Metronidazole (vaginal)
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Adeel Jamil, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Metronidazole (vaginal) is an anti-infective agent, antiparasitic and antiprotozoal agent that is FDA approved for the treatment of bacterial vaginosis (formerly referred to as Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis) in non-pregnant women. Common adverse reactions include fungal infection, headache, pruritus, abdominal pain, nausea, dysmenorrhea, pharyngitis, rash, infection, diarrhea, breast pain, and metrorrhagia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- VANDAZOLE is indicated in the treatment of bacterial vaginosis (formerly referred to as Haemophilus vaginitis, Gardnerella vaginitis, nonspecific vaginitis, Corynebacterium vaginitis, or anaerobic vaginosis) in non-pregnant women.
Dosing Information
- The recommended dose is one applicator full of VANDAZOLE , (approximately 5 grams of gel containing approximately 37.5 mg of metronidazole) administered intravaginally once a day for 5 days. For once a day dosing, VANDAZOLE should be administered at bedtime.
- Not for ophthalmic, dermal, or oral use.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Metronidazole (vaginal) in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Metronidazole (vaginal) in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Metronidazole (vaginal) FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Metronidazole (vaginal) in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Metronidazole (vaginal) in pediatric patients.
Contraindications
Hypersensitivity
- The use of VANDAZOLE is contraindicated in patients with a history of hypersensitivity to metronidazole, other nitroimidazole derivatives, or parabens. Reported reactions include urticaria; erythematous rash; Stevens-Johnson Syndrome, toxic epidermal necrolysis, flushing; nasal congestion; dryness of the mouth, vagina, or vulva; fever; pruritus; fleeting joint pains.
Psychotic Reaction with Disulfiram
- Use of oral metronidazole is associated with psychotic reactions in alcoholic patients who were using disulfiram concurrently. Do not administer VANDAZOLE to patients who have taken disulfiram within the last two weeks [see Adverse Reactions (6.2)].
Interaction with Alcohol
- Use of oral metronidazole is associated with a disulfiram-like reaction to alcohol, including abdominal cramps, nausea, vomiting, headaches, and flushing [see Adverse Reactions (6.2)]. Discontinue alcohol consumption during and for at least three days after therapy with VANDAZOLE.
Warnings
Central and Peripheral Nervous System Effects
- Use of oral or intravenous metronidazole is associated with convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or parethesia of an extremity [see Adverse Reactions (6.2)]. VANDAZOLE should be administered with caution to patients with central nervous system diseases. Discontinue VANDAZOLE promptly if a patient develops abnormal neurologic signs.
Carcinogenicity in Animals=
- Metronidazole has been shown to be carcinogenic in mice and rats [see Carcinogenesis, Mutagenesis, Impairment of Fertility (13.1)]. Unnecessary use of metronidazole should be avoided. Use of VANDAZOLE should be reserved for the treatment of bacterial vaginosis [see Indications and Usage (1)]
Interference with Laboratory Tests
- Metronidazole may interfere with certain types of determinations of serum chemistry values, such as aspartate aminotransferase (AST, SGOT), alanine aminostransferase (ALT, SGPT), lactate dehydrogenase (LDH), triglycerides, and glucose hexokinase. Values of zero may be observed. All of the assays in which interference has been reported involve enzymatic coupling of the assay to oxidation-reduction of nicotinamide-adenine dinucleotides (NAD + NADH). Interference is due to the similarity in absorbance peaks of NADH (340 nm) and metronidazole (322 nm) at pH 7. Consider postponing chemistry laboratory tests to after treatment with VANDAZOLE.
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
- The data described below reflect exposure to VANDAZOLE compared to another formulation of vaginal metronidazole in 220 women in a single trial. The population was non-pregnant females (age range 18 to 72 years, the mean was 33 years +/- 11 years) with bacterial vaginosis. The racial demographic of those enrolled was 71 (32%) of White, 143 (65%) of Black, 3 (1%) of Hispanic, 2 (1%) of Asian, and 1 (0%) of other. Patients administered an applicator full of VANDAZOLE intravaginally once daily at bedtime for 5 days.
- There were no deaths or serious adverse reactions related to drug therapy in the clinical trial. VANDAZOLE was discontinued in 5 patients (2.3%) due to adverse reactions.
- The incidence of all adverse reactions in VANDAZOLE-treated patients was 42% (92/220). Adverse reactions occurring in ≥ 1% of patients were: fungal infection* (12%), headache (7%), pruritus (6%), abdominal pain (5%), nausea (3%), dysmenorrhea (3%), pharyngitis (2%), rash (1%), infection (1%), diarrhea (1%), breast pain (1%), and metrorrhagia (1%).
- Known or previously unrecognized vaginal candidiasis may present more prominent symptoms during therapy with VANDAZOLE. Approximately 10% of patients treated with VANDAZOLE developed Candida vaginitis during or immediately after therapy.
- Additional uncommon events, reported by < 1% of those women treated with VANDAZOLE included:

Other Metronidazole Formulations
Other Vaginal Formulations
- Other reactions that have been reported in association with the use of other formulations of metronidazole vaginal gel include: unusual taste and decreased appetite.
Topical (Dermal) Formulations
- Other reactions that have been reported in association with the use of topical (dermal) formulations of metronidazole include skin irritation, transient skin erythema, and mild skin dryness and burning. None of these adverse reactions exceeded an incidence of 2% of patients.
Oral and Parenteral Formulations
- The following adverse reactions and altered laboratory tests have been reported with the oral or parenteral use of metronidazole:
Cardiovascular:
- Flattening of the T-wave may be seen in electrocardiographic tracings.
Nervous System:
- The most serious adverse reactions reported in patients treated with metronidazole have been convulsive seizures, encephalopathy, aseptic meningitis, optic and peripheral neuropathy, the latter characterized mainly by numbness or paresthesia of an extremity. In addition, patients have reported syncope, vertigo, incoordination, ataxia, confusion, dysarthria, irritability, depression, weakness, and insomnia. [see Warnings and Precautions (5.1)]
Gastrointestinal:
- Abdominal discomfort, nausea, vomiting, diarrhea, an unpleasant metallic taste, anorexia, epigastric distress, abdominal cramping, constipation, “furry” tongue, glossitis, stomatitis, pancreatitis, and modification of taste of alcoholic beverages.
Genitourinary:
- Overgrowth of Candida in the vagina, dyspareunia, decreased libido, proctitis.
Hematopoietic:
- Reversible neutropenia, reversible thrombocytopenia.
Hypersensitivity Reactions:
- Urticaria; erythematous rash; Stevens-Johnson Syndrome, toxic epidermal necrolysis, flushing; nasal congestion; dryness of the mouth, vagina, or vulva; fever; pruritus; fleeting joint pains.
Renal:
- Dysuria, cystitis, polyuria, incontinence, a sense of pelvic pressure, darkened urine.
Postmarketing Experience
There is limited information regarding Metronidazole (vaginal) Postmarketing Experience in the drug label.
Drug Interactions
- The intravaginal administration of a single 5 gram dose of VANDAZOLE results in relatively lower mean systemic exposure to metronidazole that is approximately 2% to 5% of that achieved following a 500 mg oral dose of metronidazole [see Clinical Pharmacology (12.3)]. The following drug interactions were reported for oral metronidazole.
Disulfiram
- Use of oral metronidazole has been associated with psychotic reactions in alcoholic patients who are using disulfiram concurrently. VANDAZOLE should not be used by patients who have taken disulfiram within the last two weeks [see Contraindications (4.2)].
Alcoholic Beverages
- Use of oral metronidazole has been associated with a disulfiram-like reaction (abdominal cramps, nausea, vomiting, headaches, and flushing) to alcohol. Alcoholic beverages and preparations containing ethanol or propylene glycol should not be consumed during and for at least three days after VANDAZOLE therapy [see Contraindications (4.3)].
Coumarin and Other Oral Anticoagulants
- Use of oral metronidazole has been reported to potentiate the anticoagulant effect of warfarin and other coumarin anticoagulants, resulting in a prolongation of prothrombin time. This possible drug interaction should be considered when VANDAZOLE is prescribed for patients on this type of anticoagulant therapy. In patients on oral anticoagulants, consider monitoring prothrombin time, international normalized ratio (INR), and other coagulation parameters while on VANDAZOLE.
Lithium
- Short-term use of oral metronidazole has been associated with elevation of serum lithium concentrations and, in a few cases signs of lithium toxicity, in patients stabilized on relatively high doses of lithium. Use VANDAZOLE with caution in patients treated with lithium and consider monitoring lithium serum concentrations while on VANDAZOLE.
Cimetidine
- Use of oral metronidazole with cimetidine may prolong the half-life and decrease plasma clearance of metronidazole. No dose adjustment of VANDAZOLE is necessary.
Use in Specific Populations
Pregnancy
- VANDAZOLE should be used during pregnancy only if clearly needed. There are no adequate and well-controlled studies in pregnant women.
- There are published data from case-control studies, cohort studies, and two meta-analyses that include more than 5000 pregnant women who used metronidazole systemically during pregnancy. Many studies included first trimester exposures. One study showed an increased risk of cleft lip, with or without cleft palate, in infants exposed to metronidazole in-utero; however, these findings were not confirmed. In addition, more than ten randomized, placebo-controlled clinical trials enrolled more than 5000 pregnant women to assess the use of systemic antibiotic treatment (including metronidazole) for bacterial vaginosis on the incidence of preterm delivery. Most studies did not show an increased risk for congenital anomalies or other adverse fetal outcomes following metronidazole exposure during pregnancy. Three studies conducted to assess the risk of infant cancer following systemic metronidazole exposure during pregnancy did not show an increased risk; however, the ability of these studies to detect such a signal was limited.
- Oral reproductive toxicity studies have been performed in mice at doses up to six times the recommended human dose based on body surface area comparisons and have revealed no evidence of impaired fertility or harm to the fetus. However, in a single small study where the drug was administered intraperitoneally, some intrauterine deaths were observed.
- Animal studies have shown that metronidazole crosses the placental barrier and enters the fetal circulation rapidly. Because animal reproduction studies are not always predictive of human response, and because metronidazole crosses the placental barrier and is a carcinogen in rodents, this drug should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Metronidazole (vaginal) in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Metronidazole (vaginal) during labor and delivery.
Nursing Mothers
- Caution should be exercised when VANDAZOLE is administered to a nursing woman. Following oral metronidazole administration, concentrations of metronidazole in human milk are similar to concentrations in plasma. Since some metronidazole is systemically absorbed following vaginal administration of metronidazole, excretion in human milk is possible.
- Because of the potential for tumorigenicity shown for metronidazole in animal studies, a decision should be made whether to discontinue nursing or to discontinue VANDAZOLE, taking into account the importance of the therapy to the mother. A nursing mother may choose to pump and discard her milk for the duration of VANDAZOLE therapy, and for 24 hours after therapy ends and feed her infant stored human milk or formula.
Pediatric Use
- The safety and efficacy of VANDAZOLE in the treatment of bacterial vaginosis in post-menarchal females have been established on the extrapolation of clinical trial data from adult women. The safety and efficacy of VANDAZOLE in pre-menarchal females have not been established.
Geriatic Use
- Clinical studies with VANDAZOLE did not include sufficient numbers of subjects 65 years of age or older to determine whether they respond differently than younger subjects. Other reported clinical experience in using metronidazole gel, 1% has not identified differences in responses between elderly and younger patients.
Gender
There is no FDA guidance on the use of Metronidazole (vaginal) with respect to specific gender populations.
Race
There is no FDA guidance on the use of Metronidazole (vaginal) with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Metronidazole (vaginal) in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Metronidazole (vaginal) in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Metronidazole (vaginal) in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Metronidazole (vaginal) in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Metronidazole (vaginal) Administration in the drug label.
Monitoring
There is limited information regarding Metronidazole (vaginal) Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Metronidazole (vaginal) and IV administrations.
Overdosage
- There is no human experience with overdosage of metronidazole vaginal gel. Vaginally applied metronidazole gel, 0.75% could be absorbed in sufficient amounts to produce systemic effects
Pharmacology
Mechanism of Action
- The intracellular targets of action of metronidazole on anaerobes are largely unknown. The 5-nitro group of metronidazole is reduced by metabolically active anaerobes, and studies have demonstrated that the reduced form of the drug interacts with bacterial DNA. However, it is not clear whether interaction with DNA alone is an important component in the bactericidal action of metronidazole on anaerobic organisms.
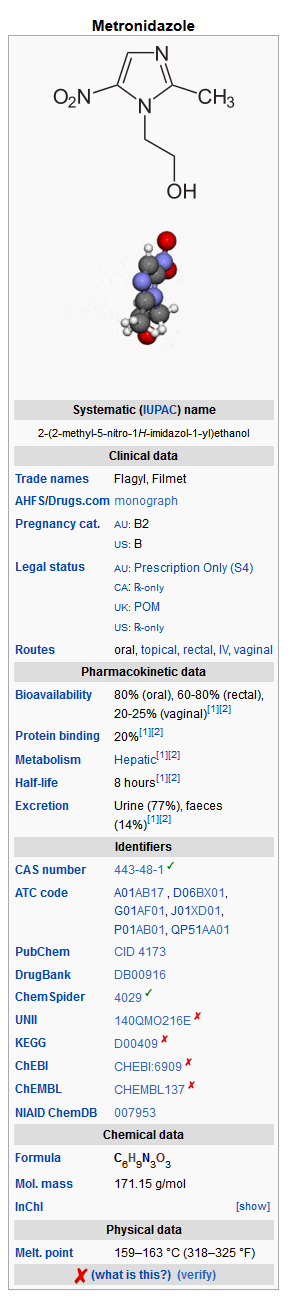
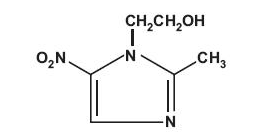
Structure
- VANDAZOLE (metronidazole vaginal gel, 0.75%) is the vaginal dosage form of the nitroimidazole antimicrobial metronidazole at a concentration of 0.75%. Chemically, metronidazole is a 2-methyl-5-nitroimidazole-1-ethanol.
- VANDAZOLE is a colorless to yellow gel, containing metronidazole at a concentration of 7.5 mg/g (0.75%). The gel also contains edetate disodium, hypromellose, methylparaben, propylene glycol, propylparaben, purified water, and sodium hydroxide (to adjust pH).
- Each applicator full of 5 grams of vaginal gel contains approximately 37.5 mg of metronidazole.
Pharmacodynamics
Microbiology
Activity In Vitro
- Metronidazole is an antibacterial agent active in vitro against most strains of the following organisms that have been reported to be associated with bacterial vaginosis:
- Bacteroides spp.
- Gardnerella vaginalis
- Mobiluncus spp.
- Peptostreptococcus spp.
- Standard methodology for the susceptibility testing of the potential bacterial vaginosis pathogens, Gardnerella vaginalis and Mobiluncus spp., has not been defined. Culture and sensitivity testing of bacteria are not routinely performed to establish the diagnosis of bacterial vaginosis.
Pharmacokinetics
Healthy Subjects
- Following a single, intravaginal 5 gram dose of metronidazole vaginal gel (equivalent to 37.5 mg of metronidazole) to 38 healthy female subjects, a mean maximum serum metronidazole concentration of 281 ng/mL was reported (range: 134 to 464 ng/mL). The average time to achieve this Cmax was 9.5 hours (range: 4 to 17 hours) after dosing with metronidazole vaginal gel. This Cmax is approximately 2% of the mean maximum serum concentration reported in healthy subjects administered a single, oral 500 mg dose of metronidazole (mean Cmax = 12,785 ng/mL).
- The extent of exposure [area under the curve (AUC)] of metronidazole, when administered as a single intravaginal 5 gram dose of metronidazole vaginal gel (equivalent to 37.5 mg of metronidazole), was 5,989 ng•hr/mL (range: 2,797 to 10,515 ng•hr/mL). This AUC0-∞ is approximately 5% of the reported AUC of metronidazole following a single oral 500 mg dose of metronidazole approximately 125,000 ng•hr/mL.
Patients with Bacterial Vaginosis
- Following single and multiple 5 gram doses of a similar metronidazole vaginal gel product to 4 patients with bacterial vaginosis, a mean maximum serum metronidazole concentration of 214 ng/mL on day one and 294 ng/mL (range: 228 to 349 ng/mL) on day five were reported. Steady state metronidazole serum concentrations following oral dosages of 400 to 500 mg BID have been reported to range from 6,000 to 20,000 ng/mL.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
- Metronidazole has shown evidence of carcinogenic activity after chronic oral administration in mice and rats. Pulmonary tumors and lymphomas were reported in several oral mouse studies in which mice were dosed at 75 mg/kg and above (about 5 times the clinical human dose based on body surface area comparison). Malignant liver tumors were reported in male mice dosed at doses equivalent to a human dose of 41 mg/kg/day (33 times the recommended clinical dose based on body surface area comparisons). Chronic oral dosing of metronidazole in rats at doses above 150 mg/kg (about 20 times the clinical human dose based on body surface area comparison) has resulted in mammary and hepatic tumors. Two lifetime tumorigenicity studies in hamsters have been performed and reported to be negative. Although no life-time studies were performed to evaluate the carcinogenic potential of VANDAZOLE (metronidazole vaginal gel, 0.75%), published data have shown that intravaginal administration of metronidazole to Wistar rats for 5 days, at doses 26 times the recommended human dose based on body surface area comparisons, has resulted in an increased frequency of micronuclei in rat vaginal mucosal cells.
- Metronidazole has shown mutagenic activity in a number of in vitro assay systems. In addition, a dose dependent increase in the frequency of micronuclei was observed in mice after intraperitoneal injections. An increase in chromosome aberrations has been reported in one study of patients with Crohn’s disease who were treated with 200 to 1200 mg/day of metronidazole for 1 to 24 months. However, in a second study, no increase in chromosome aberrations was reported in patients with Crohn’s disease who were treated with metronidazole for 8 months.
- Fertility studies have been performed in mice up to six times the recommended human oral dose (based on mg/m2) and have revealed no evidence of impaired fertility.
Clinical Studies
- A single, randomized, double-blind, active-controlled clinical trial was conducted to evaluate the efficacy of VANDAZOLE for the treatment of bacterial vaginosis. A clinical diagnosis of bacterial vaginosis was defined by the presence of a homogeneous vaginal discharge that (a) has a pH of greater than 4.5, (b) emits a "fishy" amine odor when mixed with a 10% KOH solution, and (c) contains clue cells on microscopic examination. Gram's stain results consistent with a diagnosis of bacterial vaginosis include (a) markedly reduced or absent Lactobacillus morphology, (b) predominance of Gardnerella morphotype, and (c) absent or few white blood cells. Non-pregnant females at least 18 years of age were randomized to receive treatment with either VANDAZOLE or another formulation of metronidazole vaginal gel 0.75% once daily at bedtime for 5 days. The modified intent-to treat population (patients who received study medication and had a Nugent score ≥ 4) consisted of 229 VANDAZOLE patients and 243 patients treated with another vaginal formulation of metronidazole. Therapeutic Cure defined as a clinical cure and Nugent score < 4 was assessed Day 22-31. Table 1 shows the therapeutic, clinical and Nugent score cure rates in this trial. The therapeutic cure rate was 42.8% for the VANDAZOLE group and 30.9% for the comparator group (95% confidence interval about the 11.9% difference in therapeutic cure rate: 2.8% to 21.0%).

How Supplied
VANDAZOLE (metronidazole vaginal gel, 0.75%) is supplied in a 70 gram tube and packaged with 5 vaginal applicators.
Storage
- Store at 20o to 25oC (68o to 77oF).
- Avoid exposure to extreme heat or cold.
- Protect from freezing.
Images
Drug Images
{{#ask: Page Name::Metronidazole (vaginal) |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
PRINCIPAL DISPLAY PANEL, PART 1 OF 2

PRINCIPAL DISPLAY PANEL, PART 2 OF 2

Vandazole (Metronidazole Vaginal Gel, 0.75%) 70 grams Tube, Carton Text NDC 0245-0860-70
VANDAZOLE®
(Metronidazole Vaginal Gel, 0.75%)
with 5 applicators
FOR INTRAVAGINAL USE ONLY.
(NOT FOR OPHTHALMIC, DERMAL, OR ORAL USE.)
Rx only
Net Wt. 70 grams
UPSHER-SMITH




{{#ask: Label Page::Metronidazole (vaginal) |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Interaction with Alcohol
- Instruct the patient not to consume alcoholic beverages and preparations containing ethanol or propylene glycol during and for at least 3 days after treatment with VANDAZOLE.
Drug Interactions
- Instruct the patient not to use VANDAZOLE if disulfiram had been used within the last two weeks [see Contraindications (4.2)], and to inform their healthcare provider if they are taking oral anticoagulants, or lithium.
Vaginal Intercourse and Use with Vaginal Products
- Instruct the patient not to engage in vaginal intercourse, or use other vaginal products (such as tampons or douches) during treatment with VANDAZOLE.
Fungal Vaginal Infections
- Inform the patient that vaginal fungal infections can occur following use of VANDAZOLE and may require treatment with an antifungal drug [see Adverse Reactions (6.1)].
Human Milk Feeding
- Advise women that they may consider discontinuing milk feeding or pump and discard their milk during treatment and for 24 hours after the last dose of VANDAZOLE.
Accidental Exposure to the Eye
- Inform the patient that VANDAZOLE contains ingredients that may cause burning and irritation of the eye. In the event of accidental contact with the eye, rinse the eye with copious amounts of cool tap water and consult a healthcare provider.
Vaginal Irritation
- Inform the patient to discontinue use and consult a healthcare provider if vaginal irritation occurs with use of VANDAZOLE.
Administration of Drug
- Instruct the patient that VANDAZOLE (metronidazole vaginal gel, 0.75%) is supplied with 5 vaginal applicators. For once daily dosing, one applicator should be used per dose. See DIRECTIONS FOR USE for complete instructions on how to use the product and the vaginal applicator.
US Patent No. 7,456,207
Manufactured For:
UPSHER-SMITH LABORATORIES, INC.
Minneapolis, MN 55447
Rev. F 1/2011
Precautions with Alcohol
Alcohol-Metronidazole (vaginal) interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- VANDAZOLE®
Look-Alike Drug Names
There is limited information regarding Metronidazole (vaginal) Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.