Multifocal atrial tachycardia
| Multifocal atrial tachycardia | |
 |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2] Syed Hassan A. Kazmi BSc, MD [3]
Synonyms and keywords: MAT
Overview
Multifocal atrial tachycardia (MAT) or also called chaotic atrial tachycardia is a cardiac arrhythmia, specifically a type of supraventricular tachycardia (rate exceeding 100 beats per minute). This is characterized by 3 or more different P wave shapes or contour, variable PP, PR and RR intervals. Most P waves are conducted to the ventricles but some are not. Some R waves are aberrantly conducted.This variability makes it look irregular on the surface ECG and often misinterpreted as atrial fibrillation.
A rhythm with same the ECG characteristics but at a slow rate is called multifocal atrial rhythm (MAR).
It can be seen among elderly patients with COPD and CHF and eventually develop into atrial fibrillation.
Causes
Multifocal atrial tachycardia usually results from an underlying medical condition such as COPD, chronic renal failure, pulmonary embolism, electrolyte imbalance, and many other conditions.
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
- Aminophylline toxicity
- Congestive heart failure
- Hypokalemia
- Hypoxia
- Myocardial infarction
- Pulmonary embolism
- Sepsis
Common Causes
- Chronic obstructive pulmonary disease
- Chronic renal failure
- Congestive heart failure
- Diabetes mellitus
- Hypokalemia
- Hypoxia
- Myocardial infarction
- Pneumonia
- Pulmonary embolism
- Sepsis
Causes by Organ System
| Cardiovascular | Congestive heart failure, myocardial infarction, valvular heart disease |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | Aminophylline, isoproterenol, theophylline |
| Ear Nose Throat | No underlying causes |
| Endocrine | Diabetes mellitus |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | Postoperative complication |
| Infectious Disease | Pneumonia, sepsis |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | Lung cancer |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | Aminophylline |
| Psychiatric | No underlying causes |
| Pulmonary | Chronic obstructive pulmonary disease, hypoxia, lung cancer, pneumonia, pulmonary embolism |
| Renal/Electrolyte | Chronic renal failure, hypokalemia, hypomagnesemia |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order
Diagnosis
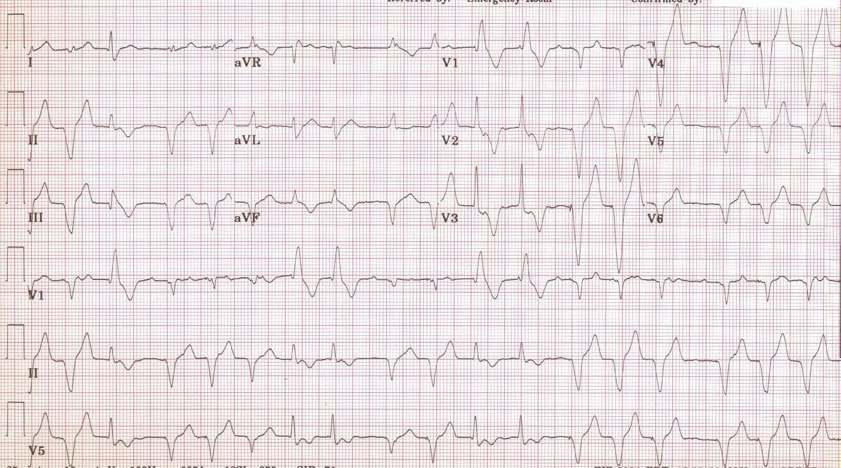
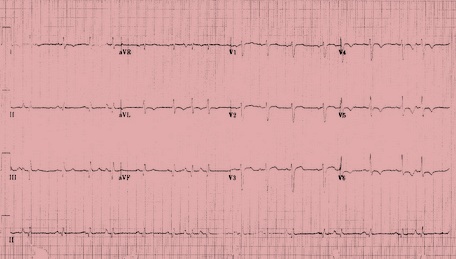
Electrocardiography
- There are P waves of varying morphology from at least three different foci
- There is absence of one dominant atrial pacemaker
- Variable PP intervals, RR intervals, and PR intervals
- Atrial rate is above 100 beats per minute (bpm)
- Can be mistaken for atrial fibrillation if the p waves are of low amplitude
- High incidence in the elderly and in those with COPD
Differentiating Multifocal Atrial Tachycardia From Other Disease
| Arrhythmia | Rhythm | Rate | P wave | PR Interval | QRS Complex | Response to Maneuvers | Epidemiology | Co-existing Conditions |
|---|---|---|---|---|---|---|---|---|
| Atrial Fibrillation (AFib)[1][2] |
|
|
|
|
|
|
|
|
| Atrial Flutter[3] |
|
|
|
|
|
|
|
|
| Atrioventricular nodal reentry tachycardia (AVNRT)[4][5][6][7] |
|
|
|
|
|
|
|
|
| Multifocal Atrial Tachycardia[8][9] |
|
|
|
|
|
|
|
|
| Paroxysmal Supraventricular Tachycardia |
|
|
|
|
|
|
|
|
| Premature Atrial Contractrions (PAC)[10][11] |
|
|
|
|
|
|
||
| Wolff-Parkinson-White Syndrome[12][13] |
|
|
|
|
|
|
|
|
| Ventricular Fibrillation (VF)[14][15][16] |
|
|
|
|
|
|
|
|
| Ventricular Tachycardia[17][18] |
|
|
|
|
|
|
|
|
References
- ↑ Lankveld TA, Zeemering S, Crijns HJ, Schotten U (July 2014). "The ECG as a tool to determine atrial fibrillation complexity". Heart. 100 (14): 1077–84. doi:10.1136/heartjnl-2013-305149. PMID 24837984.
- ↑ Harris K, Edwards D, Mant J (2012). "How can we best detect atrial fibrillation?". J R Coll Physicians Edinb. 42 Suppl 18: 5–22. doi:10.4997/JRCPE.2012.S02. PMID 22518390.
- ↑ Cosío FG (June 2017). "Atrial Flutter, Typical and Atypical: A Review". Arrhythm Electrophysiol Rev. 6 (2): 55–62. doi:10.15420/aer.2017.5.2. PMC 5522718. PMID 28835836.
- ↑ Katritsis DG, Josephson ME (August 2016). "Classification, Electrophysiological Features and Therapy of Atrioventricular Nodal Reentrant Tachycardia". Arrhythm Electrophysiol Rev. 5 (2): 130–5. doi:10.15420/AER.2016.18.2. PMC 5013176. PMID 27617092.
- ↑ Letsas KP, Weber R, Siklody CH, Mihas CC, Stockinger J, Blum T, Kalusche D, Arentz T (April 2010). "Electrocardiographic differentiation of common type atrioventricular nodal reentrant tachycardia from atrioventricular reciprocating tachycardia via a concealed accessory pathway". Acta Cardiol. 65 (2): 171–6. doi:10.2143/AC.65.2.2047050. PMID 20458824.
- ↑ "Atrioventricular Nodal Reentry Tachycardia (AVNRT) - StatPearls - NCBI Bookshelf".
- ↑ Schernthaner C, Danmayr F, Strohmer B (2014). "Coexistence of atrioventricular nodal reentrant tachycardia with other forms of arrhythmias". Med Princ Pract. 23 (6): 543–50. doi:10.1159/000365418. PMC 5586929. PMID 25196716.
- ↑ Scher DL, Arsura EL (September 1989). "Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment". Am. Heart J. 118 (3): 574–80. doi:10.1016/0002-8703(89)90275-5. PMID 2570520.
- ↑ Goodacre S, Irons R (March 2002). "ABC of clinical electrocardiography: Atrial arrhythmias". BMJ. 324 (7337): 594–7. doi:10.1136/bmj.324.7337.594. PMC 1122515. PMID 11884328.
- ↑ Lin CY, Lin YJ, Chen YY, Chang SL, Lo LW, Chao TF, Chung FP, Hu YF, Chong E, Cheng HM, Tuan TC, Liao JN, Chiou CW, Huang JL, Chen SA (August 2015). "Prognostic Significance of Premature Atrial Complexes Burden in Prediction of Long-Term Outcome". J Am Heart Assoc. 4 (9): e002192. doi:10.1161/JAHA.115.002192. PMC 4599506. PMID 26316525.
- ↑ Strasburger JF, Cheulkar B, Wichman HJ (December 2007). "Perinatal arrhythmias: diagnosis and management". Clin Perinatol. 34 (4): 627–52, vii–viii. doi:10.1016/j.clp.2007.10.002. PMC 3310372. PMID 18063110.
- ↑ Rao AL, Salerno JC, Asif IM, Drezner JA (July 2014). "Evaluation and management of wolff-Parkinson-white in athletes". Sports Health. 6 (4): 326–32. doi:10.1177/1941738113509059. PMC 4065555. PMID 24982705.
- ↑ Rosner MH, Brady WJ, Kefer MP, Martin ML (November 1999). "Electrocardiography in the patient with the Wolff-Parkinson-White syndrome: diagnostic and initial therapeutic issues". Am J Emerg Med. 17 (7): 705–14. doi:10.1016/s0735-6757(99)90167-5. PMID 10597097.
- ↑ Glinge C, Sattler S, Jabbari R, Tfelt-Hansen J (September 2016). "Epidemiology and genetics of ventricular fibrillation during acute myocardial infarction". J Geriatr Cardiol. 13 (9): 789–797. doi:10.11909/j.issn.1671-5411.2016.09.006. PMC 5122505. PMID 27899944.
- ↑ Samie FH, Jalife J (May 2001). "Mechanisms underlying ventricular tachycardia and its transition to ventricular fibrillation in the structurally normal heart". Cardiovasc. Res. 50 (2): 242–50. doi:10.1016/s0008-6363(00)00289-3. PMID 11334828.
- ↑ Adabag AS, Luepker RV, Roger VL, Gersh BJ (April 2010). "Sudden cardiac death: epidemiology and risk factors". Nat Rev Cardiol. 7 (4): 216–25. doi:10.1038/nrcardio.2010.3. PMC 5014372. PMID 20142817.
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Levis JT (2011). "ECG Diagnosis: Monomorphic Ventricular Tachycardia". Perm J. 15 (1): 65. doi:10.7812/tpp/10-130. PMC 3048638. PMID 21505622.