Left ventriculography
| Resident Survival Guide |
|
Coronary Angiography | |
|
General Principles | |
|---|---|
|
Anatomy & Projection Angles | |
|
Normal Anatomy | |
|
Anatomic Variants | |
|
Projection Angles | |
|
Epicardial Flow & Myocardial Perfusion | |
|
Epicardial Flow | |
|
Myocardial Perfusion | |
|
Lesion Complexity | |
|
ACC/AHA Lesion-Specific Classification of the Primary Target Stenosis | |
|
Lesion Morphology | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
With the advancement of noninvasive imaging methods such as echocardiography, less emphasis has recently been placed on the ventriculogram as part of a cardiac catheterization. However, entry into the left ventricle with hemodynamic measurement and visualization of the left ventricle using contrast ventriculography remains an important aspect of a complete angiographic study.
In patients presenting acutely with ST elevation myocardial infarction, assessment of myocardial and valvular function with ventriculography may provide important prognostic information and may guide in part the management of the patient. In obese patients with difficult echocardiographic windows, ventriculography may provide diagnostic information that cannot be obtained from the echocardiogram.
Indications:
- Assessment of left ventricular function including left ventricular ejection fraction, wall motion abnormalities, ventricular size and mass
- Identification and assessment of mitral regurgitation
- Identification and assessment of ventricular septal defects
Contraindications:
- Decompensated heart failure
- Extreme elevation of LVEDP
- Critical aortic stenosis
- Left ventricular thrombus
- Iodinated contrast allergy
Complication:
- Ventricular arrythmias
- Embolization of air or thrombus
- Contrast related complications
- Decompensated heart failure
- Myocardial staining
Technique:
Crossing the Aortic Valve
- Crossing the aortic valve in patients without significant aortic stenosis is fairly straight-forward.
- Ventriculography is best performed with an angled pigtail catheter which avoids some of the pitfalls such as myocardial staining and catheter movement which can occur with an end hole catheter.
- The angled pigtail catheter does not allow the measurement of precise pressure gradients (part of the catheter may lie proximal and the other part distal to the stenosis or obstruction).
- The aortic valve may be difficult to cross with an angled pigtail catheter in patients with aortic stenosis.
Ventriculography in patients without aortic stenosis
- To cross the valve in patients without stenosis, the 0.35 wire is left in the catheter slightly back from the tip and the pigtail catheter is placed above the valve forming a ‘6’ above the valve and advanced until it prolapses above the valve. Once a loop is formed above the valve with the prolapsed catheter, it is pulled back and rotated slightly clockwise. As the catheter falls into the aortic root it is advanced. This maneuver will usually facilitate entry into the left ventricle. Sometimes, the body of the catheter will prolapse across the valve. If this happens, advancement of the 0.35 wire will usually prolapse the catheter into the ventricle. Having the patient take a breath advancement of the pigtail into the ventricle during systole will sometimes facilitate ventricular entry.
Ventriculography in patients with aortic stenosis
- In patients with aortic stenosis crossing the aortic valve may be more difficult due to the profile of the pigtail. Also, the 0.035 J-tipped wire often will not engage the stenosed orifice.
- In cases of suspected severe stenosis, crossing the aortic valve is best accomplished using a catheter able to be directed toward the ostium such as an Amplatz Left-1 or an Amplatz Right-2. In this situation the catheter is advances into the aortic root and an 0.035 or 0.038 wire with either a tight curve or straight wire is advanced through the aortic orifice.
- Setting up to cross the valve is almost as important as crossing the valve itself. Before attempting to cross with this system, cinematography of the calcified valve in both the RAO and LAO tomographic projections will often give the operator clues in the direction and angulation of the orifice.
- Once proceeding, the catheter is placed in the root and the wire is advanced forward. As the catheter rotates through the orifice the wire will prolapse in one of the cusp. Quarter turns of the catheter and close attention to the direction of the wire will often allow the wire to cross the valve. Once the valve is crossed, the catheter is advanced into the ventricle and hemodynamic measurements can be made.
- Crossing a stenosed aortic valve carries risk of embolization from both the valve and also from thrombus organization on the wire while attempts are made. Due to this fact, crossing the valve should be reserved for cases where noninvasive imaging of the valve has provided inconclusive results. Also, the patient should be administered heparin (5000 U) and attempts to cross the valve should be limited to 3 minutes before flushing the catheter.
Optimal Ventriculography
- Unfortunately, unless biplane angiography is available, ventriculography only provides a 2-dimensional projection of the ventricle and each image will not include all of the left ventricular segments.
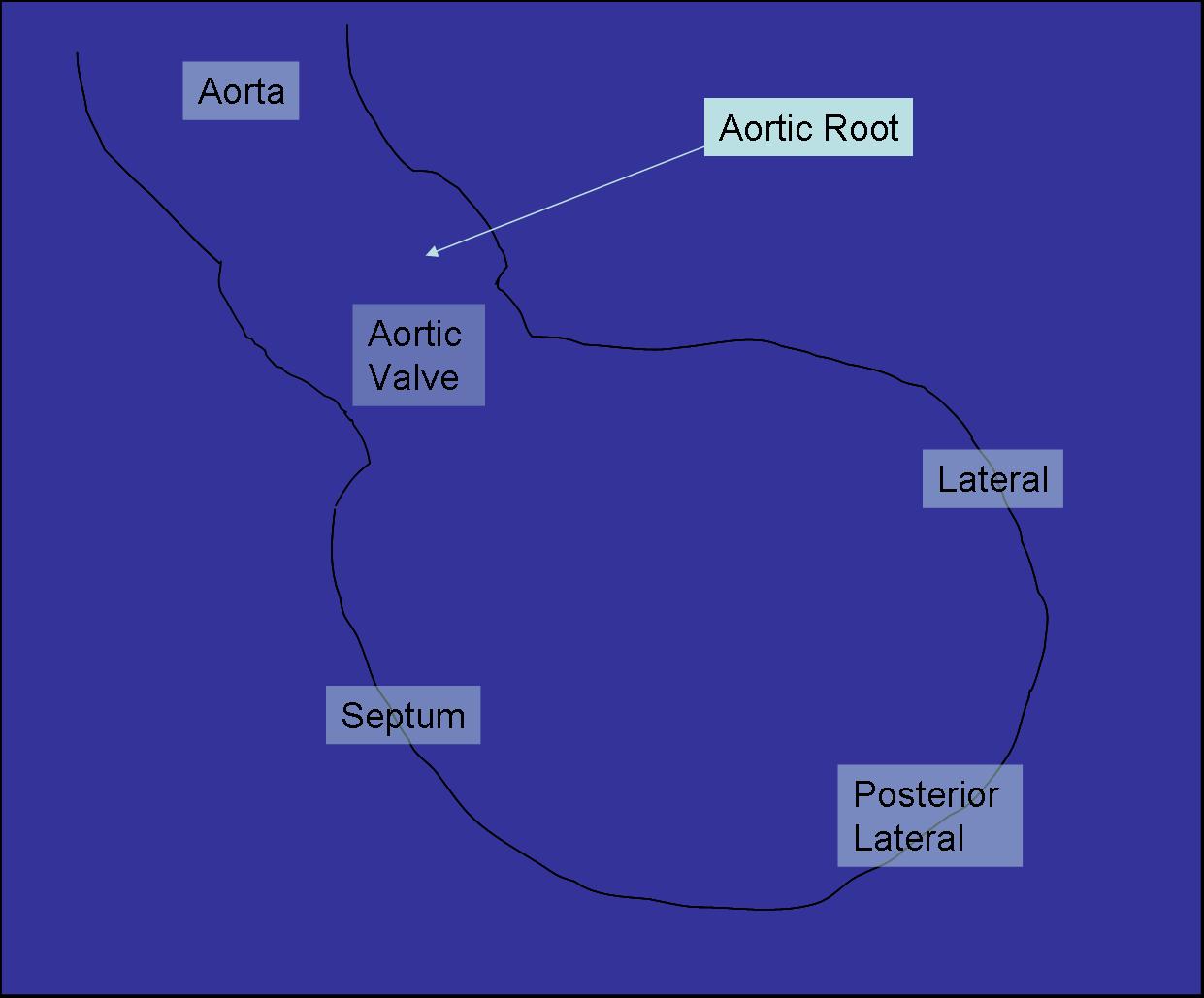
- The 2 standard views for ventriculography are the RAO (30o) which demonstrates the Anterior, Apical and Inferior ventricular walls.
- A LAO 60o LAO 20o Cranial view allows for better imaging of the lateral and septal ventricular walls.
- The latter views are particular useful in patients with lateral ischemia (especially circumflex ischemia), suspected VSD and mitral regurgitation.
- Once advanced into the left ventricle, the pigtail should be located in the mid ventricular cavity.
- Too superior or apical positioning of the catheter may lead to excessive ectopy. Ectopy may interfere with interpretation of wall motion abnormalities.
- Too inferior of a position may interfere with the mitral apparatus leading to an overestimation of mitral regurgitation.
- Difficult manipulation or visual tanglement of the catheter may indicate involvement with the apparatus.
- Reposition of the catheter usually requires countering and pulling the catheter then advancing once the tip is free. A test injection of 5 cc of contrast medium may help to confirm correct positioning of the catheter and prevent wasted contrast from a poor ventriculogram.
- All hemodynamic measurements should be performed prior to ventriculography.
- Also, ventriculography should be avoided in patients with decompensated heart failure, severe aortic stenosis and ventricular thrombus. * If digital subtraction is available, a hand injection may be attempted with the patient holding their breath. This should only be used as a quick estimation as important pathology such as a VSD may be missed due to incomplete opacification with this method.
Settings
- Optimal ventriculography is performed using a power injector to fill the left ventricular cavity.
- Adjustable settings on the power injector include pressure and flow rates, volume, rate of pressure rise.
- Each patient will have slight variation in settings based on ventricular size, sex, and catheter type and size.
- Generally, 10-15 ml/sec for 30-40 cc will be sufficient to image a normal ventricle and heart rate.
- A rate of rise of 0.4 cc/sec in order to prevent lunging of the catheter leading to increased ectopy.
- The pressure rate settings is typically 600 psi for a 6 Fr, 900 psi for a 5 Fr system and 1200 psi for a 4Fr system.
- Careful attention is required to remove air from the injector system prior to use to prevent catastrophic embolism during ventriculography.
Manipulation Technique
The operator should keep the left hand on the catheter during injection to change the position as required during the procedure. If the catheter is too far in the apex, pullback of 1-2 cm will usually reposition the catheter for several beats to obtain useful information.
Quantification of Left Ventricular Function
- Depending on the tomographic projection, specific ventricular wall motion abnormalities may be identified.
- Hypokinesia refers to decreased but not absent motion of a ventricular segment.
- Akinesia refers to a complete absence of wall motion.
- Dyskinesia refers to a paradoxical expansion or wall motion usually due to tethering from the adjacent segments.
- The ejection fraction by ventriculography will usually be slightly higher than the corresponding echocardiographic measurments.
 |
{{#ev:googlevideo|986254730861624461&hl=en}} |
 |
{{#ev:googlevideo|-8044287213933915863&hl=en}} |
Quantification of Mitral Regurgitation:
Both the RAO and LAO/Cranial projections can be used to identify significant mitral regurgitation. Grading the amount of regurgitation is based on the amount of opacification of the atrium compared to the ventricular opacification, atrial size and the number of cycles required for maximal opacification. Elevation of left atrial pressure in acute regurgitation and dilation of the left atrium from chronic regurgitation can both interfere with the use of this grading system.
Grade 1
Brief and incomplete atrial opacification over several cycles. Clears rapidly. No atrial enlargement.
{{#ev:googlevideo|8237703398893439012&hl=en}}
{{#ev:googlevideo|-8044287213933915863&hl=en}}
Grade 2
Moderate opacification of the atria with each cycle. Never greater than LV opacification. No significant LA enlargement.
{{#ev:googlevideo|-3259427927007644054&hl=en}}
Grade 3
opacification equal to ventricular opacification. Delayed clearing of atria over several cycles. Significant enlargement of the LA.
{{#ev:googlevideo|-8295323872088090226&hl=en}}
{{#ev:googlevideo|2584010676245016071&hl=en}}
Grade 4
Atrial Opacification immediate and greater than that of the ventricle. Severe enlagement of the LA. Opacification of the pulmonary veins.
{{#ev:googlevideo|-5531059825466069834&hl=en}}
{{#ev:googlevideo|7527640933077169571&hl=en}}
Left and Right Ventriculography (MSCT, Beating Heart)
{{#ev:youtube|Nf7vsj0H2Mw}}