Mitral stenosis surgery
For the WikiPatient page for this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Mohammed A. Sbeih, M.D.[2];

Overview
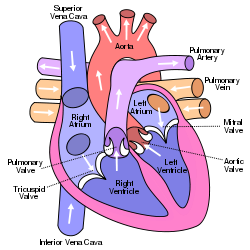
Mitral valve surgery is a surgery that can either repair or replace the mitral valve in the heart. Blood that flows between different chambers of the heart must flow through a valve. One such valve is called the mitral valve. It opens up enough so blood can flow from one chamber of the heart (left atria) to the next chamber (left ventricle). It then closes, keeping blood from flowing backwards.
Mitral stenosis is a valvular heart disease characterized by the narrowing of the orifice of the mitral valve of the heart.[1]. Severe mitral stenosis (MS) is eventually lethal disease unless treated with vulvotomy or valve replacement, it may progress to serious complications like pulmonary hypertension, heart failure and death. Most of the cases are due to rheumatic heart disease.
In open surgery, the surgeon makes a large cut in the sternum to reach the heart. Minimally invasive mitral valve surgery is done through much smaller surgical cuts than the large cuts needed for open surgery.
Anatomy and pathophysiology
Anatomy
The mitral valve is typically 4–6 cm² in area. It has two cusps, or leaflets, (the anteromedial leaflet and the posterolateral leaflet) that guard the opening. The opening is surrounded by a fibrous ring known as the mitral valve annulus [2]. The anterior cusp protects approximately two-thirds of the valve (imagine a crescent moon within the circle, where the crescent represents the posterior cusp). Note that although the anterior leaflet takes up a larger part of the ring and rises higher, the posterior leaflet has a larger surface area. These valve leaflets are prevented from prolapsing into the left atrium by the action of tendons attached to the posterior surface of the valve, chordae tendineae.
The inelastic chordae tendineae are attached at one end to the papillary muscles and the other to the valve cusps. Papillary muscles are fingerlike projections from the wall of the left ventricle. Chordae tendineae from each muscle are attached to both leaflets of the mitral valve. Thus, when the left ventricle contracts, the intraventricular pressure forces the valve to close, while the tendons keep the leaflets coapting together and prevent the valve from opening in the wrong direction (thus preventing blood to flow back to the left atrium). Each chord has a different thickness. The thinnest ones are attached to the free leaflet margin, whereas thickest ones are attached quite away from the free margin. This disposition has important effects on systolic stress distribution physiology [3].
Pathophysiology
During left ventricular diastole, after the pressure drops in the left ventricle due to relaxation of the ventricular myocardium, the mitral valve opens, and blood travels from the left atrium to the left ventricle. About 70-80% of the blood that travels across the mitral valve occurs during the early filling phase of the left ventricle. This early filling phase is due to active relaxation of the ventricular myocardium, causing a pressure gradient that allows a rapid flow of blood from the left atrium, across the mitral valve. This early filling across the mitral valve is seen on doppler echocardiography of the mitral valve as the E wave. After the E wave, there is a period of slow filling of the ventricle.
Left atrial contraction (during left ventricular diastole) causes added blood to flow across the mitral valve immediately before left ventricular systole. This late flow across the open mitral valve is seen on doppler echocardiography of the mitral valve as the A wave. The late filling of the LV contributes about 20% to the volume in the left ventricle prior to ventricular systole, and is known as the atrial kick.
The mitral annulus changes in shape and size during the cardiac cycle. It is smaller at the end of atrial systole due to the contraction of the left atrium around it, like a sphincter. This reduction in annulus size at the end of atrial systole may be important for the proper coapting of the leaflets of the mitral valve when the left ventricle contracts and pumps blood [4].
The closing of the mitral valve and the tricuspid valve constitutes the first heart sound (S1). It is not actually the valve closure which produces a sound but rather the sudden cessation of blood flow caused by the closure of the mitral and tricuspid valves. The mitral valve opening is normally not heard except in mitral stenosis as the opening Snap. Flow of blood into the heart during rapid filling is not normally heard except in certain pathological states where it constitutes the third heart sound (S3).
Thickening and immobility of the mitral valve leaflets causes an obstruction in blood flow from the left atrium to left ventricle (Mitral stenosis). As a result, the pressure in the left atrium increases, also the pressure in the pulmonary vasculature and right side of the heart increases. Mitral stenosis may cause left ventricular dysfunction if it is associated with mitral regurgitation [5].
Almost all cases of mitral stenosis are due to disease in the heart secondary to rheumatic fever and the consequent rheumatic heart disease (a condition that may develop after strep throat or scarlet fever). Around 90% of cases of rheumatic heart disease are associated with mitral stenosis [6]. The valve problems develop 5 - 10 years after the rheumatic fever, a tiny nodules forms along the valve leaflets [7], the leaflets eventually thicken with deposition of fibrin. The cusps may become fibrosed, calcified and thickened over a span of a decade [8][9]. Chronic turbulent flow through a deformed valve appears to cause these changes and as a result the valve losses it's normal morphology [5]. The degree of leaflet thickening and calcification and the severity of chordal involvement are variable. Rheumatic fever is becoming rare in the United States, so mitral stenosis is also less common [10][11].
Severity of Mitral stenosis
The severity of mitral stenosis depends on the pressure gradient between the left atrium and ventricle which depends on the cross sectional area of the mitral valve. The normal mitral valve orifice has a cross sectional area of about 4.0 cm2.
- Mitral stenosis is mild if the cross sectional area is about 2 cm2 and the pressure gradient is small.
- Mitral stenosis is moderate if the cross sectional area is about 1.0 to 1.5 cm2.
- Mitral stenosis is severe if the cross sectional area is ≤1.0 cm2 and the pressure gradient between the left atrium and left ventricle is significant.
Usually, the rate of decrement in the valve area is about 0.1 cm2/year once mitral stenosis is present [12][13].
In pregnancy, the pressure gradient between the left atrium and ventricle is usually increased due to the increase in the heart rate and cardiac output during pregnancy. This can lead to the diagnosis of previously asymptomatic case of mitral stenosis, or worsening of the symptoms of previously diagnosed case.
Symptoms of Mitral stenosis
In adults there may be no symptoms. Symptoms may, however, appear or get worse with exercise or any activity that raises the heart rate. In adults, symptoms usually develop between ages 20 - 50. Symptoms may begin with an episode of atrial fibrillation, or may be triggered by pregnancy or other stress on the body, such as infection in the heart or lungs, or other heart disorders.
Symptoms may include:
- Chest discomfort.
- Heart failure symptoms, such as dyspnea on exertion, orthopnea and paroxysmal nocturnal dyspnea.
- Palpitations.
- Chest pain.
- Hemoptysis.
- Thromboembolism
- Frequent respiratory infections such as bronchitis.
- Ascites and edema (if right-sided heart failure develops).
- Fatigue, becoming tired easily.
Symptoms increase with exercise and pregnancy
In infants and children, symptoms may be present from birth (congenital), and almost always develop within the first 2 years of life. Symptoms include:
- Bluish discoloration of the skin or mucus membranes (cyanosis)
- Poor growth
- Shortness of breath
Causes of Mitral stenosis include:
- Almost all cases of mitral stenosis are due to disease in the heart secondary to rheumatic fever and the consequent rheumatic heart disease.
- Calcification of the mitral valve leaflets.
- There are primary causes of mitral stenosis that emanate from a cleft mitral valve.
- Bacterial endocarditis where the vegetations may favor increase risk of stenosis.
- Radiation treatment to the chest.
- Some medications may cause mitral stenosis.
Children may be born with mitral stenosis (congenital) or other birth defects involving the heart that cause mitral stenosis. Often, there are other heart defects present, along with the mitral stenosis. Mitral stenosis may run in families. Mitral stenosis is the most common valvular heart disease in pregnancy[14].
Treatments for Mitral valve stenosis
The choice of treatment depends on the symptoms present and the condition and function of the heart. Patients with high blood pressure or a weakened heart muscle may be given medications to reduce the strain on the heart and help improve the condition.
Anticoagulant or antiplatelet medications (blood thinners) may be used to prevent clots from forming in patients with atrial fibrillation.
Digitalis may be used to strengthen the heartbeat, along with diuretics (water pills) to remove excess fluid in the lungs.
A low-sodium diet may be helpful. Most people have no symptoms; but if a person develops symptoms, activity may be restricted.
Hospitalization may be required for diagnosis and treatment of severe symptoms. Surgical repair or replacement of the valve is recommended if heart function is poor, symptoms are severe, or the condition gets worse. Once the diagnosis of mitral stenosis is made, the patient should have regular follow-ups with a specialist to determine whether he or she need surgery.
Medical therapy can relieve symptoms, but the patient may need surgery to relieve the blood flow obstruction by mitral stenosis. Some studies showed that surgical treatment reduces the overall mortality rate of mitral stenosis compared to medical treatment [15][16][17].
Cases of mild mitral stenosis (mitral valve area >1.5 cm2) can be followed up yearly with history, physical examination, EKG and some imaging studies like echocardiography.
The 2006 American College of Cardiology/American Heart Association (AHA/AHA) guidelines for management of valvular heart disease recommended routine repeat echocardiography every year for patients with severe mitral stenosis, every one to two years for patients with moderate mitral stenosis and every three to five years for patients with mild mitral stenosis [18]. By echocardiography, the doctor can assess the pulmonary artery pressure to decide if the surgery is indicated for the patient with mitral stenosis or not.
2006 ACC/AHA guidelines on the management of valvular heart disease recommended long-term oral anticoagulation in patients with mitral stenosis who have a prior embolic event, left atrial thrombus, or atrial fibrillation [3,28,29].
The ACC/AHA guidelines suggested that oral anticoagulation may be considered in patients with severe MS, an enlarged left atrium, and spontaneous echo contrast, although the evidence was less well established [3].
Although the evidence is somewhat limited and controversial, we would anticoagulate those patients with visualized thrombus or spontaneous echo contrast in the left atrium. Support for this approach comes from a report of 168 patients with MS who underwent transesophageal echocardiography; 21 percent had a previous embolism and 46 percent were in atrial fibrillation [30]. Multiple logistic regression analysis showed that AF, mitral valve area, and left atrial enlargement were independent predictors of spontaneous echo contrast, and left atrial spontaneous echo contrast was the principal determinant of thromboembolism. (See "Mechanisms of thrombogenesis in atrial fibrillation".)
One exception to our agreement with the 2006 ACC/AHA and 2008 ACCP guidelines is that we do not suggest anticoagulation for patients with mitral stenosis and left atrial diameter ≥55 mm in the absence of another indication for anticoagulant therapy. Both guidelines suggested that, among patients with severe mitral stenosis without a prior embolic event or AF, long-term oral anticoagulation (target INR 2.5, range 2.0 to 3.0) may be considered if the left atrial diameter is ≥55 mm, although supporting evidence was less well established [3,28]. In the ACCP guidelines, this suggestion applies to patients with left atrial diameter >55 mm and any rheumatic mitral valve disease (not limited to those with severe mitral stenosis). This suggestion places a relatively high value on prevention of systemic embolism and a relatively low value on avoiding the bleeding risk and inconvenience associated with anticoagulation therapy.
Indications for Mitral valve stenosis surgery
Surgery is indicated in patients with symptomatic mitral valve stenosis, Surgery may be recommended in asymptomatic patients
The patient may also need valve surgery in the following conditions:
- The changes in the mitral valve are causing major heart symptoms, such as angina (chest pain), shortness of breath, fainting spells (syncope), or heart failure.
- Tests show that the changes in your mitral valve are beginning to seriously affect your heart function.
- The heart valve has been damaged by endocarditis (infection of the heart valve).
- The patient has received a new heart valve in the past, and it is not working well, or you have other problems such as blood clots, infection, or bleeding.
Mitral valve repair is recommended in following:
Mitral valve replacement is recommended in following:
- Extensive calcification or degeneration of a leaflet or annulus.
- Prolapse of more than one-third of the leaflet tissue.
- Extensive chordal fusion, calcification, or papillary muscle rupture.
- Extensive damage of mitral valve secondary to endocarditis.
Based on above, ACC/AHA 2008 guidelines
Preoperative preparation
The patient may need to have some tests before the procedure. The Cardiologist usually conducts a physical examination and diagnose the condition within few days, he or she will assess the general health of the patient and will recommend the most appropriate treatment for the patient and if he or she needs surgery. Some of the tests that can be done before the procedure include:
- Cardiac catheterization.
- Chest X-ray.
- Computed tomography (CT) scan.
- Echocardiogram (Doppler echocardiogram).
- Electrocardiogram (ECG).
- Electrophysiology tests.
- Exercise tests.
- Holter monitor.
- Magnetic resonance imaging (MRI).
Many patients with Mitral stenosis requiring surgery also have coronary artery disease
Before the surgery:
- The surgeon needs to know if the patient is taking any drugs, supplements, or herbs before the procedure.
- The patient may be able to store blood in the blood bank for transfusions during and after the surgery. The family members can also donate blood (autologous donation).
- For the 2-week period before surgery, the patient should be asked to stop taking drugs that make it harder for the blood to clot. These might cause increased bleeding during the surgery. Some of these drugs are aspirin, ibuprofen (Advil, Motrin), and naproxen (Aleve, Naprosyn).
- The day before the surgery, the patient should shower and shampoo well and wash the whole body below the neck with a special soap.
- The patient may also be asked to take an antibiotic to guard against infection.
- The patient should be informed which drugs he or she should still take on the day of the surgery.
- The patient should stop smoking.
On the day of the surgery:
- An intravenous (IV) line will be placed into a blood vessel in the patient's arm or chest to give fluids and medicines.
- The patient should be asked not to drink or eat anything after midnight the night before surgery. This includes chewing gum and using breath mints. The patient can rinse mouth with water if it feels dry without swallowing.
- Make sure that the patient is taking the drugs that he or she needs to take with a small sip of water.
- Hair near the incision site may be shaved immediately before the surgery.
- The patient should be informed when to arrive to hospital on the day of the surgery.
The procedure
The Procedure can be done either by the traditional open heart surgery or by the Minimally invasive surgery. Before the surgery, the patient will receive general anesthesia. This will make the patient asleep and pain-free during the entire procedure.
- In theTraditional open heart surgery:
- The surgeon will make a 10-inch-long cut in the middle of the chest (sternum).
- Next, the surgeon will separate the breastbone (sternum) to be able to see the heart.
- Most people are connected to a heart-lung bypass machine or bypass pump. The heart is stopped while the patient is connected to this machine. This machine does the work of the heart while the heart is stopped.
- A small cut is made in the left side of the heart so the surgeon can repair or replace the mitral valve.
- In Minimally invasive mitral valve surgery; there are several different ways to perform the procedure:
- The heart surgeon may make a 2-inch to 3-inch-long cut in the right part of your chest near the sternum (breastbone). Muscles in the area will be divided so the surgeon can reach the heart. A small cut is made in the left side of the heart so the surgeon can repair or replace the mitral valve.
- In Endoscopic surgery, the surgeon makes one to four small holes in the chest, then he or she uses special instruments and a camera to do the surgery.
- For Robotically-assisted valve surgery, the surgeon makes two to four tiny cuts (about a ½ to a ¾ inch) in the chest. The surgeon uses a special computer to control robotic arms during the surgery. The surgeon sees a three-dimensional view of the heart and mitral valve on the computer. This method is very precise.
The patient may or may not need to be on a heart-lung machine for these types of surgery, but if not, the heart rate will be slowed by medicine or a mechanical device.
If the surgeon can repair the mitral valve, the patient may have:
- Ring annuloplasty: The surgeon repairs the ring-like part around the valve by sewing a ring of metal, cloth, or tissue around the valve.
- Valve repair: The surgeon trims, shapes, or rebuilds one or more of the three leaflets of the valve. The leaflets are flaps that open and close the valve.
If the mitral valve is too damaged, the patient will need a new valve. This is called Replacement surgery. The surgeon will remove the mitral valve and sew a new one into place. There are two types of valves:
1. Mechanical which is made of man-made (synthetic) materials, such as a metal like titanium. These valves last the longest, but the patient will need to take blood-thinning medicine, such as warfarin (Coumadin) or aspirin, for the rest of his or her life.
2. Biological which made of human or animal tissue. These valves last 10 to 12 years, but the patient may not need to take blood thinners for life.
Once the new or repaired valve is working, the surgeon will:
- Close the heart and take you off the heart-lung machine.
- Place catheters (tubes) around the heart to drain fluids that build up.
- Close the sternum with stainless steel wires. It will take about 6 weeks for the bone to heal. The wires will stay inside the body.
The patient may have a temporary pacemaker connected to the heart until his or her natural heart rhythm returns.
The surgeon may also perform coronary artery bypass surgery at the same time, if needed.
Recovery
Recovery at hospital The patient may spend 4 to 7 days in the hospital after surgery (much less in Minimally invasive mitral valve surgery-3 to 5 days). Then patient will wake up in the intensive care unit (ICU) and recover there for 1 or 2 days. Two to three tubes will be in the patient's chest to drain fluid from around the heart. They are usually removed 1 to 3 days after surgery.
The patient may have a catheter in the bladder to drain urine, and may also have intravenous lines to get fluids. Nurses will closely watch monitors that show information about the vital signs (pulse, temperature, and breathing).
The patient will be moved to a regular hospital room from the ICU. The nurses and doctors will continue to monitor the heart and vital signs until the patient is stable enough to go home. The patient will receive pain medicine to control pain around your surgical cut.
A nurse should help the patient to slowly resume some activity, and the patient should begin a physical therapy program to make the heart and body stronger. A temporary pacemaker may be placed in the patient's heart if the heart rate becomes too slow after surgery.
Recovery at home
The patient should be informed about the following:
- Taking care for his or her healing incisions.
- Recognizing signs of infection or other complications.
- Coping with after-effects of surgery.
- Followup appointments, medicines, and situations when he or she should call the doctor right away.
- When he or she can go back to daily routine, such as working, driving, and physical activity.
After-effects of heart surgery are normal. They may include muscle pain, chest pain, or swelling. Other after-effects may include loss of appetite, problems sleeping, constipation, and mood swings and depression. After-effects usually go away over time.
Less recovery time is needed for off-pump heart surgery and minimally invasive heart surgery.
Ongoing care
Ongoing care after valve surgery may include periodic checkups with the doctor. During these visits, the patient may have blood tests, an EKG (electrocardiogram), echocardiography, or a stress test. These tests will show how the patient's heart is working after the surgery.
Routine tests should be done to make sure the patient is getting the right amount of the blood-thinning medicine in case of Mechanical valve placement.
The patient may be advised to change his or her lifestyle, this includes: quitting smoking, making changes to diet, being physically active, and reducing and managing stress.
Surgical outcome
The results of mitral valve repair are excellent in the centers that regularly perform this surgery.
Techniques for minimally invasive heart valve surgery have improved greatly over the past 10 years. These techniques are safe for most patients, and they reduce recovery time and pain.
Valve repair versus valve replacement
Advantages of Mitral valve repair include:
- Lower operative mortality rate [19][20]
- Improves left ventricular EF and function [21].
- Preserves native heart valve and avoids the use of a prosthetic heart valve with its complications.
- Has good overall outcome with good survival rates [22][23][24].
- Lower risk for endocarditis.
- Avoids long term use of anticoagulants.
Mechanical versus Biological valves
Mechanical heart valves do not fail often. They last from 12 to 20 years. However, blood clots develop on them. If a blood clot forms, the patient may have a stroke. Bleeding can occur, but this is rare. Biological valves tend to fail over time [25][26], but they have a lower risk of blood clots.
Possible complications
Risks for any surgery
- Blood clots in the legs that may travel to the lungs.
- Blood loss.
- Breathing problems.
- Infection, including in the lungs, kidneys, bladder, chest, or heart valves.
- Reactions to medicines.
Possible risks from having open-heart surgery
- Heart attack or stroke.
- Heart rhythm problems.
- Infection in the cut, which is more likely to happen in people who are obese, have diabetes, or have already had this surgery.
- Memory loss and loss of mental clarity, or "fuzzy thinking."
- Post-pericardiotomy syndrome, which is a low-grade fever and chest pain. This could last for up to 6 months.
Prosthetic heart valves are associated with a variety of complications
- Structural deterioration, particularly with bioprosthetic valves.
- Valve obstruction due to thrombosis or pannus formation.
- Systemic embolization.
- Bleeding.
- Endocarditis and other infections.
- Left ventricular systolic dysfunction, which may be preexisting.
- Hemolytic anemia.
Videos
- Minimally invasive mitral valve surgery (Right thoracotomy approach video)
<youtube v=EnJQh_W3r3A/>
- Robotic mitral valve repair surgery animation-(1)
<youtube v=VrIxRfWDOm8/>
- Robotic mitral valve repair surgery animation-(2)
<youtube v=GYAmSH2zwic/>
External links
http://en.wikipedia.org/wiki/Mitral_valve#cite_note-0
http://en.wikipedia.org/wiki/Mitral_valve_stenosis
http://www.nlm.nih.gov/medlineplus/ency/article/000175.htm
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/before.html
http://www.mayoclinic.org/mitral-valve-disease/
http://www.nlm.nih.gov/medlineplus/ency/article/007411.htm
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/during.html
http://www.nhlbi.nih.gov/health/health-topics/topics/hs/after.html
References
- ↑ Carabello BA (2005). "Modern management of mitral stenosis". Circulation. 112 (3): 432–7. doi:10.1161/CIRCULATIONAHA.104.532498. PMID 16027271. Unknown parameter
|month=ignored (help) - ↑ Shinoda H, Stern PH (1992). "Diurnal rhythms in Ca transfer into bone, Ca release from bone, and bone resorbing activity in serum of rats". Am J Physiol. 262 (2 Pt 2): R235–40. PMID 1539731.
- ↑ Nazari S, Carli F, Salvi S, Banfi C, Aluffi A, Mourad Z; et al. (2000). "Patterns of systolic stress distribution on mitral valve anterior leaflet chordal apparatus. A structural mechanical theoretical analysis". J Cardiovasc Surg (Torino). 41 (2): 193–202. PMID 10901521.
- ↑ Pai RG, Varadarajan P, Tanimoto M (2003). "Effect of atrial fibrillation on the dynamics of mitral annular area". J Heart Valve Dis. 12 (1): 31–7. PMID 12578332.
- ↑ 5.0 5.1 Marcus RH, Sareli P, Pocock WA, Barlow JB (1994). "The spectrum of severe rheumatic mitral valve disease in a developing country. Correlations among clinical presentation, surgical pathologic findings, and hemodynamic sequelae". Ann Intern Med. 120 (3): 177–83. PMID 8043061.
- ↑ BLAND EF, DUCKETT JONES T (1951). "Rheumatic fever and rheumatic heart disease; a twenty year report on 1000 patients followed since childhood". Circulation. 4 (6): 836–43. PMID 14879491.
- ↑ Selzer A, Cohn KE (1972). "Natural history of mitral stenosis: a review". Circulation. 45 (4): 878–90. PMID 4552598.
- ↑ Rajamannan NM, Nealis TB, Subramaniam M, Pandya S, Stock SR, Ignatiev CI; et al. (2005). "Calcified rheumatic valve neoangiogenesis is associated with vascular endothelial growth factor expression and osteoblast-like bone formation". Circulation. 111 (24): 3296–301. doi:10.1161/CIRCULATIONAHA.104.473165. PMID 15956138.
- ↑ Horstkotte D, Niehues R, Strauer BE (1991). "Pathomorphological aspects, aetiology and natural history of acquired mitral valve stenosis". Eur Heart J. 12 Suppl B: 55–60. PMID 1936027.
- ↑ Chapter 1: Diseases of the Cardiovascular system > Section: Valvular Heart Disease in: Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 0-7817-7153-6.
- ↑ "Mitral Stenosis: Heart Valve Disorders: Merck Manual Home Edition". Retrieved 2009-03-14.
- ↑ Gordon SP, Douglas PS, Come PC, Manning WJ (1992). "Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up". J Am Coll Cardiol. 19 (5): 968–73. PMID 1552121.
- ↑ Sagie A, Freitas N, Padial LR, Leavitt M, Morris E, Weyman AE; et al. (1996). "Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease". J Am Coll Cardiol. 28 (2): 472–9. doi:10.1016/0735-1097(96)00153-2. PMID 8800128.
- ↑ Template:Cite doi
- ↑ ROWE JC, BLAND EF, SPRAGUE HB, WHITE PD (1960). "The course of mitral stenosis without surgery: ten- and twenty-year perspectives". Ann Intern Med. 52: 741–9. PMID 14439687.
- ↑ Dahl JC, Winchell P, Borden CW (1967). "Mitral stenosis. A long term postoperative follow-up". Arch Intern Med. 119 (1): 92–7. PMID 6015840.
- ↑ Roy SB, Gopinath N (1968). "Mitral stenosis". Circulation. 38 (1 Suppl): 68–76. PMID 4889600.
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ Tribouilloy CM, Enriquez-Sarano M, Schaff HV, Orszulak TA, Bailey KR, Tajik AJ; et al. (1999). "Impact of preoperative symptoms on survival after surgical correction of organic mitral regurgitation: rationale for optimizing surgical indications". Circulation. 99 (3): 400–5. PMID 9918527.
- ↑ Krayenbuehl HP (1986). "Surgery for mitral regurgitation. Repair versus valve replacement". Eur Heart J. 7 (8): 638–43. PMID 3769948.
- ↑ Enriquez-Sarano M, Schaff HV, Orszulak TA, Tajik AJ, Bailey KR, Frye RL (1995). "Valve repair improves the outcome of surgery for mitral regurgitation. A multivariate analysis". Circulation. 91 (4): 1022–8. PMID 7850937.
- ↑ Lee EM, Shapiro LM, Wells FC (1997). "Superiority of mitral valve repair in surgery for degenerative mitral regurgitation". Eur Heart J. 18 (4): 655–63. PMID 9129898.
- ↑ Mohty D, Orszulak TA, Schaff HV, Avierinos JF, Tajik JA, Enriquez-Sarano M (2001). "Very long-term survival and durability of mitral valve repair for mitral valve prolapse". Circulation. 104 (12 Suppl 1): I1–I7. PMID 11568020.
- ↑ Thourani VH, Weintraub WS, Guyton RA, Jones EL, Williams WH, Elkabbani S; et al. (2003). "Outcomes and long-term survival for patients undergoing mitral valve repair versus replacement: effect of age and concomitant coronary artery bypass grafting". Circulation. 108 (3): 298–304. doi:10.1161/01.CIR.0000079169.15862.13. PMID 12835220.
- ↑ Hammermeister KE, Sethi GK, Henderson WG, Oprian C, Kim T, Rahimtoola S (1993). "A comparison of outcomes in men 11 years after heart-valve replacement with a mechanical valve or bioprosthesis. Veterans Affairs Cooperative Study on Valvular Heart Disease". N Engl J Med. 328 (18): 1289–96. doi:10.1056/NEJM199305063281801. PMID 8469251.
- ↑ Hammermeister K, Sethi GK, Henderson WG, Grover FL, Oprian C, Rahimtoola SH (2000). "Outcomes 15 years after valve replacement with a mechanical versus a bioprosthetic valve: final report of the Veterans Affairs randomized trial". J Am Coll Cardiol. 36 (4): 1152–8. PMID 11028464.