Malaria history and symptoms: Difference between revisions
(Created page with "'''For patient information click here''' {{CMG}} {{Malaria}} ==Overview== '''Malaria''' is a vector-borne [[infectiou...") |
No edit summary |
||
| Line 1: | Line 1: | ||
'''Malaria''' is a [[Vector (biology)|vector]]-borne [[infectious disease]] caused by [[protozoan]] [[parasite]]s. It is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, it causes disease in approximately 650 million people and kills between one and three million, most of them young children in Sub-Saharan Africa. Malaria is commonly associated with poverty, but is also a cause of poverty and a major hindrance to economic development. | '''Malaria''' is a [[Vector (biology)|vector]]-borne [[infectious disease]] caused by [[protozoan]] [[parasite]]s. It is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, it causes disease in approximately 650 million people and kills between one and three million, most of them young children in Sub-Saharan Africa. Malaria is commonly associated with poverty, but is also a cause of poverty and a major hindrance to economic development. | ||
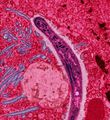
[[Image:Malaria.jpg|thumb|left|250px|A ''Plasmodium'' sporozoite traverses the cytoplasm of a mosquito midgut epithelial cell in this false-color [[electron micrograph]].]] | [[Image:Malaria.jpg|thumb|left|250px|A ''Plasmodium'' sporozoite traverses the cytoplasm of a mosquito midgut epithelial cell in this false-color [[electron micrograph]].]] | ||
Symptoms of malaria include [[fever]], [[shivering]], [[arthralgia]] (joint pain), [[vomiting]], [[anemia]] caused by [[hemolysis]], [[hemoglobinuria]], and [[convulsion]]s. There may be the feeling of tingling in the skin, particularly with malaria caused by ''P. falciparum''. The classical symptom of malaria is cyclical occurrence of sudden coldness followed by rigor and then fever and sweating lasting four to six hours, occurring every two days in ''P. vivax'' and ''P. ovale'' infections, while every three for ''P. malariae''.<ref name=RBMarmenia>[http://www.malaria.am/eng/pathogenesis.php Malaria life cycle & pathogenesis]. Malaria in Armenia. Accessed October 31, 2006.</ref> ''P. falciparum'' can have recurrent fever every 36-48 hours or a less pronounced and almost continuous fever. For reasons that are poorly understood, but which may be related to high [[intracranial pressure]], children with malaria frequently exhibit [[abnormal posturing]], a sign indicating severe brain damage.<ref name="Idro ">{{cite journal | last =Idro | first =R | authorlink = | coauthors =Otieno G, White S, Kahindi A, Fegan G, Ogutu B, Mithwani S, Maitland K, Neville BG, Newton CR | title = Decorticate, decerebrate and opisthotonic posturing and seizures in Kenyan children with cerebral malaria| journal =Malaria Journal | volume =4 | issue =57 | pages = | publisher = | date = | url =http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16336645 | doi = | id =PMID 16336645 | accessdate =2007-01-21 }} </ref> Malaria has been found to cause cognitive impairments, especially in children. It causes widespread [[anemia]] during a period of rapid brain development and also direct brain damage. This neurologic damage results from cerebral malaria to which children are more vulnerable.<ref>Boivin, M.J., "[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12394524&dopt=Citation Effects of early cerebral malaria on cognitive ability in Senegalese children]," ''Journal of Developmental and Behavioral Pediatrics'' 23, no. 5 (October 2002): 353–64. Holding, P.A. and Snow, R.W., "[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11425179&dopt=Citation Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence]," ''American Journal of Tropical Medicine and Hygiene'' 64, suppl. nos. 1–2 (January–February 2001): 68–75.</ref> | Symptoms of malaria include [[fever]], [[shivering]], [[arthralgia]] (joint pain), [[vomiting]], [[anemia]] caused by [[hemolysis]], [[hemoglobinuria]], and [[convulsion]]s. There may be the feeling of tingling in the skin, particularly with malaria caused by ''P. falciparum''. The classical symptom of malaria is cyclical occurrence of sudden coldness followed by rigor and then fever and sweating lasting four to six hours, occurring every two days in ''P. vivax'' and ''P. ovale'' infections, while every three for ''P. malariae''.<ref name=RBMarmenia>[http://www.malaria.am/eng/pathogenesis.php Malaria life cycle & pathogenesis]. Malaria in Armenia. Accessed October 31, 2006.</ref> ''P. falciparum'' can have recurrent fever every 36-48 hours or a less pronounced and almost continuous fever. For reasons that are poorly understood, but which may be related to high [[intracranial pressure]], children with malaria frequently exhibit [[abnormal posturing]], a sign indicating severe brain damage.<ref name="Idro ">{{cite journal | last =Idro | first =R | authorlink = | coauthors =Otieno G, White S, Kahindi A, Fegan G, Ogutu B, Mithwani S, Maitland K, Neville BG, Newton CR | title = Decorticate, decerebrate and opisthotonic posturing and seizures in Kenyan children with cerebral malaria| journal =Malaria Journal | volume =4 | issue =57 | pages = | publisher = | date = | url =http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16336645 | doi = | id =PMID 16336645 | accessdate =2007-01-21 }} </ref> Malaria has been found to cause cognitive impairments, especially in children. It causes widespread [[anemia]] during a period of rapid brain development and also direct brain damage. This neurologic damage results from cerebral malaria to which children are more vulnerable.<ref>Boivin, M.J., "[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=12394524&dopt=Citation Effects of early cerebral malaria on cognitive ability in Senegalese children]," ''Journal of Developmental and Behavioral Pediatrics'' 23, no. 5 (October 2002): 353–64. Holding, P.A. and Snow, R.W., "[http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=11425179&dopt=Citation Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence]," ''American Journal of Tropical Medicine and Hygiene'' 64, suppl. nos. 1–2 (January–February 2001): 68–75.</ref> | ||
{{#widget:SchemaSnippet}} | |||
Severe malaria is almost exclusively caused by ''P. falciparum'' infection and usually arises 6-14 days after infection.<ref name=Trampuz>{{cite journal | author = Trampuz A, Jereb M, Muzlovic I, Prabhu R | title = Clinical review: Severe malaria. | url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=12930555 | journal = Crit Care | volume = 7 | issue = 4 | pages = 315-23 | year = 2003 | id = PMID 12930555}}</ref> Consequences of severe malaria include [[coma]] and death if untreated—young children and pregnant women are especially vulnerable. [[Splenomegaly]] (enlarged spleen), severe [[headache]], cerebral [[ischemia]], [[hepatomegaly]] (enlarged liver), [[hypoglycemia]], and hemoglobinuria with [[renal failure]] may occur. Renal failure may cause [[blackwater fever]], where hemoglobin from lysed red blood cells leaks into the urine. Severe malaria can progress extremely rapidly and cause death within hours or days.<ref name=Trampuz/> In the most severe cases of the disease fatality rates can exceed 20%, even with intensive care and treatment.<ref>{{cite journal | author = Kain K, Harrington M, Tennyson S, Keystone J | title = Imported malaria: prospective analysis of problems in diagnosis and management. | journal = Clin Infect Dis | volume = 27 | issue = 1 | pages = 142-9 | year = 1998 | id = PMID 9675468}}</ref> In endemic areas, treatment is often less satisfactory and the overall fatality rate for all cases of malaria can be as high as one in ten.<ref>{{cite journal | author = Mockenhaupt F, Ehrhardt S, Burkhardt J, Bosomtwe S, Laryea S, Anemana S, Otchwemah R, Cramer J, Dietz E, Gellert S, Bienzle U | title = Manifestation and outcome of severe malaria in children in northern Ghana. | journal = Am J Trop Med Hyg | volume = 71 | issue = 2 | pages = 167-72 | year = 2004 | id = PMID 15306705}}</ref> Over the longer term, developmental impairments have been documented in children who have suffered episodes of severe malaria.<ref name="carter2005">{{cite journal | author=Carter JA, Ross AJ, Neville BG, Obiero E, Katana K, Mung'ala-Odera V, Lees JA, Newton CR | title=Developmental impairments following severe falciparum malaria in children | journal=Trop Med Int Health | year=2005 | volume=10 | pages=3-10 | id=PMID 15655008}}</ref> | Severe malaria is almost exclusively caused by ''P. falciparum'' infection and usually arises 6-14 days after infection.<ref name=Trampuz>{{cite journal | author = Trampuz A, Jereb M, Muzlovic I, Prabhu R | title = Clinical review: Severe malaria. | url=http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=12930555 | journal = Crit Care | volume = 7 | issue = 4 | pages = 315-23 | year = 2003 | id = PMID 12930555}}</ref> Consequences of severe malaria include [[coma]] and death if untreated—young children and pregnant women are especially vulnerable. [[Splenomegaly]] (enlarged spleen), severe [[headache]], cerebral [[ischemia]], [[hepatomegaly]] (enlarged liver), [[hypoglycemia]], and hemoglobinuria with [[renal failure]] may occur. Renal failure may cause [[blackwater fever]], where hemoglobin from lysed red blood cells leaks into the urine. Severe malaria can progress extremely rapidly and cause death within hours or days.<ref name=Trampuz/> In the most severe cases of the disease fatality rates can exceed 20%, even with intensive care and treatment.<ref>{{cite journal | author = Kain K, Harrington M, Tennyson S, Keystone J | title = Imported malaria: prospective analysis of problems in diagnosis and management. | journal = Clin Infect Dis | volume = 27 | issue = 1 | pages = 142-9 | year = 1998 | id = PMID 9675468}}</ref> In endemic areas, treatment is often less satisfactory and the overall fatality rate for all cases of malaria can be as high as one in ten.<ref>{{cite journal | author = Mockenhaupt F, Ehrhardt S, Burkhardt J, Bosomtwe S, Laryea S, Anemana S, Otchwemah R, Cramer J, Dietz E, Gellert S, Bienzle U | title = Manifestation and outcome of severe malaria in children in northern Ghana. | journal = Am J Trop Med Hyg | volume = 71 | issue = 2 | pages = 167-72 | year = 2004 | id = PMID 15306705}}</ref> Over the longer term, developmental impairments have been documented in children who have suffered episodes of severe malaria.<ref name="carter2005">{{cite journal | author=Carter JA, Ross AJ, Neville BG, Obiero E, Katana K, Mung'ala-Odera V, Lees JA, Newton CR | title=Developmental impairments following severe falciparum malaria in children | journal=Trop Med Int Health | year=2005 | volume=10 | pages=3-10 | id=PMID 15655008}}</ref> | ||
Revision as of 14:46, 14 June 2012
Malaria is a vector-borne infectious disease caused by protozoan parasites. It is widespread in tropical and subtropical regions, including parts of the Americas, Asia, and Africa. Each year, it causes disease in approximately 650 million people and kills between one and three million, most of them young children in Sub-Saharan Africa. Malaria is commonly associated with poverty, but is also a cause of poverty and a major hindrance to economic development.
Symptoms of malaria include fever, shivering, arthralgia (joint pain), vomiting, anemia caused by hemolysis, hemoglobinuria, and convulsions. There may be the feeling of tingling in the skin, particularly with malaria caused by P. falciparum. The classical symptom of malaria is cyclical occurrence of sudden coldness followed by rigor and then fever and sweating lasting four to six hours, occurring every two days in P. vivax and P. ovale infections, while every three for P. malariae.[1] P. falciparum can have recurrent fever every 36-48 hours or a less pronounced and almost continuous fever. For reasons that are poorly understood, but which may be related to high intracranial pressure, children with malaria frequently exhibit abnormal posturing, a sign indicating severe brain damage.[2] Malaria has been found to cause cognitive impairments, especially in children. It causes widespread anemia during a period of rapid brain development and also direct brain damage. This neurologic damage results from cerebral malaria to which children are more vulnerable.[3]
Chronic malaria is seen in both P. vivax and P. ovale, but not in P. falciparum. Here, the disease can relapse months or years after exposure, due to the presence of latent parasites in the liver. Describing a case of malaria as cured by observing the disappearance of parasites from the bloodstream can therefore be deceptive. The longest incubation period reported for a P. vivax infection is 30 years.[4] Approximately one in five of P. vivax malaria cases in temperate areas involve overwintering by hypnozoites (i.e., relapses begin the year after the mosquito bite).[8]
References
- ↑ Malaria life cycle & pathogenesis. Malaria in Armenia. Accessed October 31, 2006.
- ↑ Idro, R. "Decorticate, decerebrate and opisthotonic posturing and seizures in Kenyan children with cerebral malaria". Malaria Journal. 4 (57). PMID 16336645. Retrieved 2007-01-21. Unknown parameter
|coauthors=ignored (help) - ↑ Boivin, M.J., "Effects of early cerebral malaria on cognitive ability in Senegalese children," Journal of Developmental and Behavioral Pediatrics 23, no. 5 (October 2002): 353–64. Holding, P.A. and Snow, R.W., "Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence," American Journal of Tropical Medicine and Hygiene 64, suppl. nos. 1–2 (January–February 2001): 68–75.
- ↑ 4.0 4.1 4.2 Trampuz A, Jereb M, Muzlovic I, Prabhu R (2003). "Clinical review: Severe malaria". Crit Care. 7 (4): 315–23. PMID 12930555.
- ↑ Kain K, Harrington M, Tennyson S, Keystone J (1998). "Imported malaria: prospective analysis of problems in diagnosis and management". Clin Infect Dis. 27 (1): 142–9. PMID 9675468.
- ↑ Mockenhaupt F, Ehrhardt S, Burkhardt J, Bosomtwe S, Laryea S, Anemana S, Otchwemah R, Cramer J, Dietz E, Gellert S, Bienzle U (2004). "Manifestation and outcome of severe malaria in children in northern Ghana". Am J Trop Med Hyg. 71 (2): 167–72. PMID 15306705.
- ↑ Carter JA, Ross AJ, Neville BG, Obiero E, Katana K, Mung'ala-Odera V, Lees JA, Newton CR (2005). "Developmental impairments following severe falciparum malaria in children". Trop Med Int Health. 10: 3–10. PMID 15655008.
- ↑ Adak T, Sharma V, Orlov V (1998). "Studies on the Plasmodium vivax relapse pattern in Delhi, India". Am J Trop Med Hyg. 59 (1): 175–9. PMID 9684649.