Mitral stenosis echocardiography
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
In most cases, the diagnosis of mitral stenosis is most easily made by echocardiography, which shows decreased opening of the mitral valve leaflets, and increased blood flow velocity during diastole. The trans-mitral gradient as measured by Doppler echocardiography is the gold standard in the evaluation of the severity of mitral stenosis.
Echocardiographic Assessment
- Echocardiography is the standard and by using various techniques the transmitral flows can be converted to valve areas.
- The mitral valve area can be directly planimetered in some cases.
- Echocardiographic findings also predict the success/failure of balloon valvuloplasty.
- Coexisting valve dysfunction can be identified as well as pulmonary hypertension and right ventricular dysfunction.
- Cardiac catheterization is a secondary modality used when surgical/percutaneous repair is contemplated or if symptoms are out of proportion to noninvasive testing results.
Mitral valve assessment with echocardiography should include:
- Diagnosis from the pattern of valve involvement and calcification.
- severity of mitral stenosis
- Associated mitral regurgitation
- Other co-existent valve lesions
- Chamber dilatation and function
Complete echocardiographic examination of mitral valve include M-mode tracing, multiple two dimensional views, and Doppler flow evaluation.
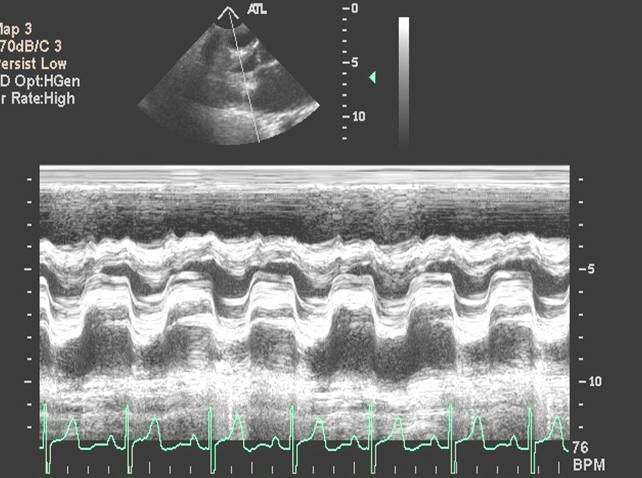
M-mode echocardiography
M-mode echocardiographic assessment of the valve reveals slow early diastolic closure of the mitral valve. The mid-diastolic closure velocity or E-F slope is remarkably reduced or sometimes even flat. Though least reliable, this can be used to assess the severity of the mitral stenosis and to determine re-stenosis from serial measurements after surgical or percutaneous treatment. E-F slope of less than 10 mm/sec (normal is >60 mm/sec) recoded during suspended respiration suggests severe mitral stenosis. E-F slope can also be flat in subjects with normal mitral valve if the left ventricular compliance is reduced.
Another M-mode feature of mitral stenosis is the anterior movement of posterior mitral valve leaflet in early diastole. Opening snap usually coincides with E point.
The images below show decreased E-F slope

2D-Echocardiography
This is a reliable method of assessing the severity of stenosis.[1][2] As with any stenotic valve, the main diagnostic feature in the parasternal long axis view is the doming of the entire valve into ventricle during diastole. This is due to the reduced mobility of the valve tips compared to the base of the leaflets leading to development of persistent left atrio-ventricular(AV) gradient. With this orientation, maximum opening area of mitral valve during diastole can be measured by direct planimetry of the two dimensional image. Valve orifice area of <1 cm2 is considered severe.
During atrial contraction when the AV gradient increases, the valves open abruptly producing opening snap and a knee bend appearance on the precordial long axis view
Thickening of the valve leaflets with or without calcification can be visualized with echocardiography. This can also involve the annulus and the chordae which can be shortened.
Other associated features may include markedly enlarged left atrium, pulmonary hypertension, right heart enlargement and tricuspid regurgitation. There may be involvement of other valves as well.
Orifice area by planimetry
- A well validated technique for assessing severity
- In parasternal short axis view
- The mitral valve is funnel shaped, so the area needs to be measured at the tip of the valves (the narrowest portion).
- Be sure to turn the gain down to have low overall 2D gain.
- Trace the inner edge of the valve orifice during the maximum opening in diastole.
- Not useful if heavily calcified valves or after valvotomy
- Sometimes chordae can mimic the valve orifice.
Echocardiogram below shows above mentioned knee bend with opening snap (Time 0:00-0:07), decreased E-F slope (Time 0:08-0:12), measurement of orifice area (Time 0:25-0:37) <youtube v=Jks98rwwsh8/>
Doppler echocardiography
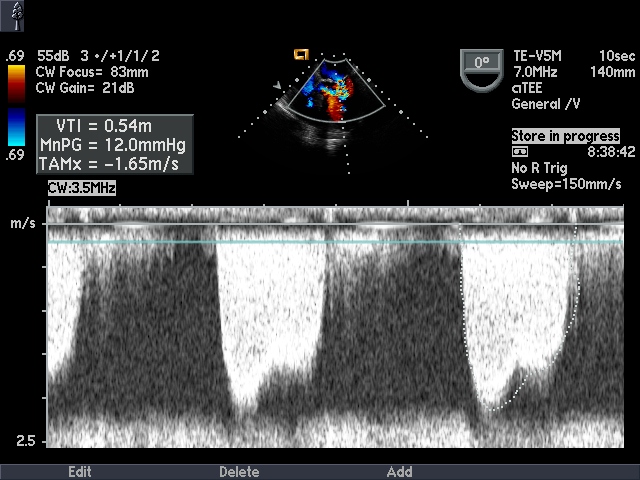
Mean transmitral valve gradient
Can be measured by tracing the area-under-the-curve of the mitral E and A waves obtained by continuous Doppler. The severity of stenosis can be assessed as mild (<5), moderate (5-10) and severe (>10). Peak transmitral gradient can be calculated from velocity of mitral inflow using modified Bernoulli equation:
Peak transmitral gradient= 4 x (peak velocity)2
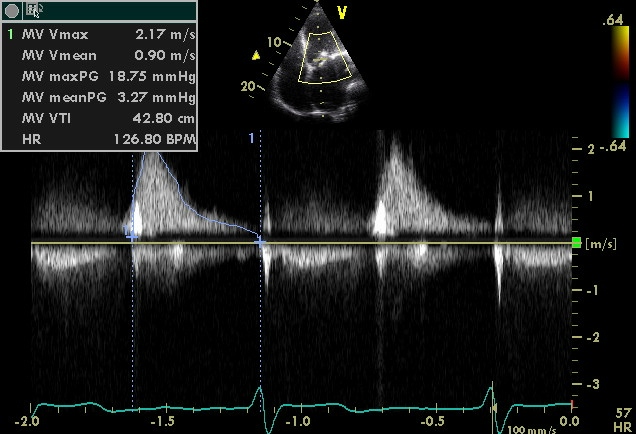
Pressure half time
The rate of pressure decline across the stenotic orifice is determined by the cross sectional area of the orifice. Smaller the orifice leads to slower rate of pressure decline.
Pressure half time is defined as the time interval between maximum early diastolic pressure gradient and the point at which the pressure gradient is half the maximum value.
By echocardiography, this is measured in apical-4-chamber view with continuous wave Doppler aligned with the inflow jet of mitral valve. The spectral trace is recorded and the slope of the flow is measured from the beginning of E-wave ignoring the A-wave.
Based on the Bernoulli equation, the velocity of pressure half time can be derived as V1/2 = 0.7 Vmax
The mitral valve area can be calculated as MV area (cm2) = 220 ÷ Pressure half time (msec)
Limitations of pressure half time
- Assumes normal left atrial and left ventricular compliance. This is not true immediately post valvuloplasty (72 hrs) and in left ventricular hypertrophy
- Aortic regurgitation leads to increased left ventricular diastolic pressure and thus shorter pressure half time. Hence Mitral valve area is over estimated.
- Angle needs constant intercept angle parallel to the flow
- Atrial fibrillation - several beats need to be averaged.
- Atrial septal defect - left to right shunt, shortened pressure half time and hence mitral valve area over estimated.
- Mitral regurgitation does not affect pressure half time.
Exercise Doppler echocardiography
2008 ACC/AHA guidelines recommend that when there is a discrepancy between resting Doppler echocardiographic findings, clinical findings, symptoms, and signs in a patient with MS, exercise doppler echocardiography should be performed.[3] In those who cannot exercise, dobutamine can be used to increase the heart rate.[4]
Continuity equation Mitral valve area[5]
Mitral valve area = (LVOT diameter)2 x 0.785 x TVILVOT
------------------------------------------
TVIMV
LVOT: Left Ventricular Outflow Tract
TVILVOT: Time Velocity Integral of Left Ventricular Outflow Tract
TVIMV: Time Velocity Integral of Mitral Valve
- Continuous Wave Doppler Echo
- 3-D Echo of Rheumatic Mitral Stenosis 1
<googlevideo>-3098493179966000395&hl=en</googlevideo>
- 3-D Echo of Rheumatic Mitral Stenosis 2
<googlevideo>-1233084670908574806&hl=en</googlevideo>
- 3-D Echo of Rheumatic Mitral Stenosis 3
<googlevideo>4388526645575160977&hl=en</googlevideo>
- Calcific Mitral Stenosis Continuous Wave Doppler
- Calcific Mitral Stenosis Severe 1
<googlevideo>-2694339846253882313&hl=en</googlevideo>
- Calcific Mitral Stenosis Severe 2
<googlevideo>-4939554452635824325&hl=en</googlevideo>
- Calcific Mitral Stenosis Severe 3
<googlevideo>-4939554452635824325&hl=en</googlevideo>
- Calcific Mitral Stenosis Severe 4
<googlevideo>9174885547972304289&hl=en</googlevideo>
- Calcific Mitral Stenosis Severe 5
<googlevideo>451524906007806928&hl=en</googlevideo>
References
- ↑ Wann LS, Weyman AE, Feigenbaum H, Dillon JC, Johnston KW, Eggleton RC (1978). "Determination of mitral valve area by cross-sectional echocardiography". Ann Intern Med. 88 (3): 337–41. PMID 629495.
- ↑ Nichol PM, Gilbert BW, Kisslo JA (1977). "Two-dimensional echocardiographic assessment of mitral stenosis". Circulation. 55 (1): 120–8. PMID 830199.
- ↑ Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Faxon DP, Freed MD; et al. (2008). "2008 Focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease): endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons". Circulation. 118 (15): e523–661. doi:10.1161/CIRCULATIONAHA.108.190748. PMID 18820172.
- ↑ Reis G, Motta MS, Barbosa MM, Esteves WA, Souza SF, Bocchi EA (2004). "Dobutamine stress echocardiography for noninvasive assessment and risk stratification of patients with rheumatic mitral stenosis". J Am Coll Cardiol. 43 (3): 393–401. doi:10.1016/j.jacc.2003.09.037. PMID 15013120.
- ↑ Oh J., Seward J.B., Tajik A.J.: The echo manual. 2nd ed. Lippincott-RavenPhiladelphia1999