Leishmaniasis pathophysiology
|
Leishmaniasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Leishmaniasis pathophysiology On the Web |
|
American Roentgen Ray Society Images of Leishmaniasis pathophysiology |
|
Risk calculators and risk factors for Leishmaniasis pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Leishmaniasis is spread by the bite of some types of phlebotomine sand flies. Sand flies become infected by biting an infected animal (for example, a rodent or dog) or person. Since sand flies do not make noise when they fly, people may not realize they are present. Sand flies are very small and may be hard to see; they are only about one-third the size of typical mosquitoes. Sand flies usually are most active in twilight, evening, and night-time hours (from dusk to dawn). Sand flies are less active during the hottest time of the day. However, they will bite if they are disturbed, such as when a person brushes up against the trunk of a tree where sand flies are resting. Rarely, leishmaniasis is spread from a pregnant woman to her baby. Leishmaniasis also can be spread by blood transfusions or contaminated needles.
Pathophysiology
 |
Leishmaniasis is caused by infection with the pathogen Leishmania. The genomes of three Leishmania species (L. major, L. infantum, and L. braziliensis) have been sequenced and this has provided much information about the biology of the parasite. For example, in Leishmania, protein-coding genes are understood to be organized as large polycistronic units in a head-to-head or tail-to-tail manner; RNA polymerase II transcribes long polycistronic messages in the absence of defined RNA pol II promoters, and Leishmania has unique features with respect to the regulation of gene expression in response to changes in the environment. The new knowledge from these studies may help identify new targets for urgently needed drugs and aid the development of vaccines.[1]
Life Cycle and Transmission
- Leishmaniasis is transmitted by the bite of female phlebotomine sandflies.
- The sandflies inject the infective stage, metacyclic promastigotes, during blood meals (1).
- Metacyclic promastigotes that reach the puncture wound are phagocytized by macrophages (2) and transform into amastigotes (3).
- Amastigotes multiply in infected cells and affect different tissues, depending in part on which Leishmania species is involved (4).
- These differing tissue specificities cause the differing clinical manifestations of the various forms of leishmaniasis. Sandflies become infected during blood meals on an infected host when they ingest macrophages infected with amastigotes (5,6).
- In the sandfly's midgut, the parasites differentiate into promastigotes (7), which multiply, differentiate into metacyclic promastigotes and migrate to the proboscis (8).
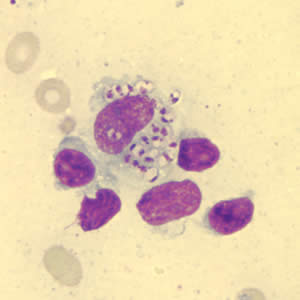
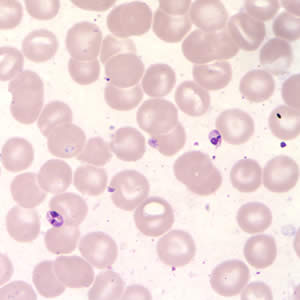
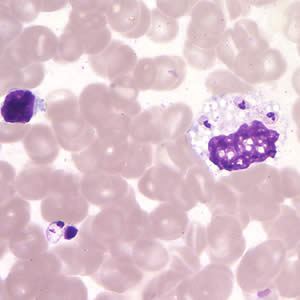
Microscopic Pathology
 |
 |
 |
 |
References
- ↑ Myler P; Fasel Nhirf;f). (2008). Leishmania: After The Genome. Caister Academic Press. isbn = 978-1-904455-28-8.
- ↑ 2.0 2.1 2.2 2.3 "CDC - DPDx - Laboratory Identification of Parasitic Diseases of Public Health Concern. Leishmaniasis".