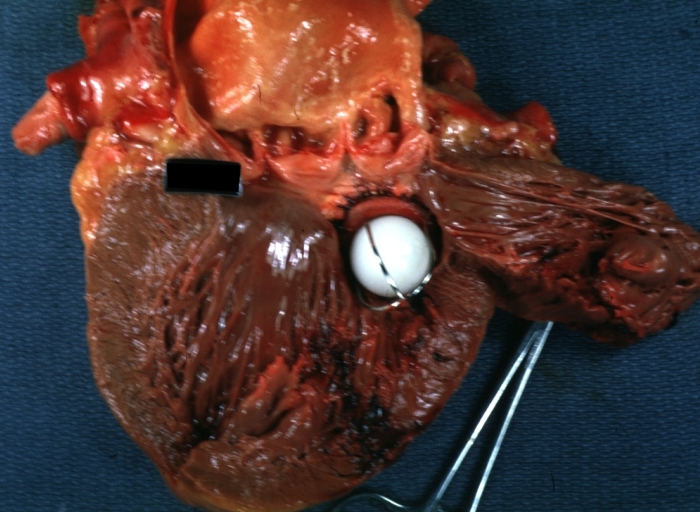
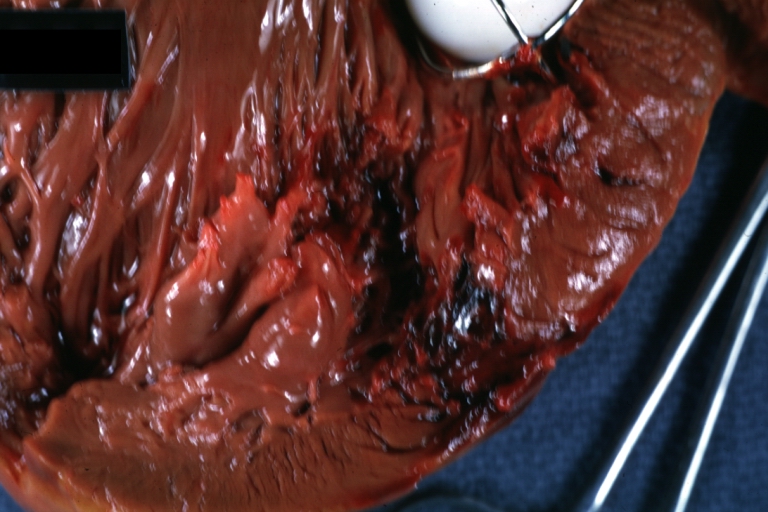
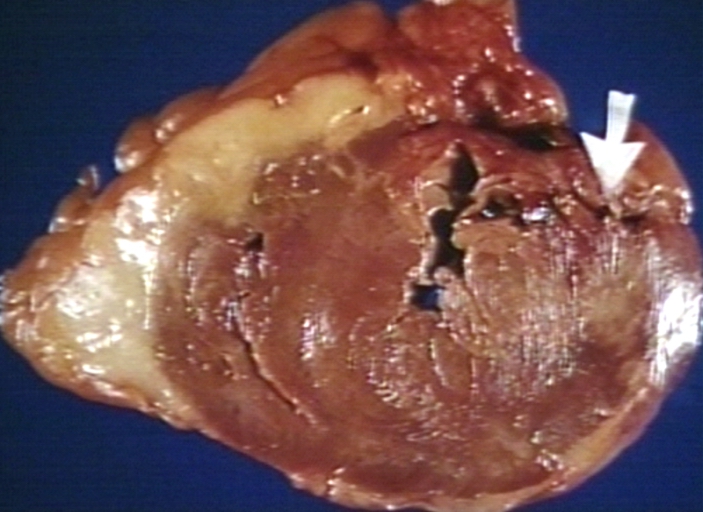
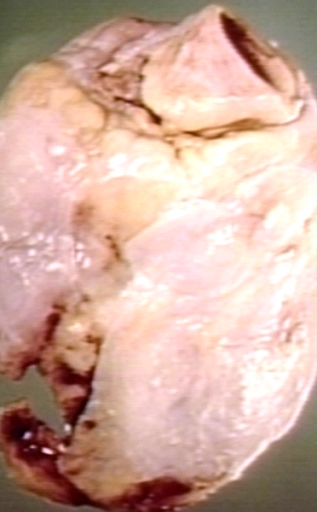
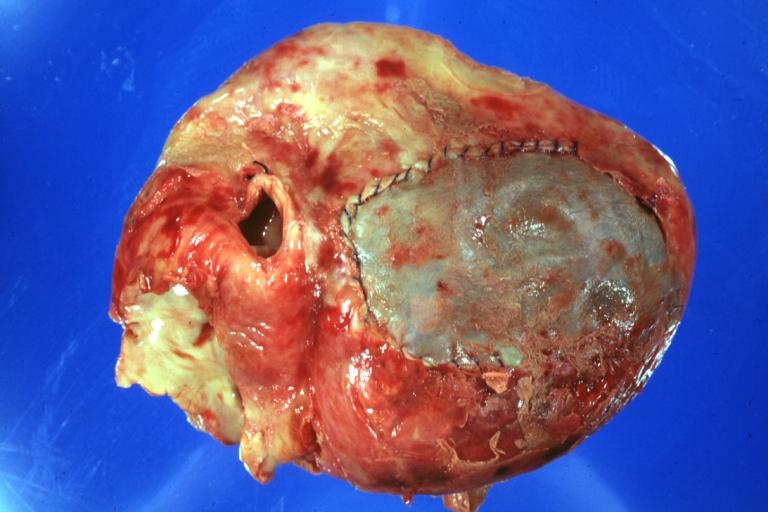
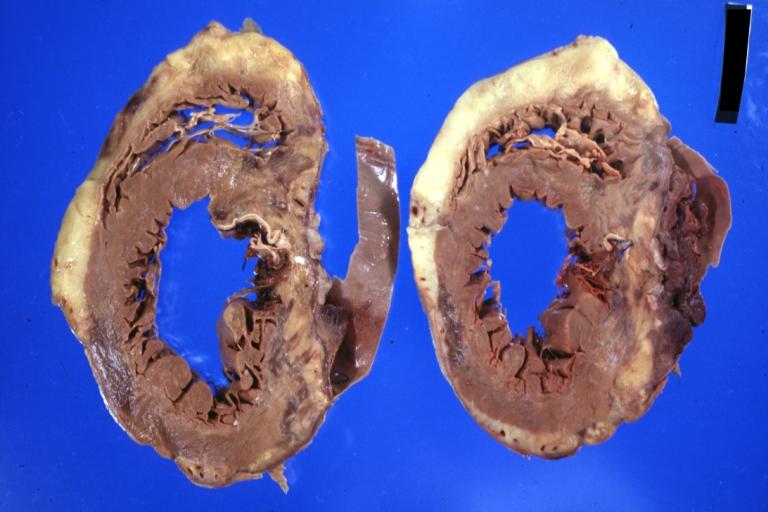
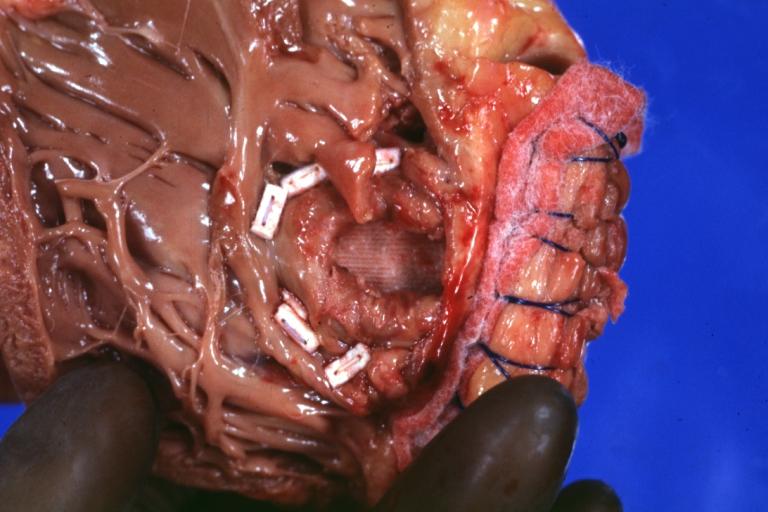
Pathologic Images Following Patch Repairs
Images shown below are courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Gross natural color external view of heart with repair patch over ruptured anterior infarction. A horizontal section of fixed ventricles
-
IAcute MI:Gross fixed tissue horizontal section ventricles. A large anterior infarct rupture with repair patch.
-
Gross natural color close-up of apical patch repair of ruptured infarct seen from right ventricle side septal rupture
Prognosis
The prognosis of myocardial rupture is dependant on a number of factors, including which portion of the myocardium is involved in the rupture. In one case series, if myocardial rupture involved the free wall of the left ventricle, the mortality rate was 100 percent.[3] Even if the individual survives the initial hemodynamic sequelae of the rupture, the 30 day mortality is still significantly higher than if rupture did not occur.[3]
ACC/AHA Guidelines- Recommendations for Ventricular Septal Rupture After STEMI (DO NOT EDIT)[9]
| “ |
Class I1. Patients with STEMI complicated by the development of a VSR should be considered for urgent cardiac surgical repair, unless further support is considered futile because of the patient’s wishes or contraindications/ unsuitability for further invasive care. (Level of Evidence: B) 2. Coronary artery bypass grafting should be undertaken at the same time as repair of the VSR. (Level of Evidence: B) |
” |
Sources
- The 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction [9]
- The 2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST-Elevation Myocardial Infarction [10]
References
- ↑ Becker RC, Gore JM, Lambrew C, Weaver WD, Rubison RM, French WJ, Tiefenbrunn AJ, Bowlby LJ, Rogers WJ. (1996). "A composite view of cardiac rupture in the United States National Registry of Myocardial Infarction". J Am Coll Cardiol. 27 (6): 1321–6. PMID 8626938.
- ↑ 2.0 2.1 2.2 2.3 2.4 Moreno R, Lopez-Sendon J, Garcia E, Perez de Isla L, Lopez de Sa E, Ortega A, Moreno M, Rubio R, Soriano J, Abeytua M, Garcia-Fernandez MA. (2002). "Primary angioplasty reduces the risk of left ventricular free wall rupture compared with thrombolysis in patients with acute myocardial infarction". J Am Coll Cardiol. 39 (4): 598–603. PMID 11849857.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Yip HK, Wu CJ, Chang HW, Wang CP, Cheng CI, Chua S, Chen MC. (2003). "Cardiac rupture complicating acute myocardial infarction in the direct percutaneous coronary intervention reperfusion era" (PDF). Chest. 124 (2): 565–71. PMID 12907544.
- ↑ Pouleur AC, Barkoudah E, Uno H, Skali H, Finn PV, Zelenkofske SL, Belenkov YN, Mareev V, Velazquez EJ, Rouleau JL, Maggioni AP, Køber L, Califf RM, McMurray JJ, Pfeffer MA, Solomon SD (2010). "Pathogenesis of Sudden Unexpected Death in a Clinical Trial of Patients With Myocardial Infarction and Left Ventricular Dysfunction, Heart Failure, or Both". Circulation. doi:10.1161/CIRCULATIONAHA.110.940619. PMID 20660803. Retrieved 2010-08-10. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Lin TH, Su HM, Voon WC, Lai HM, Yen HW, Lai WT, Sheu SH. (2006). "Association between hypertension and primary mitral chordae tendinae rupture". Am J Hypertens. 19 (1): 75–9. PMID 16461195.
- ↑ de Diego C, Marcos-Alberca P, Pai RK. (2006). "Giant periprosthetic vegetation associated with pseudoaneurysmal-like rupture" (PDF). Eur Heart J. 27 (8): 912. PMID 16569654.
- ↑ Sugiura T, Nagahama Y, Nakamura S, Kudo Y, Yamasaki F, Iwasaka T. (2003). "Left ventricular free wall rupture after reperfusion therapy for acute myocardial infarction". Am J Cardiol. 92 (3): 282–4. PMID 12888132.
- ↑ Becker AE, van Mantgem JP. (1975). "Cardiac tamponade. A study of 50 hearts". Eur J Cardiol. 3 (4): 349–58. PMID 1193118.
- ↑ 9.0 9.1 Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK (2004). "ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction)". Circulation. 110 (9): e82–292. PMID 15339869. Unknown parameter
|month=ignored (help) - ↑ Antman EM, Hand M, Armstrong PW; et al. (2008). "2007 Focused Update of the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: developed in collaboration With the Canadian Cardiovascular Society endorsed by the American Academy of Family Physicians: 2007 Writing Group to Review New Evidence and Update the ACC/AHA 2004 Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction, Writing on Behalf of the 2004 Writing Committee". Circulation. 117 (2): 296–329. doi:10.1161/CIRCULATIONAHA.107.188209. PMID 18071078. Unknown parameter
|month=ignored (help)