Melanoma physical examination
Jump to navigation
Jump to search
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: : Yazan Daaboul, M.D., Serge Korjian M.D., Jesus Rosario Hernandez, M.D. [2].
|
Melanoma Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Melanoma physical examination On the Web |
|
American Roentgen Ray Society Images of Melanoma physical examination |
|
Risk calculators and risk factors for Melanoma physical examination |
Overview
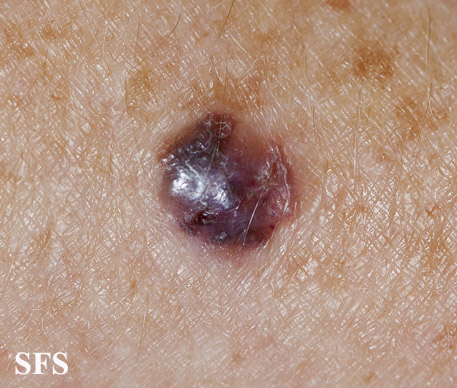
Physical examination findings suggestive of malignant melanoma include ABCDE: Asymmetry of the lesion, Border irregularity, Color change, large Diameter, and Evolution over time.
Physical Examination
Skin
- Although melanoma can occur anywhere, melanoma among women occurs more commonly on the extremities, and among men it occurs more commonly on the trunk or head and neck.
- Patients with suspected melanoma should have a full-body examination for other lesions.
- On physical examination, the ABCDE for distinguishing benign nevi from malignant melanoma are:
- Other signs in a nevus that would suggest a malignant change include the following:
- Development of satellites
- Ulceration or bleeding (late signs)[3][4][5]
- Any suggestive findings detected on physical exam warrant a complete excisional biopsy. To view the complete approach for a suspected melanoma, click here.
Gallery
HEENT
Extremities
Genitales
References
- ↑ Lee H, Kwon K (March 2017). "A mathematical analysis of the ABCD criteria for diagnosing malignant melanoma". Phys Med Biol. 62 (5): 1865–1884. doi:10.1088/1361-6560/aa562f. PMID 28036304.
- ↑ Tsao H, Olazagasti JM, Cordoro KM, Brewer JD, Taylor SC, Bordeaux JS, Chren MM, Sober AJ, Tegeler C, Bhushan R, Begolka WS (April 2015). "Early detection of melanoma: reviewing the ABCDEs". J. Am. Acad. Dermatol. 72 (4): 717–23. doi:10.1016/j.jaad.2015.01.025. PMID 25698455.
- ↑ Bønnelykke-Behrndtz ML, Schmidt H, Christensen IJ, Damsgaard TE, Møller HJ, Bastholt L, Nørgaard PH, Steiniche T (December 2014). "Prognostic stratification of ulcerated melanoma: not only the extent matters". Am. J. Clin. Pathol. 142 (6): 845–56. doi:10.1309/AJCPW56PHGLFTKZC. PMID 25389339.
- ↑ Callender GG, McMasters KM (2011). "What does ulceration of a melanoma mean for prognosis?". Adv Surg. 45: 225–36. PMID 21954690.
- ↑ Tromme I, Sacré L, Hammouch F, Richez P, Degryse JM, Speybroeck N (December 2018). "Melanoma diagnosis: predictive value of macroscopic changes observed by the patient". Melanoma Res. 28 (6): 611–617. doi:10.1097/CMR.0000000000000496. PMID 30192302.